At LivHospital, we know there’s confusion about Acute Lymphocytic Leukemia (ALL) and Acute Lymphoblastic Leukemia. These terms mean the same thing. They describe a fast-growing blood cancer that starts in the bone marrow from immature lymphoid cells. Learn acute lymphocytic leukemia vs acute lymphoblastic leukemia differences, causes, and key diagnostic facts.
In this article, we’ll look at the main differences, symptoms, how to diagnose it, and treatment options. We aim to give you a full understanding of what to expect. Our goal is to help you navigate the complexities of ALL with kindness and clarity.
Key Takeaways
- Acute Lymphocytic Leukemia (ALL) and Acute Lymphoblastic Leukemia are terms used interchangeably.
- ALL is a rapidly progressing blood cancer originating from immature lymphoid cells.
- The condition requires prompt diagnosis and treatment.
- Understanding the symptoms and diagnosis process is key for effective treatment.
- Treatment options vary based on individual patient needs.
The Truth About Terminology: Same Disease, Different Names

Learning about Acute Lymphoblastic Leukemia (ALL) starts with its history and how names have changed. The names for this disease have shifted as we’ve learned more about it. This change shows how our understanding and tools for diagnosing have grown.
Medical Nomenclature Evolution
Changes in how we talk about ALL come from better diagnostic tools and a deeper understanding of the disease. At first, doctors looked at the disease’s appearance. But with new tests like immunophenotyping and genetic analysis, our way of classifying it has gotten more detailed.
“The terminology used in medicine is not static; it evolves as our understanding of diseases improves,” reflecting the dynamic nature of medical science. This change is clear in ALL, where the difference between ‘lymphocytic’ and ‘lymphoblastic’ has become clearer over time.
Historical Context of ALL Terminology
In the past, ‘lymphocytic’ and ‘lymphoblastic’ described different parts of the disease. ‘Lymphoblastic’ points to the young cells found in this leukemia. ‘Lymphocytic’ refers to the type of cells involved. The mix-up in these terms comes from the disease’s complexity and how it was first classified.
Current Usage in Clinical Settings
Today, both terms are used, based on the situation and treatment plans. The split into B-cell ALL and T-cell ALL helps doctors decide on treatments. This dual naming can be confusing, but it shows how complex ALL is.
Knowing the history and current use of ALL terms helps both patients and doctors. As we learn more about ALL, the names used will likely change again. This will reflect the latest in science and medicine.
Acute Lymphocytic Leukemia vs Acute Lymphoblastic Leukemia: Understanding the Basics
To understand Acute Lymphocytic Leukemia, we need to know its definition, how it progresses, and its effects on the body. We will cover the basics to give a clear picture.
Definition and Pathophysiology
Acute Lymphocytic Leukemia (ALL) is a cancer that affects the lymphocytes, key to our immune system. It’s marked by the fast growth of immature lymphocytes that can’t work right. These cells build up in the bone marrow and blood, stopping normal blood cell production.
ALL starts with the cancerous change of lymphoid cells, causing them to grow out of control. This messes up how blood is made, leading to various symptoms.
Rapid Progression Characteristics
ALL grows fast, with symptoms appearing in weeks or months. It can cause tiredness, weight loss, and frequent infections. This is because of the buildup of immature lymphocytes in the bone marrow and other organs.
Because ALL progresses quickly, it’s vital to diagnose and treat it fast. This helps avoid serious problems and improves chances of recovery. Knowing how the disease works helps doctors find the best treatments.
Impact on Normal Blood Cell Production
The growth of leukemic cells in ALL harms normal blood cell making. The bone marrow is filled with immature lymphocytes, reducing red blood cells, platelets, and normal white blood cells.
This problem in blood making leads to anemia, low platelets, and a higher risk of infections. It shows why quick and effective treatment is needed to fix blood cell production.
Classification Systems: B-Cell and T-Cell Variants
Acute Lymphocytic Leukemia (ALL) is split into different types based on where the cancer starts. This is key for picking the right treatment. The main split is between B-cell and T-cell ALL, based on the cell type.
B-Cell ALL Characteristics and Prevalence
B-cell ALL is the most common type, mostly in kids. It grows from B-cell lymphoblasts in the bone marrow. B-cell ALL is split further by genetic changes, which affect how well it does and how it’s treated.
T-Cell ALL Features and Distinctions
T-cell ALL starts from T-cell lymphoblasts and often hits older kids and young adults. It’s seen as a more serious and fast-moving disease than B-cell ALL.
