Last Updated on November 20, 2025 by Ugurkan Demir

Bleeding disorders are conditions where the body can’t stop bleeding properly. This makes it hard for the body to clot blood. As a result, people with these disorders might bleed too much or for too long.Discover bleeding disorders list, inherited and hemorrhagic types, and symptoms.
These hemostatic conditions mess up the body’s clotting process. This can lead to health problems. People with these conditions might bleed on their own or take a long time to stop bleeding after an injury.
Liv Hospital is dedicated to giving top-notch care to those with these conditions. They use the latest medical standards to help patients.
Key Takeaways
- Knowing about different bleeding disorders is key for the right treatment.
- Hemorrhagic disorders can be passed down or happen later in life. They affect people of all ages.
- Good care and management can really improve life for those affected.
- Liv Hospital provides special care for bleeding disorder patients.
- Getting diagnosed and treated early can stop serious problems.
What Are Bleeding Disorders and How Do They Affect the Body?
Bleeding disorders happen when blood clotting doesn’t work right. They are also known as hemorrhagic conditions. These disorders affect how blood clots in the body.
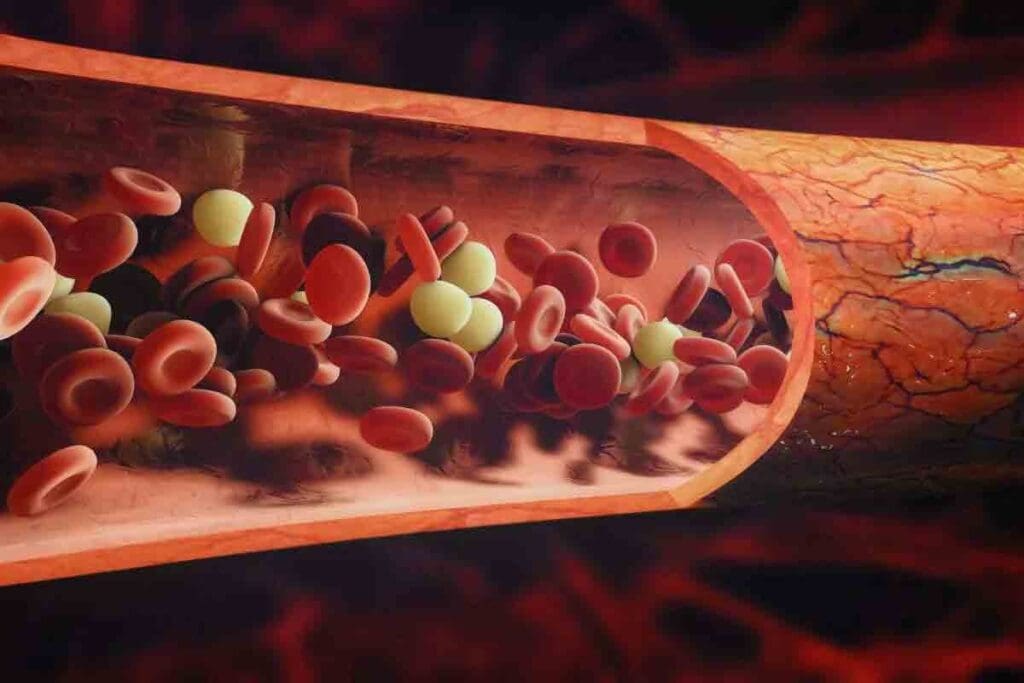
The Normal Blood Clotting Process
The blood clotting process is complex. It involves platelets and clotting factors. When a blood vessel gets hurt, platelets stick to it, forming a plug.
At the same time, clotting factors start a series of chemical reactions. This leads to the creation of fibrin, which makes the plug stronger. This forms a stable clot.
A hematologist, says, “The blood clotting process is a finely tuned mechanism. It involves the coordination of multiple cell types and proteins.” This process is key to stopping bleeding when a vessel is damaged.
When Clotting Goes Wrong
Bleeding disorders happen when the blood clotting process goes wrong. This can be due to low platelet numbers or faulty platelet function. It can also be because of missing or deficient clotting factors.
People with bleeding disorders may bleed a lot after injuries, surgeries, or even without any reason. According to the
“National Hemophilia Foundation, bleeding disorders can significantly impact an individual’s quality of life. They require careful management and treatment to prevent complications.”
Common problems include frequent nosebleeds, easy bruising, and heavy or long menstrual periods. In severe cases, bleeding can get into joints or muscles. This can cause pain and swelling.
