
Childhood leukemia is the most common cancer in kids, making up about 31 percent of cases in those under 15. Most cases happen because of random genetic mutations in blood cells. But, 10 to 21 percent are linked to inherited genetic changes. At Liv Hospital, we focus on understanding the complex causes of childhood leukemia, including genetic and environmental factors.
We look into the risks, inheritance, and ways to prevent it. This helps us give families the care and support they need. Knowing the causes is key to finding effective ways to prevent it.
Key Takeaways
- Childhood leukemia accounts for about 31% of cancers in children under 15.
- Random genetic mutations cause most childhood leukemia cases.
- Inherited genetic changes are associated with 10 to 21% of cases.
- Environmental factors may also play a role in childhood leukemia.
- Understanding causes is key to prevention strategies.
Understanding Childhood Leukemia: The Basics

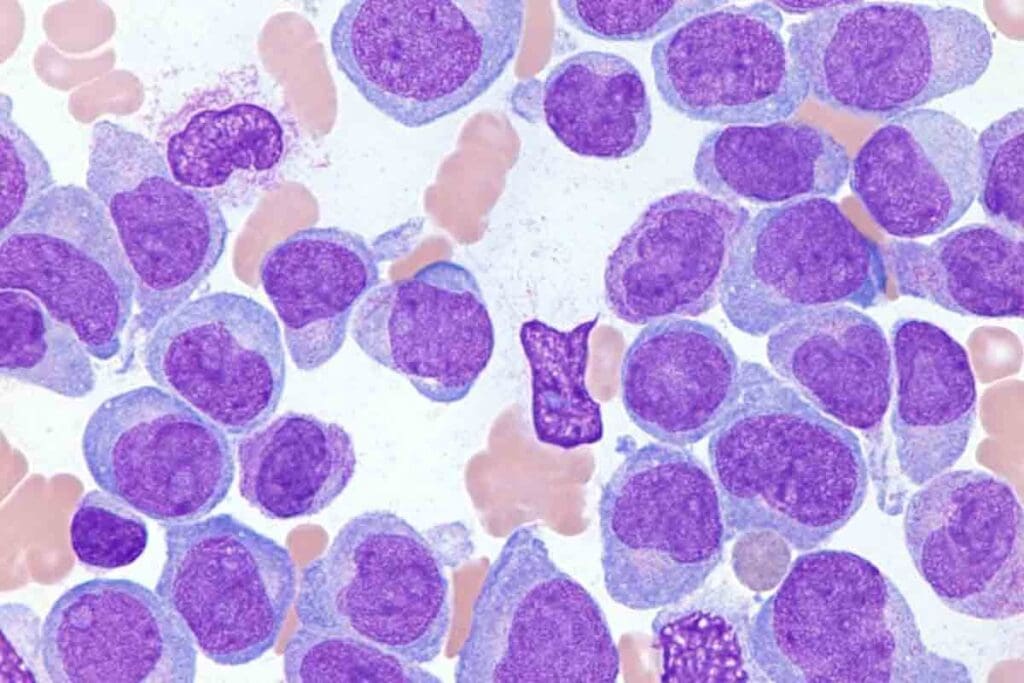
Leukemia in children is a cancer that starts in the blood and bone marrow. It’s important to know what it is, its types, and how common it is.
What Is Childhood Leukemia?
Childhood leukemia is a cancer that affects kids’ blood and bone marrow. It happens when the bone marrow makes bad white blood cells. These bad cells take over, making it hard for the body to fight off infections.
The National Cancer Institute says it’s the most common cancer in kids. It makes up about 30% of all childhood cancers.
Types of Childhood Leukemia
Childhood leukemia comes in two main types: acute and chronic. Acute leukemia grows fast and needs quick treatment. Chronic leukemia grows slowly over time.
- Acute Lymphoblastic Leukemia (ALL): This is the most common type, making up 80% of childhood leukemia cases.
- Acute Myeloid Leukemia (AML): AML is less common but can grow fast if not treated quickly.
- Chronic Lymphocytic Leukemia (CLL) and Chronic Myeloid Leukemia (CML): These are rare in kids and more common in adults.
Prevalence and Statistics
Childhood leukemia is a big health issue worldwide. The most cases happen between 2 and 5 years old.
| Age Group | Incidence Rate per Million Children |
| 0-4 years | 80-90 |
| 5-9 years | 40-50 |
| 10-14 years | 30-40 |
Knowing these stats and types helps parents and caregivers spot signs early. This can lead to quicker diagnosis and treatment.
