Last Updated on November 20, 2025 by Ugurkan Demir
Knowing about hemoglobin levels is key to managing sickle cell disease well. Sickle cell disease is a blood disorder caused by a problem with hemoglobin, the protein that carries oxygen in red blood cells. Understanding a hemoglobin concentration in sickle cell disease helps doctors see how severe the condition is and decide on the best treatment.
People with sickle cell disease usually have low hemoglobin levels, often between 7–10 g/dL, because their red blood cells are destroyed faster and produced less. At Liv Hospital, we use the latest research and medical knowledge to give our patients the best care, tailoring treatment to meet each patient’s specific needs.
Key Takeaways
- Understanding hemoglobin levels is key to managing sickle cell disease.
- Low hemoglobin levels are common in sickle cell disease patients.
- The level of hemoglobin affects how severe the disease is and treatment choices.
- Good care means knowing a lot about blood disorders related to hemoglobin.
- Liv Hospital offers top-notch, ethical care for sickle cell disease patients.
The Fundamentals of Hemoglobin and Sickle Cell Disease

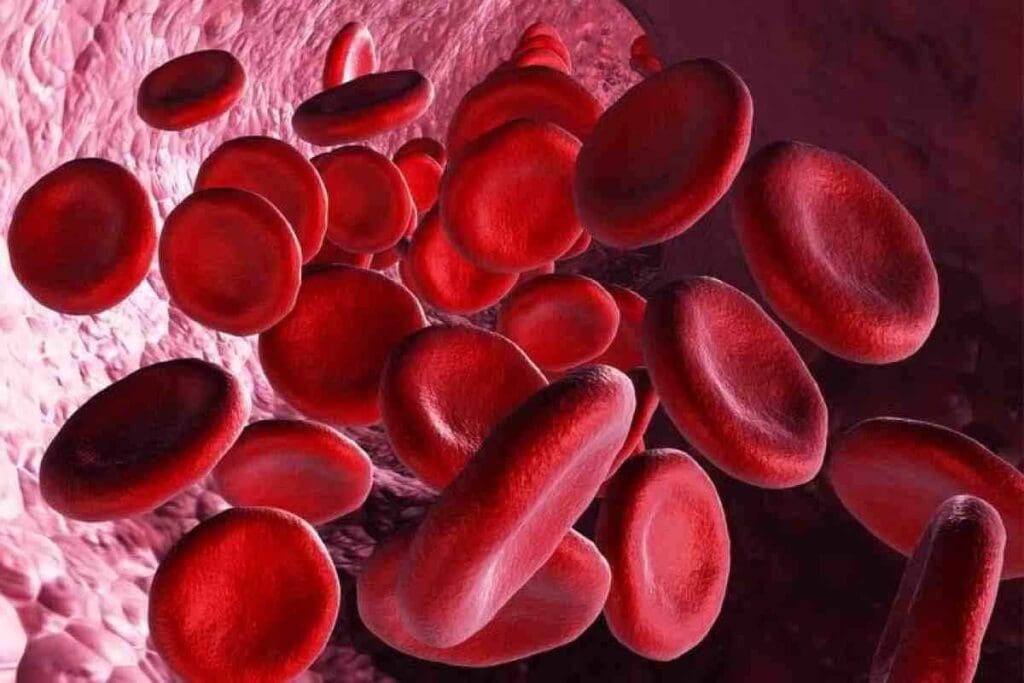
Hemoglobin is a key protein in red blood cells. It’s vital for carrying oxygen from the lungs to the body’s tissues. We’ll look at how normal hemoglobin works and the genetic cause of abnormal hemoglobin S.
How Normal Hemoglobin Functions in the Body
Normal hemoglobin is key for the body’s oxygen supply. It has four protein chains: two alpha-globin and two beta-globin chains. Its proper function is essential for:
- Delivering oxygen to tissues and organs
- Maintaining healthy red blood cells
- Supporting overall bodily functions
In healthy people, hemoglobin levels stay within a certain range. But, abnormalities like those in sickle cell disease can cause serious health problems.
The Genetic Basis of Abnormal Hemoglobin S
Sickle cell disease comes from a genetic mutation in the HBB gene. This mutation causes abnormal hemoglobin S (HbS). The genetic cause of sickle cell disease involves:
- A point mutation in the HBB gene, replacing glutamic acid with valine at position 6 of the beta-globin chain.
- The disease follows an autosomal recessive inheritance pattern. This means a person needs two defective HBB genes (one from each parent) to have the disease.