Implications for Treatment Selection
The choice between B-cell and T-cell ALL treatments is big. Both need strong chemotherapy, but the exact plan can change based on the type and the patient. Knowing these differences helps doctors give the best care.
Epidemiology and Risk Factors
Studying ALL helps doctors and scientists find better ways to treat it. This is important for both kids and adults with the disease.
Annual Incidence in the United States
Every year, about 6,540 new cases of ALL happen in the U.S. This shows how big of a health issue it is.
Age Distribution: Children vs Adults
Children are more likely to get ALL than adults. It’s most common in kids aged 2-5. Adults over 65 also get it a lot.
Known Risk Factors and Genetic Predispositions
Things like too much radiation and certain genetic conditions raise the risk. Some genetic problems make it more likely to get ALL.
| Risk Factor | Description | Impact |
| Genetic Conditions | Presence of specific genetic syndromes | Increased risk of ALL |
| Radiation Exposure | High levels of ionizing radiation | Elevated risk of leukemia |
| Age | Children aged 2-5 years and adults over 65 | Higher incidence of ALL |
Clinical Manifestations and Warning Signs
It’s important to know the signs of Acute Lymphocytic Leukemia (ALL) for early treatment. We’ll talk about the common symptoms and warning signs. This helps patients get medical help quickly.
Early Symptoms of Acute Leukemia
The first signs of ALL can be vague. They might include fatigue, bone pain, fever, dizziness, shortness of breath, bruising, pale skin, frequent or heavy bleeding, and recurrent infections. These happen because cancer cells in the bone marrow stop normal blood cell production.
Complications from Bone Marrow Dysfunction
Bone marrow problems in ALL cause many issues. These include:
- Anemia, leading to tiredness and weakness
- Thrombocytopenia, causing bruising and bleeding
- Neutropenia, making infections more likely
These problems can really affect a person’s life. They need to see a doctor right away.
When to Seek Immediate Medical Attention
If you’re feeling very tired, have unexplained bleeding, or keep getting infections, get medical help. Early treatment of ALL can greatly improve chances of recovery.
Diagnostic Approaches and Disease Staging
Getting a correct diagnosis of Acute Lymphoblastic Leukemia is key for good treatment. We use blood tests, bone marrow checks, and special tests to fully understand the disease.
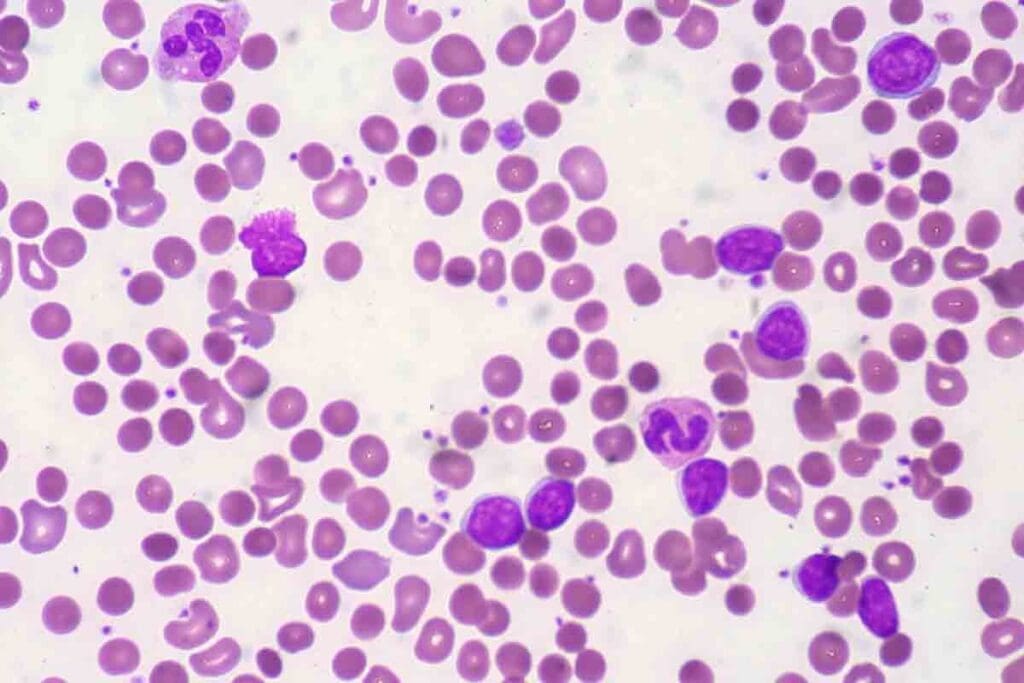
Initial Blood Work and Laboratory Findings
The first step is blood work. This includes a complete blood count (CBC) to check blood cell levels. If the results show anemia, thrombocytopenia, or leukocytosis, it might mean leukemia.
