Being diagnosed with 3 vessel coronary artery disease can be scary. It’s a serious condition that affects all three major coronary arteries. This can lead to heart problems.
Studies have found that this disease raises the risk of heart issues. It’s important to know about its symptoms, how it differs, and how to treat it.
At Liv Hospital, we offer top-notch care. Our team uses the latest evidence and care with compassion. We make sure our patients get the best treatment for their heart condition.
Key Takeaways
- Understanding 3 vessel coronary artery disease is key to managing it well.
- This condition greatly increases the risk of heart problems.
- There are advanced treatments available to manage it.
- Putting the patient first is vital for successful treatment.
- Liv Hospital offers complete care for patients from around the world.
Understanding Coronary Artery Disease Basics
Let’s dive into coronary artery disease basics. We’ll look at the role of coronary arteries and how atherosclerosis develops. Coronary artery disease (CAD) happens when the coronary arteries, which supply blood to the heart, get blocked by plaque.
The Role of Coronary Arteries in Heart Function
The coronary arteries are key to the heart’s health. They bring oxygen and nutrients to the heart muscle. The heart needs blood constantly to work well.
The coronary arteries branch from the aorta and cover the heart’s surface. This ensures every part of the heart gets the blood it needs.
Good blood flow through the coronary arteries is vital. Any blockage can cause chest pain, heart attacks, or serious heart problems.
How Atherosclerosis Develops
Atherosclerosis is the main cause of coronary artery disease. It starts with cholesterol and fatty substances building up in the arteries. Over time, this plaque hardens and narrows the arteries, reducing blood flow to the heart.
Many factors can lead to atherosclerosis, like high blood pressure, smoking, high cholesterol, and diabetes. As plaque builds, arteries become stiff and narrow, making it hard for the heart to get the blood it needs.
Progression from Single to Multiple Vessel Disease
Coronary artery disease can affect one or more arteries. Single-vessel disease happens when one artery is affected. But, as the disease gets worse, it can involve multiple arteries, leading to three-vessel coronary artery disease.
The disease spreads as atherosclerosis and risk factors build up. When more arteries are involved, the risk of heart problems grows. Early diagnosis and treatment are key.
Grasping these basics helps us understand coronary artery disease’s complexities. It shows why managing risk factors is so important to prevent it from getting worse.
What Is 3 Vessel Coronary Artery Disease?
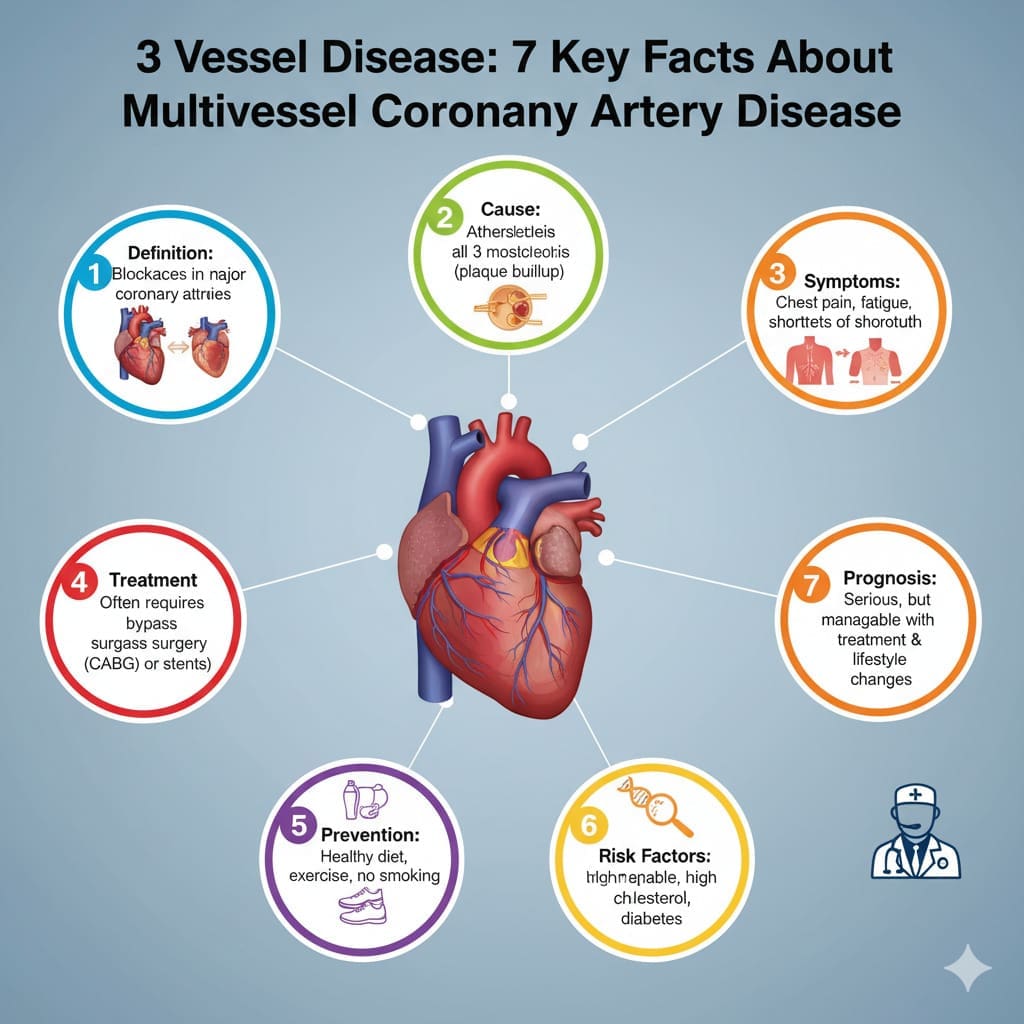
Understanding 3 vessel coronary artery disease is key to keeping your heart healthy. This condition means big blockages in three main arteries that supply blood to the heart.