Knowing the genetic cause of abnormal hemoglobin S is key for diagnosing and managing sickle cell disease. It also shows why genetic counseling is important for families with the disease.
Fact 1: A Hemoglobin Concentration in Sickle Cell Disease Typically Ranges from 7-10 g/dL

In people with sickle cell disease, their hemoglobin levels usually fall in a certain range. This range helps doctors understand how severe the anemia is and how to manage it well.
Understanding Normal vs. Sickle Cell Hemoglobin Levels
Adults usually have hemoglobin levels between 13.5 to 17.5 g/dL. But, those with sickle cell disease have levels between 7-10 g/dL. This is much lower than normal. It’s because of the abnormal hemoglobin S (HbS) in the disease, which causes red blood cells to break down early.
Key differences between normal and sickle cell hemoglobin levels include:
- Normal hemoglobin levels are typically above 13.5 g/dL.
- Sickle cell disease hemoglobin levels are usually between 7-10 g/dL.
- The presence of HbS causes a reduction in the lifespan of red blood cells.
Why Baseline Levels Average Around 8 g/dL
The average baseline hemoglobin level in sickle cell disease patients is about 8 g/dL. This is due to several reasons. These include how much red blood cells are being destroyed, how well the body can handle anemia, and the presence of other hemoglobin types like fetal hemoglobin (HbF). Studies show that keeping hemoglobin around 8 g/dL is a balance between making new red blood cells and losing them.
Having a baseline hemoglobin level of about 8 g/dL has big implications. It affects how often blood transfusions are needed, the risk of sickle cell crises, and how patients are managed. It’s key for doctors to understand these factors to create good treatment plans.
Fact 2: Red Blood Cell Destruction Drives Low Hemoglobin Levels
Red blood cell destruction, or hemolysis, is a key feature of sickle cell disease. It greatly affects hemoglobin levels. We will look into how hemolysis happens and its effects on red blood cells.
The Mechanism of Hemolysis in Sickle Cell Disease
Hemolysis happens because of sickle-shaped red blood cells that break down early. These cells turn sickle-shaped when hemoglobin S polymerizes under low oxygen. This makes them stiff and more likely to be destroyed by the spleen.
The damage gets worse because these cells stick to blood vessel walls. This causes blockages and more damage to red blood cells. So, red blood cells in sickle cell disease don’t live as long as they should.
Shortened Red Cell Lifespan and Its Consequences
Normally, red blood cells last about 120 days. But in sickle cell disease, they only last 10-20 days. This means the body needs to make new red blood cells all the time.
This constant need puts a lot of pressure on the bone marrow. It can lead to anemia because the bone marrow can’t keep up. People with sickle cell disease often have low hemoglobin levels. This can cause fatigue, shortness of breath, and a higher risk of infections.
It’s important to understand hemolysis and how it shortens red blood cell lifespan. This knowledge helps doctors find better ways to treat sickle cell disease. By tackling these issues, healthcare providers can improve patient care.
Fact 3: Different Sickle Cell Genotypes Show Varying Hemoglobin Patterns
Different sickle cell disease genotypes lead to different hemoglobin patterns. This affects how severe the disease is. People with sickle cell disease have abnormal hemoglobin, called hemoglobin S. The type of sickle cell disease someone has can change their hemoglobin levels and how severe their disease is.
Homozygous HbSS and Severe Anemia
Those with the homozygous HbSS genotype, or sickle cell anemia, often have more severe anemia. This is because their red blood cells have a lot of hemoglobin S. This genotype usually means hemoglobin levels are very low, between 7-10 g/dL. The homozygous HbSS genotype is the most common type of sickle cell disease. It has two abnormal beta-globin genes.
Hemoglobin SC Disease and Higher Baseline Levels
On the other hand, people with hemoglobin SC disease have higher hemoglobin levels. This condition comes from having one hemoglobin S gene and one hemoglobin C gene. Those with this genotype usually have milder anemia and fewer problems. This is because hemoglobin C helps counteract the effects of hemoglobin S.
The Role of Hemoglobin F in Modifying Disease Severity
Hemoglobin F, or fetal hemoglobin, plays a big role in how sickle cell disease affects people. More hemoglobin F means less severe disease and fewer problems. Hemoglobin F stops hemoglobin S from sticking together, which reduces sickling episodes. Therapeutic strategies that increase hemoglobin F levels, like hydroxyurea, can help patients with sickle cell disease.
The different hemoglobin patterns in sickle cell disease show how complex it is. Knowing these differences is key to creating effective treatment plans for each patient.