It’s important to understand the causes and signs of bleeding disorders. This helps doctors diagnose and treat them. By recognizing symptoms, healthcare providers can start the right tests and treatment plans.
Comprehensive Bleeding Disorders List: Understanding the 7 Main Types

Bleeding disorders make it hard for blood to clot. They can be inherited or caused by other factors. Knowing the different types is key for the right treatment.
Inherited vs. Acquired Hemorrhagic Conditions
Inherited bleeding disorders come from genes. Examples are Hemophilia A and B, and Von Willebrand Disease. Acquired disorders happen later in life due to various reasons.
Inherited Bleeding Disorders: These are caused by genetic changes. They affect proteins needed for blood clotting. The most common include:
- Von Willebrand Disease
- Hemophilia A (Factor VIII deficiency)
- Hemophilia B (Factor IX deficiency)
- Rare factor deficiencies (e.g., Factor I, II, V, VII, X, XI, XII, XIII deficiencies)
- Platelet function disorders (e.g., Glanzmann Thrombasthenia, Bernard-Soulier Syndrome)
Classification of Bleeding Disorders
Bleeding disorders are grouped by their cause. The main groups are:
| Category | Description | Examples |
| Coagulation Factor Deficiencies | Proteins needed for clotting are missing | Hemophilia A, Hemophilia B, Rare factor deficiencies |
| Platelet Disorders | Problems with platelet count or function | Glanzmann Thrombasthenia, Bernard-Soulier Syndrome |
| Fibrinolytic Disorders | Conditions that affect blood clot breakdown | Certain cases of excessive bleeding due to enhanced fibrinolysis |
Knowing about bleeding disorders helps doctors treat them better. By understanding the causes, doctors can give better care. This improves patient outcomes.
Von Willebrand Disease: The Most Common Bleeding Disorder
Von Willebrand disease is the most common bleeding disorder. It needs a deep understanding for proper management and treatment. This condition is caused by a problem with von Willebrand factor (VWF), a key protein for blood clotting.
It affects both men and women, but symptoms can differ due to hormones and genetics. Healthcare providers must grasp the details of von Willebrand disease to diagnose and treat it well.
Types of Von Willebrand Disease
Von Willebrand disease is divided into three types: Type 1, Type 2, and Type 3. Each type has a different level of VWF deficiency, affecting severity.
- Type 1: The mildest form, with a partial VWF deficiency.
- Type 2: Includes subtypes (2A, 2B, 2M, and 2N), with qualitative VWF defects.
- Type 3: The most severe, with no VWF, causing serious bleeding issues.
Symptoms, Diagnosis, and Treatment
Symptoms of von Willebrand disease vary from mild to severe. They include easy bruising, frequent nosebleeds, and heavy menstrual bleeding in women. Diagnosis requires lab tests to check VWF levels and activity.
| Symptom | Description | Diagnostic Test |
| Easy Bruising | Frequent bruising without apparent cause | VWF Antigen Test |
| Nosebleeds | Recurring nosebleeds | Bleeding Time Test |
| Heavy Menstrual Bleeding | Prolonged or excessive menstrual bleeding | VWF Activity Test |
Treatment depends on the disease type and severity. Options include desmopressin, VWF replacement therapies, and bleeding prevention medications.
Managing von Willebrand disease requires a personalized approach. Healthcare providers must consider each person’s specific situation and needs. By knowing the types, symptoms, and treatments, they can offer tailored care.
Hemophilia A: Factor VIII Deficiency
Hemophilia A, also known as factor VIII deficiency, is a genetic disorder. It makes it hard for the body to clot blood. This leads to long-lasting bleeding, which can be dangerous if not treated right.
Genetic Inheritance Pattern
Hemophilia A is an X-linked recessive disorder. This means the gene for this condition is on the X chromosome. It mainly affects males, as they have only one X chromosome.
Females are usually carriers unless they have two defective X chromosomes, which is rare. The F8 gene, which makes factor VIII, has mutations in Hemophilia A. These mutations cause less or no factor VIII, leading to bleeding problems.
Severity Levels and Clinical Manifestations
The severity of Hemophilia A depends on how much factor VIII is in the blood. There are three main levels:
- Mild Hemophilia A: Factor VIII activity is between 5% and 40% of normal. Bleeding happens with trauma or surgery.