Definition and Classification
Three-vessel coronary artery disease, or MVCAD, is when big blockages are found in three main arteries. Doctors use tests like coronary angiography to see how bad these blockages are. This helps them figure out how serious it is.
The severity of 3 vessel CAD can differ. Some people have more severe blockages than others. Knowing how bad it is helps doctors choose the best treatment. Treatments can range from medicine to surgery.
Prevalence and Recent Statistics
Recent studies show that 3 vessel CAD affects up to 25 percent of people needing heart interventions. This shows how important it is to manage this condition well.
Studies from heart registries and trials give us important information. They help doctors understand how common 3 vessel CAD is. This knowledge helps them create better treatments for patients.
Terminology: Triple Vessel Disease and MVCAD
The terms “triple vessel disease” and “multivessel coronary artery disease” (MVCAD) are often used the same way. Knowing the terms is important for clear talk between doctors and patients.
“3 vessel coronary artery disease” means blockages in three main arteries. MVCAD can mean blockages in two or more arteries. Being clear about the terms helps make sure patients get the right care.
Comparing Different Forms of Multivessel CAD
It’s key to know the differences between single, double, and 3 vessel CAD to find the best treatments. Multivessel coronary artery disease (CAD) happens when many coronary arteries get blocked. This reduces blood flow to the heart.
Single Vessel vs. Double Vessel Disease
Single vessel disease affects one artery, while double vessel disease hits two. Research shows that more vessels affected means more complex disease and higher risks. People with double vessel disease face a higher risk of heart attacks and death than those with single vessel disease. A study in Nature found that multivessel CAD has a worse prognosis than single vessel disease.
The difference between single and double vessel disease isn’t just about the number of arteries. It’s also about the disease’s impact on the heart. As disease moves from single to double vessel, risks grow, needing more aggressive treatment.
3 Vessel CAD vs. 2 Vessel CAD Outcomes
Outcomes are worse for 3 vessel CAD than for 2 vessel CAD. This is because 3 vessel CAD shows a more severe blockage. Those with 3 vessel CAD face a higher risk of heart attacks and need for more procedures. Treating 3 vessel CAD often requires a detailed plan, including medicine, lifestyle changes, and procedures.
Left Main Coronary Artery Disease Considerations
Left main coronary artery disease is very risky because it affects a big part of the heart. The left main artery supplies a lot of the heart muscle. Left main disease is seen as more critical than other CAD types because of its impact on the heart. Deciding how to treat left main disease is complex, often involving a team to choose between CABG or PCI.
In summary, understanding the differences in multivessel CAD is vital for effective treatment. As CAD gets more complex, treatments must be more aggressive and tailored to the disease’s severity.
Pathophysiology of 3 Vessel Coronary Artery Disease
Understanding 3 vessel coronary artery disease is key to good treatment. It’s a complex mix of factors that hurt our heart health.
Atherosclerotic Process in Multiple Vessels
Atherosclerosis in many coronary vessels is a big part of 3 vessel disease. It’s when plaque builds up in artery walls, making them hard and narrow. This happens because of lipid metabolism disorders, inflammation, and endothelial dysfunction.
As atherosclerosis grows in many vessels, it blocks blood flow to the heart. This can cause ischemia, which is worse when the heart needs more oxygen.