- Homozygous HbSS: More severe anemia, lower hemoglobin levels.
- Hemoglobin SC disease: Milder anemia, higher baseline hemoglobin levels.
- Hemoglobin F: Modifies disease severity, reduces frequency of sickling episodes.
Fact 4: Hemoglobin Concentration Directly Impacts Clinical Symptoms
Hemoglobin levels are key in how sickle cell disease symptoms show up. We’ll see how these levels affect organ damage and when a sickle cell crisis happens.
Correlation Between Hemoglobin Levels and Organ Damage
Low hemoglobin levels raise the risk of organ damage in sickle cell disease patients. When hemoglobin drops, tissues and organs get less oxygen. This can cause damage. Chronic anemia leads to fatigue, shortness of breath, and less ability to exercise, making the disease harder to manage.
Organ damage comes from repeated episodes of ischemia and infarction by sickled red blood cells. For example, splenic sequestration can harm the spleen. Repeated infarctions can damage the kidneys, liver, and other vital organs.
How Low Hemoglobin Triggers Sickle Cell Crisis
A low hemoglobin level can start a sickle cell crisis by making more sickled red blood cells in the blood. When hemoglobin is low, blood gets thicker, raising the chance of vaso-occlusion. This can cause severe pain, acute chest syndrome, and other sickle cell disease complications.
It’s important to manage anemia to avoid these problems. Keeping hemoglobin levels right can lower the risk of a sickle cell crisis. This means using medicine, changing lifestyle, and checking hemoglobin levels often.
Fact 5: Hemoglobin Electrophoresis Test Is Essential for Diagnosis and Monitoring
Hemoglobin electrophoresis is key in diagnosing and managing sickle cell disease. It helps find out the types of hemoglobin in a patient’s blood. This is vital for diagnosing sickle cell disease and tracking its progress.
How the Test Identifies Different Hemoglobin Types
Hemoglobin electrophoresis separates hemoglobin types by their electrical charge. This lets doctors spot abnormal hemoglobin, like Hemoglobin S, which is a sign of sickle cell disease. Knowing the hemoglobin types helps doctors diagnose and keep track of the disease’s severity.
Frequency of Testing Recommendations
How often to test for hemoglobin electrophoresis depends on the patient’s condition and disease stage. People with sickle cell disease might need regular tests to watch their hemoglobin levels. Studies show that regular checks help adjust treatment plans to manage the disease better https://pmc.ncbi.nlm.nih.gov/articles/PMC8148117/.
For those with sickle cell disease, knowing their hemoglobin types is essential. Hemoglobin electrophoresis helps in:
- Finding Hemoglobin S
- Measuring Hemoglobin F levels, which affect disease severity
- Tracking changes in hemoglobin types over time
Medical literature says, “Hemoglobin electrophoresis remains the gold standard for diagnosing and characterizing hemoglobinopathies” – a statement that highlights its critical role in medical practice.
Fact 6: Multiple Factors Influence Hemoglobin Levels in Sickle Cell Disease
Many things, like dehydration and oxidative stress, affect hemoglobin levels in sickle cell disease. We will look into how these factors impact the condition and its management.
Dehydration and Oxidative Stress Effects
Dehydration is a big problem that makes sickling crises worse. It raises the concentration of hemoglobin S in red blood cells. When patients are dehydrated, their red blood cells are more likely to sickle. This leads to a cycle of cell destruction and more dehydration.
Oxidative stress also plays a big role in sickle cell disease. The abnormal hemoglobin S is more likely to oxidize. This creates reactive oxygen species that damage red blood cells and lead to their early destruction.
Impact of Hemoglobin S Concentration on Sickling
The amount of hemoglobin S is key to how severe sickling is. More hemoglobin S means more chance of sickling. This is because there are more chances for the abnormal hemoglobin to polymerize when oxygen levels are low.
The table below summarizes the key factors influencing hemoglobin levels in sickle cell disease and their effects on the condition.
| Factor | Effect on Hemoglobin Levels | Impact on Sickle Cell Disease |
| Dehydration | Increases hemoglobin S concentration | Exacerbates sickling crises |
| Oxidative Stress | Contributes to red blood cell damage | Premature destruction of red blood cells |
| Hemoglobin S Concentration | Directly influences sickling severity | Increases risk of sickling crises |
It’s important to understand these factors for better management of sickle cell disease. By tackling dehydration, reducing oxidative stress, and keeping an eye on hemoglobin S concentration, healthcare providers can lessen the severity of sickling crises.