- Moderate Hemophilia A: Factor VIII activity is between 1% and 5% of normal. Bleeding can happen with minor trauma.
- Severe Hemophilia A: Factor VIII activity is less than 1% of normal. Spontaneous bleeding is common, often without reason.
Clinical signs include long bleeding after injuries, surgeries, or dental work. In severe cases, bleeding into joints or muscles can happen. This can cause chronic joint disease and disability.
Modern Treatment Approaches
Modern treatment for Hemophilia A involves replacing factor VIII through factor replacement therapy. This can be for bleeding episodes or to prevent them.
Prophylactic treatment is now common for severe Hemophilia A. It aims to keep factor VIII levels high. This makes severe hemophilia milder. Newer treatments, like extended half-life factor VIII products and emicizumab, have improved patient outcomes.
Hemophilia B: Christmas Disease
Hemophilia B is a bleeding disorder caused by a lack of clotting factor IX. It leads to prolonged bleeding, which can happen without any reason or because of an injury.
Differences from Hemophilia A
Hemophilia A and B are both bleeding disorders linked to the X chromosome. But they affect different clotting factors. Hemophilia A lacks factor VIII, while Hemophilia B lacks factor IX. The World Federation of Hemophilia says Hemophilia B is less common, making up about 15-20% of cases worldwide.
The symptoms of both conditions are similar, making it hard to diagnose just by looking at symptoms. But, the treatment is different because of the different clotting factors involved.
Diagnosis and Management
To diagnose Hemophilia B, doctors use a mix of clinical checks, family history, and lab tests. These include tests to measure factor IX levels. Treatment usually involves giving factor IX concentrates to help with clotting.
“Prophylactic treatment with factor IX can significantly reduce the frequency of bleeding episodes and improve the quality of life for individuals with Hemophilia B,” experts say.
Doctors can give treatment when needed to stop bleeding or regularly to prevent it. The choice depends on how severe the condition is, what the patient prefers, and what the guidelines say.
Living with Hemophilia B
Managing Hemophilia B means a detailed plan that includes regular factor IX infusions and watching for bleeding. It’s also important to stay active and eat well to stay healthy.
Support from patient groups and treatment centers is key for those with Hemophilia B. As one patient said, “Getting the right care and support has really helped me live a normal life with Hemophilia B.”
Rare Factor Deficiencies: Beyond Hemophilia
Rare factor deficiencies are a wide range of bleeding disorders. They go beyond the well-known hemophilia A and B. These deficiencies affect different clotting factors needed for blood to clot.
The clotting process involves many factors. When these factors are low, it can cause serious bleeding. It’s important to understand these rare conditions for proper diagnosis and treatment.
Factor I (Fibrinogen) and Factor II (Prothrombin) Deficiencies
Factor I deficiency, or fibrinogen deficiency, is a rare disorder. It’s caused by low fibrinogen levels, a key protein in clotting. Symptoms can be mild or severe, including easy bruising and prolonged bleeding.
Factor II deficiency, or prothrombin deficiency, is another rare condition. It’s caused by low prothrombin levels, a vital clotting factor. This can lead to severe bleeding, including bleeding in the brain.
| Condition | Symptoms | Clotting Factor Involved |
| Fibrinogen Deficiency | Bruising, nosebleeds, prolonged bleeding | Fibrinogen (Factor I) |
| Prothrombin Deficiency | Severe bleeding episodes, intracranial hemorrhage | Prothrombin (Factor II) |
Factor V, VII, X, XI, XII, and XIII Deficiencies
Other rare deficiencies include Factors V, VII, X, XI, XII, and XIII. Each presents unique challenges.
Factor V deficiency can cause significant bleeding after injuries or surgery. Factor VII deficiency often leads to bleeding in the skin and mucous membranes. Factor X deficiency is very severe, causing bleeding similar to hemophilia.
Factor XI deficiency, also known as hemophilia C, causes bleeding after surgery or trauma. Factor XII deficiency is usually without symptoms but can lead to blood clots in some cases. Factor XIII deficiency makes clots unstable, leading to frequent bleeding and poor wound healing.
| Factor Deficiency | Common Symptoms |
| Factor V | Bleeding after trauma or surgery |
| Factor VII | Mucocutaneous bleeding |
| Factor X | Joint and muscle bleeding |
| Factor XI | Bleeding after surgery or trauma |
| Factor XII | Often asymptomatic, sometimes thrombosis |
| Factor XIII | Recurrent bleeding, poor wound healing |
Platelet Function Disorders: The Cellular Component
Platelet function disorders are a group of bleeding conditions. They happen when platelets can’t stick together properly. This makes it hard for the body to stop bleeding.