Impact on Cardiac Blood Flow and Function
3 vessel coronary artery disease really affects cardiac blood flow and function. With many vessels blocked, the heart can’t get enough blood. This leads to symptoms like angina, shortness of breath, and fatigue, mostly when we’re active.
| Vessel Involvement | Impact on Cardiac Blood Flow | Symptoms and Complications |
|---|---|---|
| Single Vessel | Mild to moderate reduction | May be asymptomatic or mild angina |
| Double Vessel | Moderate to severe reduction | Angina, shortness of breath |
| Three Vessel | Severe reduction | Frequent angina, heart failure symptoms |
In summary, 3 vessel coronary artery disease is a complex issue. It affects many vessels, impacting blood flow and heart function. Knowing this helps us find better ways to manage it.
Risk Factors and Causes
The risk factors for 3 vessel coronary artery disease include traditional cardiovascular risk factors, genetic predisposition, and lifestyle contributors. Knowing these factors helps assess individual risk and take preventive steps.
Traditional Cardiovascular Risk Factors
Traditional cardiovascular risk factors are key in developing 3 vessel coronary artery disease. These include:
- Hypertension: High blood pressure damages blood vessel linings, making them more prone to blockage.
- Hyperlipidemia: High levels of LDL cholesterol can cause plaque in arteries.
- Diabetes Mellitus: Diabetes greatly increases the risk of coronary artery disease by affecting blood vessels and nerves.
| Risk Factor | Impact on CAD |
|---|---|
| Hypertension | Damages blood vessel lining, increasing blockage risk |
| Hyperlipidemia | Contributes to plaque formation |
| Diabetes Mellitus | Affects blood vessels and nerves, increasing CAD risk |
Genetic Predisposition
Genetic factors greatly influence the risk of coronary artery disease. A family history of heart disease, even at a young age, is a strong indicator of genetic predisposition.
“A family history of coronary artery disease, even in first-degree relatives, increases the risk of developing the condition.”
Lifestyle Contributors
Lifestyle factors also play a big role in developing 3 vessel coronary artery disease. These include:
- Smoking: Tobacco use harms the cardiovascular system and raises CAD risk.
- Physical Inactivity: Not exercising regularly can lead to obesity, hypertension, and other cardiovascular risks.
- Unhealthy Diet: Eating a diet rich in saturated fats, cholesterol, and sodium increases CAD risk.
By understanding and addressing these risk factors, individuals can lower their chance of getting 3 vessel coronary artery disease and its complications.
Signs, Symptoms and Complications
It’s key to know the signs and symptoms of 3 vessel coronary artery disease early. This condition can affect a person’s life quality a lot. Knowing the symptoms is the first step to getting help.
Common Presenting Symptoms
People with 3 vessel coronary artery disease often feel chest pain, or angina. They might also have trouble breathing. This happens because the heart doesn’t get enough oxygen-rich blood.
Other signs include feeling very tired, dizzy, or having irregular heartbeats. It’s important to notice these signs. If they don’t go away or get worse, see a doctor.
Emergency Warning Signs
Some symptoms need immediate help. Look out for severe chest pain or pressure that lasts more than a few minutes. Also, watch for trouble breathing or pain in the arms, back, neck, jaw, or stomach.
If you see these signs, call for emergency help right away. Quick action can make a big difference in treatment and outcomes.
Long-term Complications and Mortality Risk
Not treating 3 vessel coronary artery disease can lead to serious problems. These include heart failure, arrhythmias, and a higher risk of heart attack.
| Complication | Description | Mortality Risk |
|---|---|---|
| Heart Failure | The heart’s inability to pump enough blood to meet the body’s needs. | High |
| Arrhythmias | Abnormal heart rhythms that can be life-threatening. | Moderate to High |
| Heart Attack | A blockage of blood flow to the heart, causing damage to the heart muscle. | High |
Knowing about these risks shows why managing 3 vessel coronary artery disease is so important. It can be done through lifestyle changes, medicine, and sometimes surgery.
Diagnosis and Assessment Methods
We use many tools to accurately diagnose 3 vessel coronary artery disease. Diagnosing this condition involves non-invasive tests, invasive assessments, and risk tools. These help us understand the disease’s extent and guide treatment.
Non-invasive Diagnostic Tests
Non-invasive tests are often the first step in diagnosing coronary artery disease. These include:
- Stress Test: Checks heart function under stress, usually through exercise or medication.
- Echocardiogram: Uses sound waves to create heart images, checking its structure and function.
- Coronary Computed Tomography Angiography (CCTA): Uses CT technology to get detailed images of the coronary arteries.
These tests help spot issues and decide if more invasive tests are needed.
Coronary Angiography and Invasive Assessment
Coronary angiography is the top choice for diagnosing coronary artery disease. It involves:
- Cardiac Catheterization: A catheter is inserted into an artery and guided to the coronary arteries.
- Angiography: Contrast dye is injected, and X-ray images are taken to see the coronary arteries.