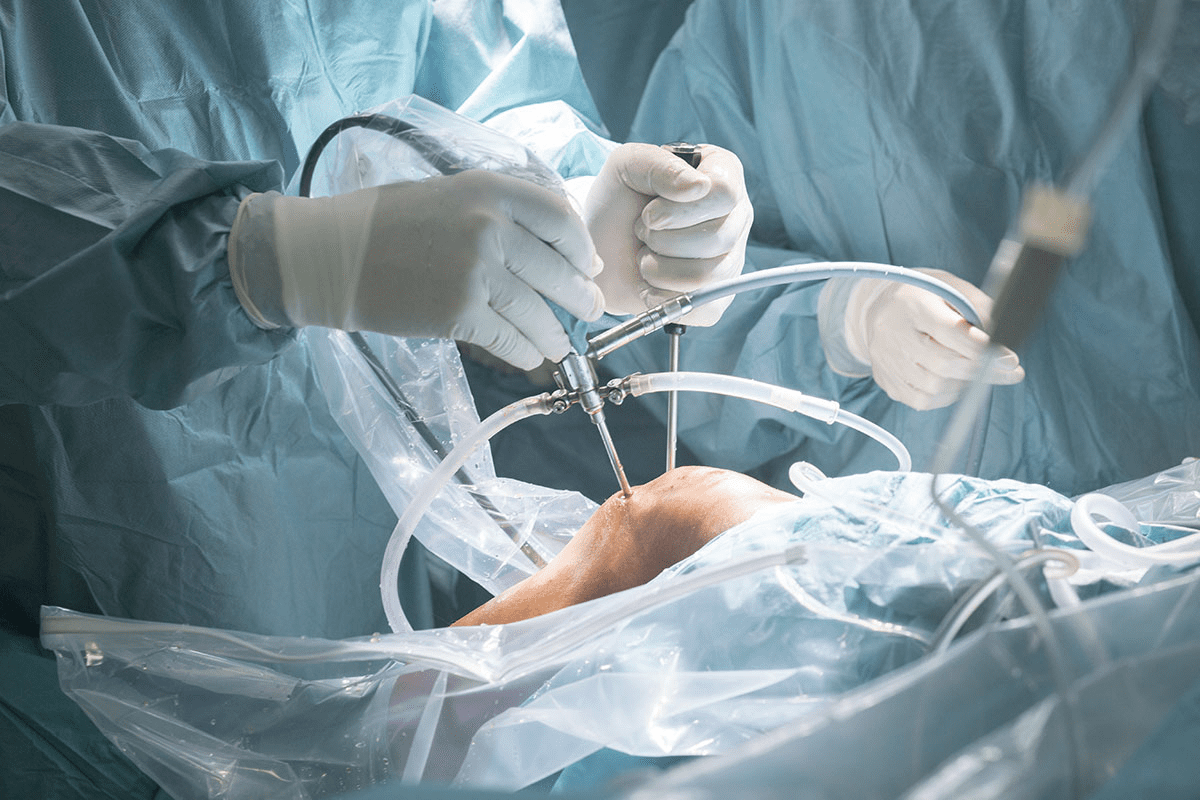
Fact 7: Blood Transfusions Play a Critical Role in Managing Hemoglobin Levels
Hemoglobin management in sickle cell disease often includes blood transfusions. These transfusions help increase hemoglobin levels. They also lower the risk of complications from sickle cell disease. We will look at when transfusions are needed and the different ways they are given.
Indications for Transfusion
Blood transfusions are needed in several situations for sickle cell disease patients. These include:
- Acute chest syndrome
- Severe anemia
- Stroke or other acute neurological events
- Preoperative preparation to reduce surgical risks
Transfusions introduce normal red blood cells. This helps improve oxygen delivery to tissues. It also reduces the risk of vaso-occlusive crises.
Simple vs. Exchange Transfusion Protocols
There are two main transfusion methods for sickle cell disease: simple transfusion and exchange transfusion.
Simple Transfusion: This method increases hemoglobin levels without removing the patient’s red cells. It’s often used for severe anemia or acute chest syndrome.
Exchange Transfusion: This involves exchanging the patient’s red cells for donor red cells. It’s used in emergencies like stroke or severe acute chest syndrome. It quickly lowers hemoglobin S levels.
Both methods have their uses, depending on the patient’s situation. The goal is to improve oxygen delivery and lower the risk of complications from sickle cell disease.