The Genetic Basis of Childhood Leukemia
Understanding the genetic basis of childhood leukemia is key to better treatments and outcomes. We’ll look at how genetic mutations lead to this disease.
How Blood Cells Develop and Mutate
Blood cells start from stem cells in the bone marrow. This process, called hematopoiesis, can lead to genetic mutations. These mutations can cause abnormal cell growth and leukemia. Genetic alterations in genes that control cell growth can lead to uncontrolled cell growth.
The creation of blood cells involves many genetic and environmental factors. Mutations in genes for DNA repair, cell cycle, and apoptosis can lead to leukemia.
Somatic vs. Germline Mutations
Leukemia-causing mutations can be somatic or germline. Somatic mutations happen in non-reproductive cells and aren’t passed on. Germline mutations are in reproductive cells and can be inherited. Somatic mutations are more common in childhood leukemia, but germline mutations increase the risk.
It’s important to know the difference between these mutations to understand leukemia’s causes and for genetic counseling.
Common Genetic Alterations in Childhood Leukemia
Childhood leukemia often involves specific genetic changes. These include mutations in MLL, ETV6, and RUNX1 genes. Chromosomal translocations, like the ETV6-RUNX1 fusion, are common in B-cell ALL, the most common childhood leukemia.
Knowing these genetic changes helps in diagnosing and treating leukemia. We’re constantly researching to improve treatments and care for patients.
Is Childhood Leukemia Genetic? Examining Hereditary Factors
Most childhood leukemia cases aren’t passed down from parents. Yet, research shows genetic factors are key. We’ll look at inherited genetic changes, how common they are, and how to tell them apart from other mutations.
The Role of Inherited Genetic Changes
Inherited genetic changes can make kids more likely to get leukemia. This is because they affect how blood cells grow and work. For example, Down syndrome increases leukemia risk. This is because of mutations in genes important for cell growth.
Children with Down syndrome face a higher risk of AML and ALL. The genetic changes in Down syndrome cause blood cells to grow too much. This raises the chance of leukemia.
Percentage of Cases with Genetic Predisposition
Research shows a small part of childhood leukemia is linked to inherited genetic syndromes. It’s thought that 5-10% of cases have a genetic predisposition.
- Genetic syndromes like Down syndrome, Li-Fraumeni syndrome, and bone marrow failure syndromes raise the risk.
- Having a family history of leukemia or other cancers is also a risk factor.
- Some genetic mutations can be passed down, making kids more likely to get leukemia.
Distinguishing Between Inherited and Acquired Mutations
It’s important to know if a child’s leukemia is inherited or acquired. Inherited mutations are in germline cells and can be passed on. Acquired mutations happen during a child’s life, often due to environmental factors or DNA errors.
Genetic testing can tell if a child’s leukemia is due to an inherited mutation. Knowing this helps in giving the right care and understanding the risk to other family members.
Genetic Syndromes Associated with Increased Leukemia Risk
Certain genetic syndromes raise the risk of leukemia in kids. These conditions have genetic mutations that make people more likely to get cancer, including leukemia.
Down Syndrome and Leukemia Risk
Children with Down syndrome face a higher risk of leukemia. The National Cancer Institute says this risk is much higher in kids under 5. Down syndrome increases the risk of acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML).
A study in the Journal of Clinical Oncology found kids with Down syndrome are 20 times more likely to get ALL. They are 150 times more likely to get AML than kids without Down syndrome.
Li-Fraumeni Syndrome
Li-Fraumeni syndrome is a rare genetic disorder. It greatly increases the risk of several cancers, including leukemia. This syndrome is caused by inherited mutations in the TP53 tumor suppressor gene.
“Li-Fraumeni syndrome is characterized by a high risk of early-onset cancers, including leukemia, due to germline mutations in the TP53 gene.”