This invasive test gives detailed info on coronary artery blockages.
Risk Stratification Tools
Risk tools help us understand the risk of bad outcomes in patients with 3 vessel coronary artery disease. These include:
- SYNTAX Score: A scoring system that checks the complexity of coronary artery disease.
- Heart Team Assessment: A team evaluates the patient’s condition and picks the best treatment.
By using these tools, we can better understand the patient’s risk and plan the right treatment.
Treatment Options for 3 Vessel Coronary Artery Disease
Treating 3 vessel coronary artery disease requires a mix of medical management and revascularization strategies. We’ll dive into these methods, looking at how they handle this complex condition.
Medical Management Approaches
Medical management is key in treating 3 vessel coronary artery disease. It aims to lessen symptoms, slow disease growth, and boost quality of life. Important parts include:
- Pharmacological Therapy: Using drugs like beta-blockers, ACE inhibitors, statins, and antiplatelet agents to manage symptoms and risks.
- Lifestyle Modifications: Helping patients live healthier by quitting smoking, eating better, and exercising regularly.
- Risk Factor Management: Managing high blood pressure, diabetes, and high cholesterol through lifestyle changes and medicine.
Revascularization Strategies
Revascularization aims to improve blood flow to the heart, easing symptoms and possibly increasing survival chances. The main strategies are:
- Percutaneous Coronary Intervention (PCI): A less invasive method using angioplasty and stenting to open blocked arteries.
- Coronary Artery Bypass Grafting (CABG): A surgery that bypasses blocked arteries with grafts.
Choosing between PCI and CABG depends on the heart’s anatomy, patient health, and personal preference.
Patient-Specific Factors Influencing Treatment Decisions
When picking a treatment, we look at several factors unique to each patient, such as:
- Clinical Presentation: How severe the symptoms are and if there’s an acute coronary syndrome.
- Coronary Anatomy: How widespread and complex the heart disease is.
- Comorbid Conditions: Other health issues that might affect treatment choices.
- Patient Preference: What the patient values and prefers in treatment.
By focusing on these factors, we can create personalized treatment plans. This approach helps improve outcomes for 3 vessel coronary artery disease.
Conclusion
Understanding 3 vessel coronary artery disease is key for helping international patients get the best care. This condition blocks all three major coronary arteries. It’s a big risk to heart health and overall cardiovascular health.
We’ve looked at the main facts and differences of 3 vessel coronary artery disease. This includes its definition, how common it is, and its effect on the heart. We’ve also talked about the treatments available, like medicine and procedures to open blocked arteries. It’s important to consider each patient’s needs when choosing a treatment.
By understanding 3 vessel coronary artery disease and its treatment, doctors can give better care to patients. This knowledge helps us improve heart health results. It also supports international patients as they go through their treatment.
What is 3 vessel coronary artery disease?
3 vessel coronary artery disease is when all three main coronary arteries get blocked. This greatly reduces blood flow to the heart.
How does 3 vessel coronary artery disease differ from single or double vessel disease?
3 vessel disease affects more areas, making it more serious than single or double vessel disease. Single or double vessel disease impacts fewer arteries.
What are the risk factors for developing 3 vessel coronary artery disease?
Risk factors include high blood pressure, high cholesterol, diabetes, and smoking. Family history and lifestyle also play a role.
What are the common symptoms of 3 vessel coronary artery disease?
Symptoms include chest pain, shortness of breath, and fatigue. Pain in the arms, back, neck, jaw, or stomach is also common.
How is 3 vessel coronary artery disease diagnosed?
Doctors use stress tests and echocardiograms first. Then, they might do coronary angiography to see the arteries.
What are the treatment options for 3 vessel coronary artery disease?
Treatment includes medicines to control symptoms and slow the disease. They also do procedures like CABG and PCI to open blocked arteries.
What is the significance of left main coronary artery disease in the context of 3 vessel coronary artery disease?
Left main disease is very serious. It can greatly affect patients with 3 vessel disease. It often needs aggressive treatment.
Can lifestyle changes help manage 3 vessel coronary artery disease?
Yes, making healthy lifestyle choices can help. Eating right, exercising, quitting smoking, and managing stress can slow the disease.
What are the long-term complications of 3 vessel coronary artery disease?
Long-term risks include heart attacks, heart failure, and arrhythmias. These risks highlight the need for ongoing care and monitoring.
How does the pathophysiology of 3 vessel coronary artery disease impact cardiac function?
Atherosclerosis in multiple arteries reduces blood flow to the heart. This can lead to heart problems, symptoms, and complications.
References
Britannica: Coronary Artery Disease (Science Article)




