Glanzmann Thrombasthenia
Glanzmann thrombasthenia is a rare bleeding disorder. It makes platelets unable to stick together. This leads to long bleeding times and a higher risk of bleeding.
Symptoms can vary from mild to severe. They include frequent nosebleeds, easy bruising, and long bleeding after injuries or surgery.
To diagnose, tests like platelet aggregometry and flow cytometry are used. These tests check if platelets have the right proteins. Treatment may include platelet transfusions and medicines to stop bleeding.
Bernard-Soulier Syndrome and Other Platelet Disorders
Bernard-Soulier syndrome is a rare bleeding disorder. It’s caused by a problem with the glycoprotein Ib-IX-V complex on platelets. This complex helps platelets stick to von Willebrand factor at injury sites.
It’s characterized by giant platelets and low platelet count. This leads to bleeding problems.
- Bernard-Soulier Syndrome: Characterized by giant platelets and thrombocytopenia.
- Other Platelet Disorders: Include conditions like platelet storage pool disease and defects in platelet signal transduction.
Managing these conditions often involves supportive care. This includes platelet transfusions during bleeding or before surgery. It also includes steps to prevent bleeding.
“The management of platelet disorders requires a complete approach. This includes diagnosis, treatment, and preventive strategies tailored to the specific condition and patient needs.”
Diagnosing Hemorrhagic Conditions: From Symptoms to Confirmation
Diagnosing hemorrhagic conditions starts with a detailed clinical assessment. Bleeding disorders show up in different ways. It’s key to carefully check symptoms and run the right tests.
Initial Evaluation and Screening Tests
The first step is a detailed medical history and physical exam. Doctors look for signs like ecchymoses, petechiae, or long bleeding from cuts.
Screening tests help spot bleeding disorders. These tests include:
- Complete Blood Count (CBC) to check platelet count and blood cell health.
- Coagulation panel, with tests like prothrombin time (PT) and activated partial thromboplastin time (aPTT), to see how blood clots.
Advanced Diagnostic Procedures
If screening tests suggest a bleeding disorder, more tests are needed. These can be:
- Specific factor assays to measure clotting factor levels.
- Molecular genetic testing to find genetic mutations in inherited disorders.
- Platelet function tests to check platelet aggregation and find issues like Glanzmann thrombasthenia.
The table below shows how to diagnose bleeding disorders:
| Diagnostic Step | Purpose | Tests Involved |
| Initial Evaluation | Assess symptoms and medical history | Medical history, physical examination |
| Screening Tests | Identify possible bleeding disorders | CBC, coagulation panel (PT, aPTT) |
| Advanced Diagnostic Procedures | Confirm specific bleeding disorders | Specific factor assays, molecular genetic testing, platelet function tests |
Getting the right diagnosis is crucial for managing bleeding disorders well. A systematic approach helps doctors find the cause and plan treatment.
Treatment Strategies for Inherited Bleeding Disorders
Medical science has made big strides in treating inherited bleeding disorders. Now, patients have more effective ways to manage their conditions. The right treatment depends on the disorder, its severity, and the patient’s health.
Factor Replacement Therapy
Factor replacement therapy is key for treating hemophilia A and B. It replaces missing or faulty clotting factors with man-made or plasma-derived ones.
Benefits of Factor Replacement Therapy:
- It stops and treats bleeding episodes well
- It can be used to prevent bleeding
- There are different types, including ones that last longer
| Clotting Factor | Indication | Administration Frequency |
| Factor VIII | Hemophilia A | 2-3 times a week (prophylaxis) |
| Factor IX | Hemophilia B | 1-2 times a week (prophylaxis) |
Non-Replacement Therapies and Medications
New treatments are being developed to help with bleeding disorders. These options don’t replace clotting factors but help with stopping bleeding.
Examples of Non-Replacement Therapies:
- Desmopressin for mild hemophilia A and some von Willebrand disease
- Antifibrinolytics to keep clots stable and prevent bleeding
- Emicizumab, a drug that acts like factor VIII
Gene Therapy and Future Directions
Gene therapy is a new hope for treating bleeding disorders. It aims to fix the genetic problem by adding a healthy gene to cells. This could offer a lasting cure.