Natalie S. Cooper et al., Journal of Clinical Oncology
Bone Marrow Failure Syndromes
Bone marrow failure syndromes, like Fanconi anemia and Dyskeratosis congenita, affect the bone marrow’s ability to make blood cells. These conditions raise the risk of leukemia because of genetic instability and poor DNA repair.
| Syndrome | Leukemia Risk | Key Features |
| Down Syndrome | Increased risk of ALL and AML | Chromosomal abnormality, developmental delays |
| Li-Fraumeni Syndrome | High risk of various cancers, including leukemia | TP53 gene mutation, early-onset cancers |
| Fanconi Anemia | Increased risk of AML | Bone marrow failure, congenital abnormalities |
Other Genetic Conditions Linked to Leukemia
Other genetic conditions, like Noonan syndrome and ataxia-telangiectasia, also increase leukemia risk. These conditions often have genetic mutations that affect cell growth and DNA repair.
It’s important to know about genetic syndromes linked to leukemia risk. We suggest regular monitoring and screening for leukemia in kids with these syndromes.
Family History and Leukemia: Does Leukemia Run in Families?
Leukemia in families is a complex issue. It involves genetics and environmental factors. We look into how family history affects leukemia risk and the genetic links involved.
Sibling Risk Factors
Having a sibling with leukemia slightly raises a child’s risk. The risk is higher for twins, but it’s low overall.
Here are some key statistics:
| Family History | Relative Risk | Absolute Risk |
| No family history | 1.0 | 0.02% |
| Sibling with leukemia | 2.0-4.0 | 0.04%-0.08% |
| Identical twin with leukemia | Higher | Up to 25% in some studies |
The Unique Case of Identical Twins
Identical twins share the same genes. If one gets leukemia, the other’s risk is much higher. This is true, even in infants.
Multi-Generational Patterns
Leukemia sometimes runs in families for generations. But these cases are rare. A family history might lead to looking into genetic risks.
When to Consider Genetic Counseling
Families with leukemia history should think about genetic counseling. Counselors can explain genetic testing risks and benefits. They help families understand their situation.
For genetic counseling, families should:
- Know their cancer and leukemia history.
- Talk about genetic factors in leukemia.
- Learn about genetic testing options and what they mean.
Understanding family history in leukemia helps families make health decisions. They can lower their risk with early detection and prevention.
Environmental Factors and Childhood Leukemia Development
Childhood leukemia is shaped by genetics and the environment. We’ve covered genetics before. Now, let’s look at how the environment can affect leukemia risk.
Prenatal and Early Life Exposures
Exposure to the environment before and after birth is key. What a mother is exposed to can affect her child’s risk of leukemia.
Research shows that certain chemicals and infections in pregnancy might increase leukemia risk. Knowing this helps us guide pregnant women to avoid harmful substances.
Radiation Exposure
Radiation is a known risk for leukemia. High doses, like from nuclear accidents, can raise a child’s risk.
There’s strong evidence that radiation increases leukemia risk. So, we must limit radiation, even in medical tests, to protect kids.
Chemical Exposures
Some chemicals, like benzene, are linked to leukemia. Benzene is in gasoline and used in many industries.
It’s vital to reduce chemical exposure. Rules and safety gear can help keep people away from harmful chemicals.
Infections and Immune System Development
Infections and the immune system’s growth in early life matter. The “hygiene hypothesis” suggests a lack of infections might raise leukemia risk.
Studying infections and the immune system’s role in leukemia is complex. But, it shows the importance of some infections in early life for a strong immune system.
Infant Leukemia: Unique Causes and Considerations
Infant leukemia is a complex condition. It involves genetic mutations, maternal exposures, and in-utero development. This type of leukemia is diagnosed in the first year of life. It has its own set of genetic and environmental factors.
In-Utero Origins of Infant Leukemia
Some infant leukemia cases start in the womb. Genetic mutations happen during fetal development. These can come from inherited genes or environmental exposures during pregnancy.
In-utero origins mean the leukemia can begin before birth. This shows how important prenatal factors are. Studies on identical twins with infant leukemia show they often share the same leukemic clone. This supports the idea that it starts in the womb.
MLL Gene Rearrangements
Many infant leukemia cases have MLL gene rearrangements. The MLL gene is key for blood cell development. When it rearranges, it can cause leukemia. This is more common in infant leukemia than in older children.
- MLL gene rearrangements are linked to a poor prognosis in infant leukemia.
- These rearrangements affect treatment strategies and outcomes.
- Research on MLL gene rearrangements is ongoing. It could lead to new treatments.
A study onNCBI highlights the importance of genetic alterations in infant leukemia. Understanding these is key for effective treatments.
Maternal Exposures During Pregnancy
Maternal exposures during pregnancy might increase the risk of infant leukemia. This includes exposure to chemicals, radiation, and infections. While the evidence is not yet clear, it’s wise to avoid harmful substances during pregnancy.
