
Getting a correct diagnosis of Acute Lymphoblastic Leukemia (ALL) depends on key lab tests. These tests help figure out if you have the disease, what type it is, and how serious it is.
The BC Cancer Clinical Pharmacy Guide says starting with a Complete Blood Count (CBC) and a blood smear is important. These tests give vital info about your health. They help doctors decide what to do next.
When it comes to diagnosis of ALL (acute lymphoblastic leukemia), a detailed check is done. This makes sure each patient gets the right care fast and helps doctors tailor treatment plans to fit each person’s needs.
Key Takeaways
- Lab tests are key for diagnosing ALL.
- CBC and blood smear are first steps.
- Comprehensive assessment leads to personalized care.
- Accurate diagnosis is vital for good treatment.
- Quick results help improve patient outcomes.
The Clinical Presentation and Pathophysiology of ALL
Understanding ALL’s pathophysiology is key for early diagnosis and treatment. Acute Lymphoblastic Leukemia (ALL) is a complex disorder. It involves the uncontrolled growth of lymphoid cells that don’t mature into normal lymphocytes.
Definition and Disease Mechanism
ALL is marked by the buildup of cancerous lymphoblasts in the bone marrow and blood. It’s caused by genetic changes that stop normal cell development. The National Cancer Institute says knowing these genetic changes is critical for diagnosis and treatment planning.
Genetic problems in ALL can lead to uncontrolled cell growth. For example, the BCR-ABL1 gene, found in some cases, is a bad sign for the patient’s future.
Common Signs and Symptoms
ALL’s symptoms vary but often show bone marrow failure. This can include anemia, low white blood cells, and low platelets. Common symptoms are:
- Pallor and fatigue from anemia
- Infections from low white blood cells
- Bleeding or bruising from low platelets
- Bone pain and joint pain
- Enlarged liver, spleen, and lymph nodes
Risk Factors and Epidemiology
ALL is more common in kids, peaking between 2 and 5 years old. It can also affect adults, who often have a worse prognosis. Risk factors include genetic conditions like Down syndrome and exposure to harmful substances.
Studies have found several risk factors for ALL. Here’s a table of some key ones:
| Risk Factor | Description | Implication |
| Genetic Syndromes | Conditions like Down syndrome | Increased risk of developing ALL |
| Ionizing Radiation | Exposure to high levels of radiation | Increased risk of ALL, mainly in children |
| Chemical Exposure | Exposure to certain chemicals, such as benzene | Potential increased risk of ALL |
Knowing these risk factors and symptoms is vital for early detection and treatment of ALL.
Initial Screening: Complete Blood Count and Peripheral Blood Smear
A CBC and Peripheral Blood Smear are key steps in finding ALL. They give us important info about blood cell shapes. These tests help us understand blood issues, as the BC Cancer Clinical Pharmacy Guide explains.
CBC Abnormalities in ALL
The CBC helps spot odd blood cell counts, which might mean ALL. Common signs include:
- Anemia: Low hemoglobin means you might feel tired and look pale.
- Thrombocytopenia: Fewer platelets can cause bruises and bleeding.
- Leukocytosis or Leukopenia: Either too many or too few white blood cells, a leukemia sign.
These signs mean we need to do more tests to figure out what’s going on.
Peripheral Blood Smear Examination
The Peripheral Blood Smear lets us see blood cell shapes up close. In ALL, we might see:
- Blast Cells: Young cells that show leukemia.
- Abnormal Lymphocytes: Cells that look different, like they’re not quite right.
This test is key for spotting leukemia cells in the blood. It helps us diagnose ALL.
Gold Standard: Bone Marrow Aspiration and Biopsy
Bone marrow examination through aspiration and biopsy is the best way to diagnose ALL.
Procedure Overview and Patient Preparation
The bone marrow aspiration and biopsy take a sample from the hip bone (pelvis). Patient preparation is key. It includes explaining the procedure, its risks, and benefits, and getting informed consent.
Patients lie on their stomach or side. The skin over the hip is cleaned and numbed with local anesthesia to reduce pain.
