
Diagnosing acute lymphoblastic leukemia (ALL) needs quick and accurate lab tests. At Liv Hospital, we put our patients first. We use the newest lab methods to give exact diagnoses and care plans.
A coordinated set of laboratory tests is key for spotting and treating acute leukemia. These tests include a complete blood count (CBC) with differential, a blood smear analysis, and genetic testing. Together, these acute leukemia labs help doctors make an accurate diagnosis and plan effective treatment.
Diagnosing acute leukemia is complex. It involves knowing its types and the tools used to diagnose it. This cancer affects the blood and bone marrow, causing the fast growth of immature blood cells. It’s important to tell AML from ALL to choose the right treatment.
Knowing the difference between AML and ALL is key. AML is more common in adults and affects the cells that make red blood cells and platelets. ALL, on the other hand, is more common in kids and affects the immune system cells.
ALL and AML have different patterns in who gets them. ALL is the top cancer in kids, while AML is more common as people get older. Knowing this helps doctors plan better treatment.
Getting a quick and correct diagnosis is very important. A late diagnosis can make the disease worse. A fast diagnosis lets doctors start treatment right away, which can save lives and improve quality of life.
| Diagnostic Factor | Acute Myeloid Leukemia (AML) | Acute Lymphoblastic Leukemia (ALL) |
| Age Distribution | More common in adults, incidence increases with age | More prevalent in children |
| Cell Lineage | Affects myeloid cells | Affects lymphoid cells |
| Treatment Approach | Intensive chemotherapy, targeted therapy | Combination chemotherapy, targeted therapy |
The table shows the main differences between AML and ALL. Understanding these helps doctors create better treatment plans. This can lead to better outcomes for patients.
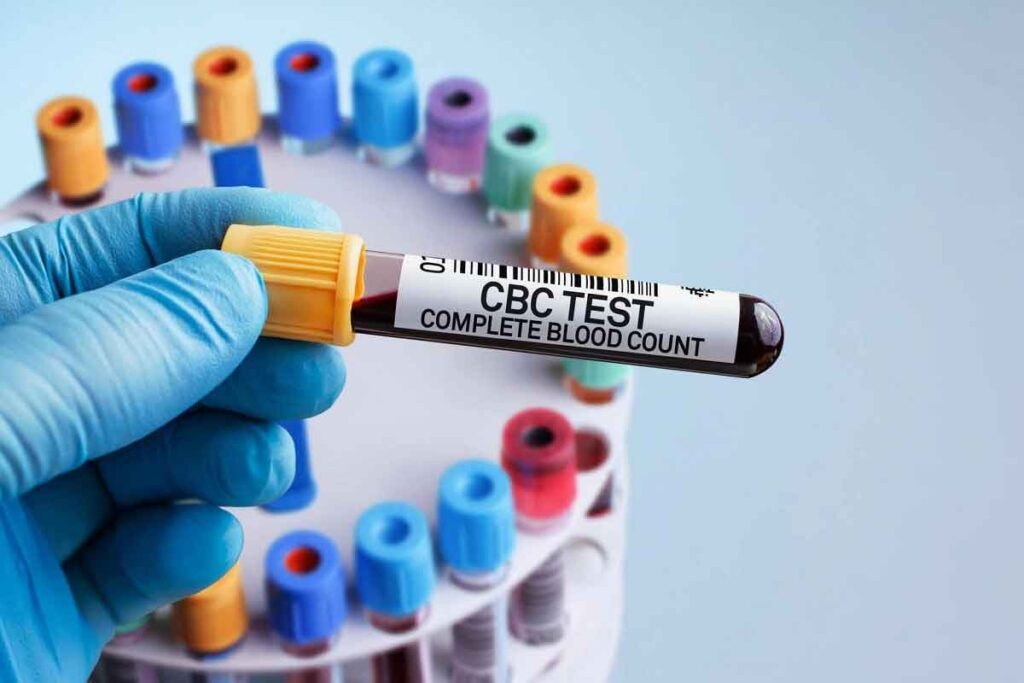
A Complete Blood Count (CBC) with Differential is often the first step in investigating suspected acute leukemia. This critical lab test measures the amounts of different cells in the blood. It includes red blood cells, white blood cells, and platelets. It provides valuable insights into the presence of abnormalities that may indicate leukemia.