“The role of maternal exposures in the development of infant leukemia is an area of active research, with studies examining the impact of various environmental factors on fetal development.”
In conclusion, infant leukemia is a complex condition. It involves in-utero origins, MLL gene rearrangements, and maternal exposures. More research is needed to understand these factors and their impact on prevention and treatment.
Prevention Strategies and Current Research
There’s no sure way to stop childhood leukemia yet. But, research keeps finding new paths. We’re looking into many ways to understand and maybe prevent this disease.
Limitations in Prevention
Stopping childhood leukemia is hard because it’s caused by many things. We don’t have a way to stop most cases yet.
Key Challenges in Prevention:
- We don’t fully know what causes it.
- Genetics and environment play a big role.
- Finding who’s at risk is tough.
Genetic Testing for High-Risk Families
Genetic testing might help families with a history of leukemia. If you have a family history, talk to a genetic counselor.
Testing can spot those at higher risk. This means we can watch them closer and act sooner.
| Genetic Syndrome | Leukemia Risk | Recommended Surveillance |
| Down Syndrome | Increased risk of ALL and AML | Regular blood counts, annual check-ups |
| Li-Fraumeni Syndrome | High risk of various cancers, including leukemia | Annual physical exams, advanced imaging |
Surveillance Recommendations
Children at risk need regular checks. This includes blood tests and doctor visits.
These checks should match the child’s risk and health history.
Promising Research Directions
Research is diving into what causes childhood leukemia. We’re looking at:
- How to avoid known dangers like radiation.
- Therapies that target specific genes.
- The impact of mom’s health during pregnancy.
As we learn more, we might find ways to prevent or treat leukemia better. This could really change how we handle childhood leukemia.
Conclusion: Understanding the Complex Origins of Childhood Leukemia
It’s key to understand childhood leukemia to find better ways to prevent and treat it. We’ve looked into how genetics, environment, and other factors play a role in its development.
The American Cancer Society and others keep funding research on childhood leukemia. This research is essential for learning more about the disease and finding new treatments.
As we learn more about childhood leukemia, we get closer to helping kids with this disease. By supporting research and raising awareness, we aim for a future where every child can survive and live well.
FAQ
What causes childhood leukemia?
Childhood leukemia is a complex disease. It’s caused by genetic and environmental factors. Research has found several risk factors, including genetic mutations and exposure to radiation.
Is childhood leukemia genetic?
Yes, some cases of childhood leukemia are genetic. But not all cases are inherited. Some occur due to mutations that happen during a child’s lifetime.
How do kids get leukemia?
Leukemia happens when there are mutations in genes that control blood cell development. These mutations can be inherited or caused by environmental exposures. Often, the exact cause is unknown.
What are the causes of childhood leukemia?
Causes include genetic factors and environmental exposures like radiation. Certain infections and genetic syndromes, like Down syndrome, also increase the risk.
What is the role of inherited genetic changes in childhood leukemia?
Inherited genetic changes can increase a child’s risk of leukemia. They affect genes that regulate blood cell production. But most cases are not directly caused by inherited mutations.
Does leukemia run in families?
Leukemia usually doesn’t run in families. But having a family history or certain genetic syndromes can slightly raise a child’s risk.
Can leukemia be prevented?
There’s no proven way to prevent most childhood leukemia cases. But research is ongoing into genetic testing and reducing exposure to risk factors.
What causes leukemia in infants?
Infant leukemia is often linked to specific genetic mutations, like MLL gene rearrangements. Maternal exposures during pregnancy may also play a role.
Is leukemia hereditary?
While some leukemia cases have a genetic component, it’s not typically hereditary. Most cases are sporadic, meaning they occur without a clear family history.
What are the risk factors for childhood leukemia?
Risk factors include genetic predisposition, exposure to ionizing radiation, and certain chemical exposures. Infections and some genetic syndromes also increase the risk.
How can we reduce the risk of childhood leukemia?
While some risks are unavoidable, reducing exposure to known dangers like ionizing radiation helps. Research is ongoing to find more prevention strategies.
Reference
- American Cancer Society. (2025, July 22). Key statistics for childhood leukemia. https://www.cancer.org/cancer/types/leukemia-in-children/key-statistics.html


