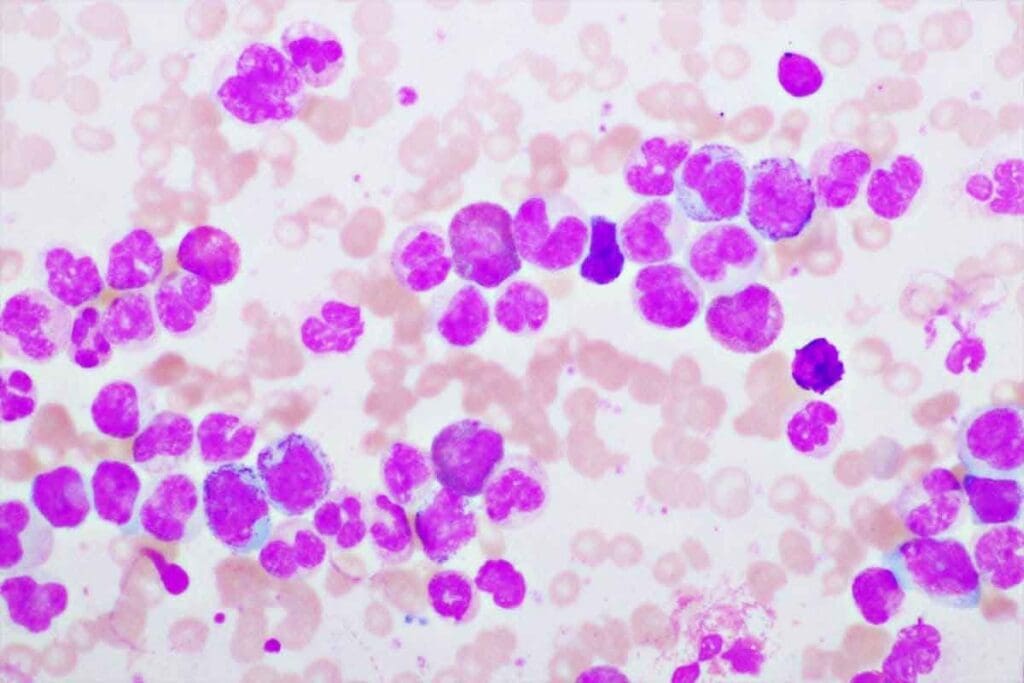
Morphologic Assessment of Bone Marrow
The bone marrow is examined under a microscope. This checks for different cell types and their numbers.
In ALL, the marrow has lymphoblasts, abnormal cells. The morphologic assessment finds these cells and how much marrow they occupy.
| Parameter | Normal Bone Marrow | ALL Infiltrated Bone Marrow |
| Cellularity | 30-70% | Often hypercellular |
| Lymphoblasts | >20% (often majority) | |
| Morphology | Normal hematopoietic cells | Lymphoblasts with characteristic features |
Sample Collection for Additional Testing
After the bone marrow test, samples are used for more tests. These include immunophenotyping, cytogenetic analysis, and molecular genetic testing.
These tests tell us about the leukemia’s genetic makeup. This info is vital for planning treatment.
Immunophenotyping: Flow Cytometry in Diagnosis of ALL
Flow cytometry is key in diagnosing ALL. It helps doctors understand the disease better. This method is vital for identifying and classifying ALL, showing the type and maturity of cancer cells.
Principles and Methodology
Immunophenotyping looks at proteins on cell surfaces or inside cells. Flow cytometry checks for many antigens at once. This makes it a must-have for finding the exact type of ALL.
Methodology: Cells are first labeled with fluorescent antibodies. Then, they go through a flow cytometer. This machine measures how bright the cells glow, helping spot different cell types based on their proteins.
B-Cell ALL Immunophenotypic Markers
B-Cell ALL shows certain B-cell markers. These include CD19, CD20, CD22, and CD10. Finding these markers helps diagnose B-Cell ALL and shows when the leukemia started.
- CD19: A pan-B-cell marker that is typically expressed in B-Cell ALL.
- CD20: Expressed on the surface of B-cells, often used in conjunction with other markers.
- CD22: Another B-cell marker that is frequently expressed in B-Cell ALL.
- CD10: Commonly known as CALLA (Common Acute Lymphoblastic Leukemia Antigen), it is often positive in B-Cell ALL.
T-Cell ALL Immunophenotypic Markers
T-Cell ALL is found by looking at T-cell markers. Important markers include CD2, CD3, CD5, CD7, and CD1a. These markers help diagnose T-Cell ALL and show its developmental stage.
- CD2 and CD7: Early T-cell markers often expressed in T-Cell ALL.
- CD3: A definitive T-cell marker, typically expressed cytoplasmically in early T-cell development.
- CD5: Expressed on T-cells and a subset of B-cells.
- CD1a: Expressed during the cortical stage of T-cell development.
Minimal Residual Disease Detection
Flow cytometry is key in finding Minimal Residual Disease (MRD) in ALL. MRD is when cancer cells are too few to see with regular tests. It helps plan treatment and check how well it’s working.
MRD detection is very important. It can tell if cancer might come back. Flow cytometry’s ability to find MRD makes it a big help in caring for ALL patients.
Cytogenetic Analysis: Karyotyping and FISH
Diagnosing and managing ALL heavily relies on cytogenetic analysis. This includes karyotyping and FISH. These methods give vital info for risk stratification, helping tailor treatments to each patient.
Conventional Karyotyping Techniques
Karyotyping examines chromosomes in a cell sample, usually from bone marrow. It spots chromosomal issues like translocations and deletions, common in ALL.