Therapeutic Approaches to Increase Hemoglobin in Sickle Cell Disease
Boosting hemoglobin levels is key in treating sickle cell disease. We’ll look at current and new treatments to increase hemoglobin. This can lessen disease severity and improve patient outcomes.
Hydroxyurea Therapy and Hemoglobin F Induction
Hydroxyurea is a main treatment for sickle cell disease. It boosts fetal hemoglobin (Hemoglobin F) production. This type of hemoglobin is less likely to cause sickling than adult hemoglobin.
Research shows hydroxyurea cuts down on painful crises and blood transfusions. A study on PMC found it increases Hemoglobin F levels effectively.
The benefits of hydroxyurea therapy include:
- Reduced frequency of sickle cell crises
- Decreased need for blood transfusions
- Increased Hemoglobin F production
Emerging Gene Therapies and Novel Treatments
Gene therapy is a promising area for sickle cell disease treatment. It aims to fix the genetic mutation causing the disease. This could restore normal hemoglobin production.
Several clinical trials are testing gene therapies for sickle cell disease.
Some of the emerging gene therapies include:
| Therapy Type | Description | Current Status |
| Lentiviral Gene Therapy | Involves using a lentivirus to deliver a corrected copy of the HBB gene into patient cells. | Clinical Trials |
| CRISPR/Cas9 Gene Editing | A precise gene-editing technique that can correct the sickle cell mutation. | Early Stage Clinical Trials |
| Gene Expression Modulation | Therapies that aim to increase Hemoglobin F production by modulating gene expression. | Preclinical Studies |
These new therapies bring hope for sickle cell disease patients. As research improves, we’ll see better treatments. These could manage or even cure the disease.
Conclusion: Optimizing Hemoglobin Management for Better Quality of Life
Managing hemoglobin levels well is key to reducing sickle cell disease complications. Knowing about hemoglobin helps us manage anemia better. This leads to better health outcomes.
Improving hemoglobin management means using many strategies. These include regular blood checks, transfusions, and treatments like hydroxyurea. These steps help lessen the disease’s impact and improve life quality for those with sickle cell disease.
We understand that treating anemia in sickle cell disease is complex. It needs a detailed plan that meets patient needs. By focusing on better hemoglobin management, we can make patients’ lives better and lower disease risks.
FAQ
What is the typical range of hemoglobin concentration in sickle cell disease?
In sickle cell disease, hemoglobin levels usually range from 7-10 g/dL. The average is about 8 g/dL.
How does hemolysis contribute to low hemoglobin levels in sickle cell disease?
Hemolysis, or the breakdown of red blood cells, is a major reason for low hemoglobin in sickle cell disease. This happens because the abnormal hemoglobin S makes red blood cells more likely to break down.
What is the role of hemoglobin F in modifying disease severity in sickle cell disease?
Hemoglobin F, or fetal hemoglobin, is very important in sickle cell disease. More of it means less severe disease and fewer problems.
How does hemoglobin concentration impact clinical symptoms in sickle cell disease?
The amount of hemoglobin directly affects symptoms in sickle cell disease. Lower levels mean a higher risk of organ damage and sickle cell crisis.
What is the purpose of hemoglobin electrophoresis in diagnosing and monitoring sickle cell disease?
Hemoglobin electrophoresis is key for diagnosing and tracking sickle cell disease. It shows different hemoglobin types and tracks changes over time.
What factors can influence hemoglobin levels in sickle cell disease?
Several things can affect hemoglobin levels in sickle cell disease. These include dehydration, oxidative stress, and the amount of hemoglobin S. All these can change how severe the anemia is.
How do blood transfusions help manage hemoglobin levels in sickle cell disease?
Blood transfusions are very important for managing hemoglobin levels in sickle cell disease. They increase normal red blood cells and lower the risk of complications.
What are the therapeutic approaches to increasing hemoglobin in sickle cell disease?
To increase hemoglobin in sickle cell disease, treatments include hydroxyurea therapy. It boosts hemoglobin F production. Gene therapies are also being explored to fix the genetic defect.
How can managing anemia help prevent complications in sickle cell disease?
Managing anemia is key to avoiding complications in sickle cell disease. It reduces the risk of organ damage and sickle cell crisis, improving life quality.
What is the average hemoglobin concentration in sickle cell anemia?
The average hemoglobin in sickle cell anemia is around 8 g/dL. But, it can vary based on individual factors and disease severity.
References
- Centers for Disease Control and Prevention. (2024). Sickle cell disease data & statistics. https://www.cdc.gov/sickle-cell/data/index.html