In acute leukemia, the CBC often reveals significant abnormalities. Anemia, characterized by a low red blood cell count, is commonly observed. Thrombocytopenia, or a low platelet count, is another frequent finding. The white blood cell count can be either elevated (leukocytosis) or decreased (leukopenia), with the presence of blast cells often indicating leukemia.
The differential count, which distinguishes between different types of white blood cells, can show an increase in immature cells or blasts. These abnormalities collectively suggest the need for further diagnostic testing to confirm the presence of acute leukemia.
Interpreting CBC results requires an understanding of the differences between Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML). While both types can present with similar CBC abnormalities, certain patterns may be more indicative of one type over the other.
Understanding these differences is key for guiding further diagnostic tests and developing an appropriate treatment plan.
In diagnosing acute leukemia, a peripheral blood smear analysis is key. It helps doctors see the shape of blood cells. This is important for spotting signs of leukemia.
Peripheral blood smear analysis looks for blast cells. These are young cells that might mean leukemia if there are too many. Blast cells are big, have big nucleoli, and little cytoplasm. Seeing these cells in the blood can show leukemia, like ALL.
Blast cells are important because they show leukemia is present. They help tell the difference between ALL and AML. In ALL, you see lymphoblasts, which look different from myeloblasts in AML.
ALL’s blood smear shows lymphoblasts with special shapes. These include:
These shapes help tell ALL apart from other leukemias. They guide more tests and help diagnose ALL right.
| Morphological Feature | Description | Significance in ALL |
| High nuclear-to-cytoplasmic ratio | Indicates a large nucleus relative to the amount of cytoplasm | Characteristic of lymphoblasts |
| Fine chromatin | Refers to the texture of the nuclear material | Typical of immature lymphoid cells |
| Prominent nucleoli | Nucleoli are visible and often multiple | Indicative of active cell division |
Bone marrow tests, like aspiration and biopsy, are key in finding acute leukemia. They let doctors see the bone marrow’s cells up close. This helps spot cancer cells and other issues.
Bone marrow tests are done together. A needle takes out bone marrow fluid, and a small bone piece is removed. Medical guidelines say getting the samples right is very important.
The tests are done with local anesthesia. The fluid sample is checked for cell shape. The bone piece shows the marrow’s structure and how full it is.
Looking at bone marrow samples under a microscope is key. It finds out how many cancer cells there are. A lot of cancer cells mean acute leukemia.
Doctors look for cancer cells and count them. This helps figure out what kind of leukemia it is. It also helps plan treatment.
Bone marrow tests are essential for diagnosing acute leukemia. They are very important when tests like CBC and blood smear are not clear.
But, sometimes these tests are not needed. This is when a diagnosis is already made. For most, though, these tests are vital for confirming the disease and planning treatment.
Flow cytometry immunophenotyping is key in diagnosing acute leukemia. It helps tell different leukemia types apart. This method looks at cell surface markers on leukemic cells. It’s vital for correct diagnosis and treatment planning.
Flow cytometry is great for finding out if ALL cells are B-cell or T-cell. B-cell ALL shows markers like CD19, CD22, and CD10. On the other hand, T-cell ALL has markers like CD2, CD3, and CD7. Knowing the type is important because it affects treatment and outlook.
Sometimes, leukemia cells can have markers from both lineages. This is called mixed-phenotype acute leukemia (MPAL). Flow cytometry is key in spotting MPAL. It finds both myeloid and lymphoid markers on the same cells. MPAL is rare and aggressive, needing special treatment.
Flow cytometry also checks for minimal residual disease (MRD). MRD means there are leftover leukemic cells after treatment. Flow cytometry spots these cells by their unique markers. The MRD level tells us how well treatment is working and if more treatment is needed.
Understanding the genetic makeup of acute leukemia cells is key. Cytogenetic analysis, through karyotyping and FISH, gives us this insight. It’s a vital tool for diagnosing chromosomal abnormalities. These are important for predicting outcomes and treatment plans.
Acute Lymphoblastic Leukemia (ALL) shows various chromosomal issues. Some common ones are:
These issues greatly affect prognosis and treatment for ALL patients.
Cytogenetic findings are key in predicting outcomes for ALL. For example:
Knowing these factors helps tailor treatments to each patient’s needs.