The BC Cancer Clinical Pharmacy Guide says cytogenetic analysis is key in ALL diagnosis. Accurate karyotyping is vital for finding genetic issues that guide treatment.
Common Chromosomal Abnormalities
ALL is linked to several chromosomal issues. These include the Philadelphia chromosome, MLL gene rearrangements, and hyperdiploidy. These affect prognosis and are used for risk stratification.
| Chromosomal Abnormality | Prognostic Impact |
| Philadelphia chromosome (t(9;22)) | Generally associated with a poorer prognosis |
| MLL gene rearrangements | Variable prognosis depending on the specific rearrangement |
| Hyperdiploidy | Often associated with a favorable prognosis |
Fluorescence In Situ Hybridization (FISH)
FISH is a precise method for spotting specific genetic issues. It uses fluorescent probes to highlight genetic changes in cells.
“FISH analysis has become an indispensable tool in the diagnosis of hematological malignancies, providing high sensitivity and specificity for detecting genetic abnormalities.”
Impact on Risk Stratification
Cytogenetic analysis, including karyotyping and FISH, is key for ALL risk stratification. It helps sort patients into risk groups, guiding treatment intensity and choice.
Cytogenetic analysis is vital in ALL diagnosis and management. It offers essential info for risk stratification and treatment planning. By understanding ALL’s genetic makeup, clinicians can provide more personalized care.
Molecular Genetic Testing for ALL
Advances in molecular genetic testing have changed how we diagnose and treat ALL. This testing is key for finding specific genetic mutations linked to the disease.
PCR-Based Assays
PCR (Polymerase Chain Reaction) based assays are a big part of molecular genetic testing for ALL. They help spot specific genetic mutations, like the BCR-ABL1 fusion gene. This gene is a sign of certain ALL types.
These assays help doctors accurately diagnose ALL and track how well it responds to treatment.
Next-Generation Sequencing Applications
Next-generation sequencing (NGS) is a powerful tool for diagnosing ALL. It lets doctors look at many genes at once. This way, it finds complex genetic mutations that PCR-based assays might miss.
NGS is great for finding mutations that mean a worse prognosis or resistance to some treatments.
Key Genetic Mutations and Their Significance
ALL is linked to several genetic mutations, like the ETV6-RUNX1 fusion, MLL gene rearrangements, and IKZF1 deletions. Knowing about these mutations is vital for figuring out the risk and planning treatment.
| Genetic Mutation | Significance in ALL |
| BCR-ABL1 fusion | Associated with a poor prognosis; targets for tyrosine kinase inhibitors |
| ETV6-RUNX1 fusion | Common in pediatric ALL; generally associated with a favorable prognosis |
| MLL gene rearrangements | Often associated with a poor prognosis; more common in infant ALL |
Imaging Studies in ALL Assessment
Imaging tools are key in checking and staging Acute Lymphoblastic Leukemia (ALL). They show how far the disease has spread. These studies help see if the disease is in places outside the bone marrow and guide treatment.
Chest Radiography
Chest X-rays are a first step in checking ALL patients. They spot big masses in the chest, common in T-cell ALL. They also find other issues like fluid in the lungs.
Key findings on chest radiography may include:
- Mediastinal widening due to lymphadenopathy or thymic enlargement
- Pleural effusions
- Pulmonary infiltrates
Abdominal Ultrasound
Abdominal ultrasound is also important for ALL checks. It’s great for looking at the liver and spleen and finding lymph nodes in the belly.
“Ultrasound is a non-invasive and effective method for assessing abdominal involvement in ALL, providing valuable information on organ size and possible lymph node enlargement.”
Ultrasound helps in:
- Checking liver and spleen size
- Finding big lymph nodes
- Helping decide on biopsies
CT and MRI Applications
CT and MRI scans give more detailed views of the disease. CT scans are good for looking at lymph nodes and organs. MRI shows soft tissues well.
CT and MRI are used for:
| Imaging Modality | Primary Use in ALL Assessment |
| CT Scan | Evaluating lymphadenopathy and organ involvement |
| MRI | Providing detailed soft tissue assessment |
PET-CT in Selected Cases
PET-CT is used sometimes to see how active disease sites are. It’s helpful in checking on masses after treatment.
Using different imaging studies together helps get a clear picture of ALL. This lets doctors understand the disease better and plan treatments well.
Lumbar Puncture and CNS Evaluation
The evaluation of CNS involvement through lumbar puncture is key in diagnosing and managing ALL.
Procedure and Technique
Lumbar puncture, also known as a spinal tap, collects cerebrospinal fluid (CSF) for tests. It’s done by inserting a needle between two vertebrae in the lower back, usually between L3-L4 or L4-L5.