Then, we do more tests to look at the blood cells closely. These tests help figure out the type of leukemia and its details.
| Laboratory Test | Purpose | Significance in ALL Diagnosis |
| Complete Blood Count (CBC) | Assess levels of different blood cells | Identifies abnormalities such as anemia or thrombocytopenia |
| Blood Smear | Examine morphology of blood cells | Helps identify abnormal cells |
| Flow Cytometry | Analyze cell surface markers | Critical for diagnosing ALL and distinguishing it from other leukemias |
Bone Marrow Examination Procedures
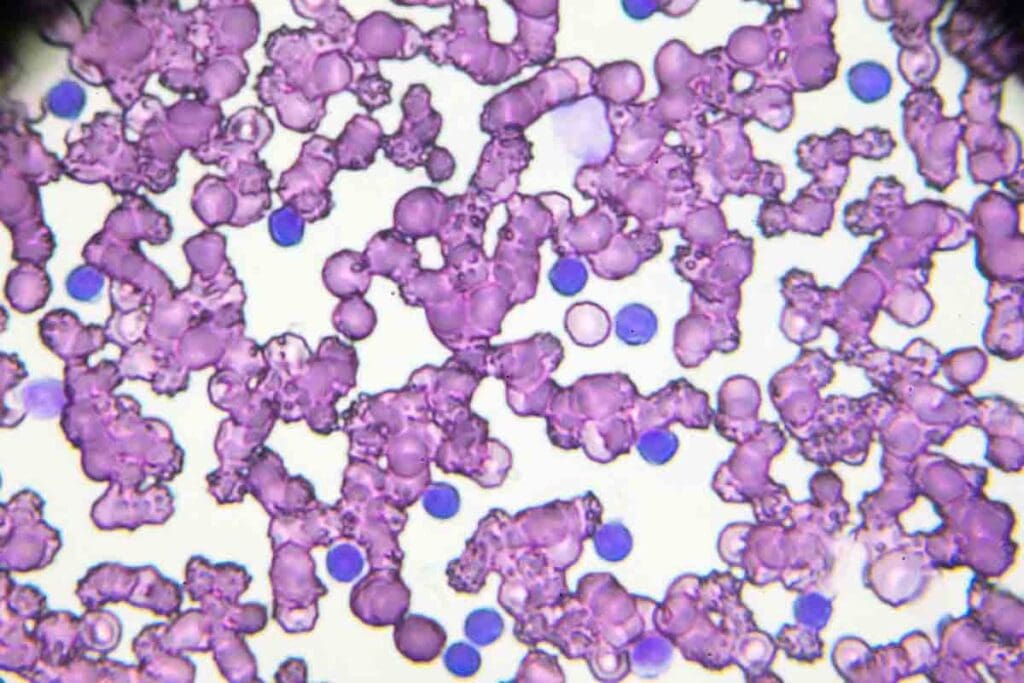
Bone marrow tests are key for ALL diagnosis. We take a sample of bone marrow for a check. Finding lymphoblasts in the bone marrow shows ALL.
Advanced Diagnostic Techniques
Tests like flow cytometry, cytogenetics, and molecular diagnostics are very important. They help us understand the leukemia’s genetics. This is vital for making a treatment plan.
By using blood work, bone marrow tests, and advanced tests, we can accurately diagnose ALL. Then, we can plan a good treatment.
Comprehensive Treatment Protocols
Managing ALL needs a detailed treatment plan with several phases. We’ll cover the main parts of these plans. This will give you an idea of the current best care for ALL.
Phase 1: Induction Therapy
Induction therapy is the first step. It aims to clear leukemia cells from the bone marrow and blood. This phase is key and often includes strong chemotherapy.
We mix different drugs to hit the leukemia cells hard.
Phase 2: Consolidation Treatment
After reaching remission, consolidation therapy comes next. It targets any hidden leukemia cells that could grow back. This phase is vital for better long-term survival.