Potential Benefits of Gene Therapy:
- Less frequent treatment needed
- Improved life quality
- Stable clotting factor levels
Gene therapy is in early trials for bleeding disorders. Early results look good, and it’s expected to play a big role in treatment soon.
Living with Hereditary Blood Disorders: Practical Considerations
Living with a hereditary blood disorder can be tough, but it’s possible to live an active life. It takes a mix of daily care, preventive steps, and support to manage these conditions well.
Daily Management and Preventive Measures
Managing hereditary blood disorders daily means using medicine, making lifestyle changes, and keeping an eye on your health. Factor replacement therapy is a key treatment for conditions like hemophilia A and B. It helps prevent or treat bleeding by adding the missing clotting factor.
It’s also important to take steps to prevent bleeding. Avoid activities that could cause injuries, like contact sports. Use protective gear when doing things that might be risky.
| Preventive Measure | Description | Benefit |
| Avoiding Contact Sports | Reducing participation in activities that could lead to physical trauma. | Decreases the risk of bleeding episodes. |
| Using Protective Gear | Utilizing gear like helmets and knee pads during potentially hazardous activities. | Minimizes the risk of injury and subsequent bleeding. |
| Regular Monitoring | Frequent check-ups with healthcare providers to monitor the condition. | Allows for early detection and management of possible issues. |
Support Resources and Patient Communities
Living with a hereditary blood disorder can feel lonely, but there’s help out there. Patient advocacy groups offer important info, emotional support, and connections with others who get it.
Online forums and local groups are great places to share your story, ask questions, and get advice from people who face similar challenges.
By using these resources and being proactive, people with hereditary blood disorders can enhance their life quality. They can live a fulfilling life.
Conclusion
Bleeding disorders, like inherited and hemorrhagic ones, are tough to deal with. We’ve looked at different types, symptoms, how to find out you have one, and ways to treat it.
Managing bleeding disorders well is key to a better life. Knowing how blood clots normally and how it fails in these disorders helps a lot.
Knowing about hemorrhagic disorders and managing them well can lower the risk of serious problems. New treatments like factor replacement and gene therapy give hope to those with these conditions.
By staying informed and working with doctors, people with bleeding disorders can live full lives. More research and learning are needed to help those with these conditions.
FAQ
What is a bleeding disorder?
A bleeding disorder makes it hard for the body to stop bleeding. This happens because it can’t clot blood right.
What are the main types of bleeding disorders?
There are many bleeding disorders. Some are inherited, like von Willebrand disease and hemophilia. Others are not passed down in families.
What is von Willebrand disease?
Von Willebrand disease is the most common. It’s caused by a problem with the von Willebrand factor. This factor is key for blood to clot.
How is hemophilia A different from hemophilia B?
Hemophilia A is when there’s not enough factor VIII. Hemophilia B is when there’s not enough factor IX. Both affect clotting, but differently.
What are rare factor deficiencies?
Rare factor deficiencies happen when there’s not enough of other clotting factors. These include factors I, II, V, VII, X, XI, XII, or XIII.
How are bleeding disorders diagnosed?
Doctors use many ways to find bleeding disorders. They look at your medical history and do tests. They might also do clotting factor assays and genetic tests.
What are the treatment options for bleeding disorders?
There are several ways to treat bleeding disorders. Factor replacement therapy is one. There are also non-replacement therapies and medicines. Gene therapy is being researched too.
How can I manage a bleeding disorder on a daily basis?
To manage a bleeding disorder, take steps to avoid injuries. Take your medicines as told. Know the signs of bleeding and get help when needed.
Are there support resources available for people with bleeding disorders?
Yes, there are many resources. You can find patient communities, online forums, and organizations. They offer education, support, and advocacy.
Can bleeding disorders be cured?
Some bleeding disorders can be managed well with treatment. But, a cure isn’t always possible. Yet, research is ongoing, and new treatments like gene therapy are promising.
What is the most common blood disease?
Von Willebrand disease is the most common. It makes it hard for blood to clot properly.
What is a disease that prevents blood from clotting?
Diseases like hemophilia A or B, von Willebrand disease, or rare factor deficiencies prevent blood from clotting.
What are haemostatic disorders?
Haemostatic disorders affect the body’s ability to balance bleeding and clotting. They include bleeding disorders and conditions that cause too much clotting.
Reference
- National Heart, Lung, and Blood Institute. (2023, August 3). Bleeding disorders: Types. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/health/bleeding-disorders/types