The Philadelphia chromosome, from a t(9;22) translocation, is a major risk factor in ALL. Other important translocations include:
These genetic issues affect prognosis and treatment choices. For instance, Tyrosine Kinase Inhibitors (TKIs) are used for patients with the Philadelphia chromosome-positive ALL.
“The identification of specific chromosomal abnormalities has revolutionized the treatment of ALL, enabling a more personalized approach to therapy.”
Senior Hematologist
In summary, cytogenetic analysis is vital for diagnosing and managing acute leukemia. It helps identify chromosomal issues, guiding treatment and predicting outcomes.
Molecular genetic testing has changed how we diagnose and treat acute leukemia. Tools like Polymerase Chain Reaction (PCR) and Next-Generation Sequencing (NGS) help find specific genetic mutations. These findings guide treatment choices and predict outcomes.
PCR and NGS find fusion genes and mutations in acute leukemia. For example, the BCR-ABL1 fusion gene is key in some Acute Lymphoblastic Leukemia (ALL) cases. Finding these genetic changes is vital for correct diagnosis and treatment.
“The discovery of specific genetic mutations has changed leukemia treatment,” a top hematologist said. “It has led to personalized medicine.”
Molecular testing helps sort patients by risk level based on genetic markers. Some mutations mean a higher risk of relapse, needing stronger treatments. Others might get milder treatments, reducing side effects.
Molecular testing does more than diagnose; it predicts and guides treatment. New targets for therapy are found through NGS and other tech. For example, FLT3 and IDH1/2 mutations have led to promising new treatments in trials.
Biochemical and organ function tests are key in checking how acute leukemia affects the body. They help doctors track the disease’s growth and its impact on different organs. This allows for quick action to help the patient.
Tests for the liver and kidneys are vital in seeing how acute leukemia affects these important organs. Liver function tests, like ALT and AST, spot liver damage or issues. Kidney function tests, including serum creatinine and urea, check kidney health and find problems.
Tumor lysis syndrome (TLS) is a serious problem that can happen with acute leukemia. Biochemical markers like potassium, phosphate, calcium, and uric acid are watched to spot and treat TLS. High levels of these markers mean TLS might be happening, needing quick medical help.
Lactate dehydrogenase (LDH) is a key sign of how serious acute leukemia is. High LDH levels mean more tumor and a worse outlook. Other signs, like albumin levels and bilirubin, also show how severe the disease is and the patient’s health.
Diagnosing and treating acute leukemia well depends on combining lab results. Tests like the Complete Blood Count (CBC) and Bone Marrow Aspiration help a lot. They give doctors a full picture of the disease.
Understanding lab results is key to knowing the exact type of leukemia. This helps doctors choose the best treatment. Working together, healthcare teams make sure patients get the best care. This leads to better health and happiness for patients.
Lab results help doctors make treatment plans that fit each patient. They consider things like genetic changes and how much disease is left. Keeping up with new lab tests and research helps doctors give top-notch care. This makes diagnosis and treatment more effective for patients with acute leukemia.
To diagnose acute leukemia, several tests are used. These include a complete blood count (CBC) and a blood smear analysis. Bone marrow tests, flow cytometry, and genetic tests are also used.
The CBC is key in diagnosing acute leukemia. It checks the blood for different types of cells. It can show if there are too many or too few cells, which is a sign of leukemia.
This test looks at blood cell shapes. It helps find abnormal cells, like blast cells. It’s a big help in diagnosing acute leukemia.
These tests are vital for diagnosing acute leukemia. They take a sample of bone marrow. This sample is checked for abnormal cells, which is key in making a diagnosis.
This test helps sort leukemia types. It looks at cell surface markers. This helps tell if it’s B-cell or T-cell ALL and checks for other types of leukemia.
This test looks for genetic changes in leukemia cells. It uses karyotyping and FISH to find things like translocations. These findings help predict how the disease will progress.
This test finds specific genetic changes in leukemia cells. PCR and NGS look for genes that affect treatment and how the disease will progress.
These tests check how leukemia affects the body. They look at liver and kidney function, and other markers. This helps understand the disease’s impact.
Combining lab results is key for treating acute leukemia. It gives a full picture of the disease. This helps doctors plan the best treatment.
Quick and correct diagnosis is vital for treating acute leukemia. It helps doctors choose the right treatment plan. This is important for better patient outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us