Key steps in the procedure include:
- Patient positioning: The patient is positioned on their side with knees drawn up to the chest.
- Sterilization: The skin is cleaned and sterilized to minimize the risk of infection.
- Local anesthesia: Local anesthetic is administered to reduce discomfort.
- Needle insertion: A spinal needle is carefully inserted between the vertebrae.
CSF Analysis Parameters
CSF analysis is vital for checking CNS involvement in ALL. The main things looked at include:
| Parameter | Description | Significance in ALL |
| CSF Cell Count | Measures the number of cells in the CSF | Elevated cell count may indicate CNS involvement |
| CSF Differential | Identifies the types of cells present | Presence of blasts suggests leukemic infiltration |
| Protein Levels | Measures the concentration of protein in CSF | Elevated protein may indicate disruption of the blood-CSF barrier |
| Glucose Levels | Measures the concentration of glucose in CSF | Low glucose may indicate CNS involvement or infection |
CNS Involvement Classification
CNS involvement in ALL is classified based on the presence and characteristics of leukemic cells in the CSF. The main classifications are:
- CNS1: No blasts in CSF
- CNS2: Blasts present, but CSF cell count is normal
- CNS3: Blasts present with elevated CSF cell count
Prophylactic Intrathecal Therapy
Prophylactic intrathecal therapy involves giving chemotherapy directly into the CSF to prevent CNS involvement. This is very important for patients at high risk of CNS relapse.
The goal of prophylactic intrathecal therapy is to:
- Eliminate leukemic cells from the CNS
- Reduce the risk of CNS relapse
- Improve overall survival rates
Conclusion: Integrated Approach to ALL Diagnosis and Classification
An integrated approach is key for accurate diagnosis and classification of Acute Lymphoblastic Leukemia (ALL). This method combines various lab tests. It includes clinical presentation, lab tests, and imaging studies.
Healthcare professionals use Complete Blood Count (CBC), Peripheral Blood Smear, and Bone Marrow Aspiration and Biopsy. They also use Immunophenotyping, Cytogenetic Analysis, Molecular Genetic Testing, and Imaging Studies. This way, they can accurately diagnose and classify ALL.
This approach helps clinicians make better treatment decisions. It improves patient outcomes. The detailed assessment helps in risk stratification and targeted therapy.
In conclusion, diagnosing and classifying ALL needs a multifaceted approach. It uses a range of diagnostic tools and techniques. This shows the importance of an integrated approach to ALL diagnosis and classification.
FAQ
What lab tests are used to diagnose Acute Lymphoblastic Leukemia (ALL)?
To diagnose ALL, doctors use several lab tests. These include a Complete Blood Count (CBC), a peripheral blood smear, and bone marrow tests. They also use flow cytometry, cytogenetic analysis, and molecular genetic testing.
What are the typical CBC abnormalities in ALL?
In ALL, CBC tests often show anemia, low platelets, and too many or too few white blood cells. The presence of blasts is a key finding.
How is peripheral blood smear examination helpful in diagnosing ALL?
A peripheral blood smear helps spot blasts. This is a key step in diagnosing ALL.
What is the role of bone marrow aspiration and biopsy in ALL diagnosis?
Bone marrow tests are key for diagnosing ALL. They provide a sample for detailed analysis and testing.
How is immunophenotyping used in the diagnosis of ALL?
Immunophenotyping uses flow cytometry to find specific markers on leukemia cells. It helps tell if it’s B-Cell or T-Cell ALL and checks for disease leftovers.
What is the significance of cytogenetic analysis in ALL?
Cytogenetic analysis looks for chromosomal changes. These changes help determine the risk level and guide treatment.
What molecular genetic tests are used in ALL diagnosis?
Molecular tests, like PCR and next-generation sequencing, find genetic mutations. These tests help diagnose and manage the disease.
How are imaging studies used in assessing ALL?
Imaging tests, such as CT scans and MRI, check how far the disease has spread. They help doctors understand the extent of the disease.
What is the purpose of lumbar puncture in ALL diagnosis?
A lumbar puncture checks the cerebrospinal fluid for disease. It also helps with treatment by adding medicine directly to the brain and spinal cord.
How is CNS involvement classified in ALL?
CNS involvement is classified by the presence and type of leukemia cells in the cerebrospinal fluid.
What is the importance of detecting minimal residual disease in ALL?
Finding minimal residual disease helps track treatment success. It also predicts if the disease might come back.
How do lab tests guide treatment decisions in ALL?
Lab tests provide vital information for treatment planning. They include CBC, bone marrow tests, and genetic tests. This helps doctors make the best treatment choices for each patient.
References:
- Kroft, S. H. (2025). Laboratory Evaluation of Acute Leukemia. In StatPearls. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK611988/