Phase 3: Maintenance Therapy
Maintenance therapy is the last phase. It keeps remission going and stops relapse. It uses less strong chemotherapy for a longer time, sometimes up to three years.
Emerging Treatments and Clinical Trials
New treatments and clinical trials bring hope for ALL patients. We’re always looking into new therapies like targeted and immunotherapy. They might improve patient outcomes.
Joining clinical trials can give you access to new treatments not available yet.
It’s important to know about ALL’s treatment phases for patients and families. We aim to offer the best care with the latest medical science.
Prognosis and Survival Statistics
Knowing the prognosis for Acute Lymphocytic Leukemia (ALL) is key for patients and their families. The outlook changes a lot based on age, how well treatment works, and the leukemia’s specific traits.
Five-Year Survival Rate Analysis
The five-year survival rate for ALL has gone up a lot, now over 70 percent. This boost comes from better treatments and a deeper understanding of the disease.
| Age Group | Five-Year Survival Rate |
| Children | 85-90% |
| Adults | 40-50% |
Prognostic Factors Affecting Outcomes
Many things can change how likely someone is to survive ALL. These include the patient’s age, how many white blood cells they have at first, genetic issues, and how well they do with the first treatment. People with certain genetic markers or who do well with the first treatment usually have a better chance.
Relapse Risks and Management
Relapse is a big worry in ALL, mainly for those who don’t fully recover or are at high risk. Keeping an eye out for signs of relapse and changing treatment plans is key to better results.
By knowing these factors and survival rates, patients and doctors can make better choices about treatment and managing ALL.
LivHospital’s Approach to ALL Treatment
At LivHospital, we treat ALL with the latest medical tech and care. Getting a diagnosis of Acute Lymphocytic Leukemia can feel scary. We’re here to support you every step of the way.
Multidisciplinary Treatment Teams
Our teams at LivHospital are made up of experts from different fields. They work together to create treatment plans that fit each patient’s needs. This team effort means our patients get the best care possible.
Up-to-Date Protocol Implementation
We always use the newest ALL treatment methods. Our team keeps learning to offer the latest therapies. This helps us improve our patients’ chances of a good outcome.
International Standards and Quality Care
LivHospital follows global care standards. This ensures our patients get top-notch treatment. We focus on keeping our care safe and efficient.
Patient Experience and Support Services
We know care is more than just treatment. Our support services help with emotional, psychological, and practical needs. We aim to care for the whole person, not just the illness.
Conclusion: Navigating an ALL Diagnosis
Getting a diagnosis of acute lymphocytic leukemia (ALL) means you need to know a lot about it. We’ve talked about how ALL and acute lymphoblastic leukemia are the same thing. It’s important for patients to understand this to make good choices about their treatment.
Getting treatment quickly is key to fighting ALL. This is because ALL is a fast-moving cancer. We’ve looked at the different treatments, like induction and maintenance therapy. A team of doctors working together is also very important.
At LivHospital, we’re here to help patients with ALL. Our team creates treatment plans that are just right for each patient. Knowing about ALL and the treatments available helps patients feel more in control. They can face their treatment with hope and confidence.
FAQ
What is the difference between acute lymphocytic leukemia and acute lymphoblastic leukemia?
Acute lymphocytic leukemia and acute lymphoblastic leukemia are the same disease. The terms are often used the same way. The difference is just in the words used, not the disease itself.
What is acute lymphoblastic leukemia (ALL)?
Acute lymphoblastic leukemia (ALL) is a blood and bone marrow cancer. It makes too many immature white blood cells. This stops the body from making normal blood cells.
What are the symptoms of acute lymphoblastic leukemia?
Symptoms of ALL include feeling very tired, looking pale, and getting sick often. You might also bruise easily, bleed a lot, or have swollen lymph nodes. It’s important to see a doctor if you notice these signs.
How is acute lymphoblastic leukemia diagnosed?
Doctors use many tests to find ALL. These include blood tests, bone marrow exams, and imaging studies. They also do genetic tests.
What are the treatment phases for acute lymphoblastic leukemia?
ALL treatment has three main parts. First, there’s induction therapy to get the cancer into remission. Then, there’s consolidation treatment to kill any cancer cells left. Lastly, there’s maintenance therapy to keep the cancer from coming back.
What are the survival statistics for acute lymphoblastic leukemia?
Survival rates for ALL depend on several things. These include how old you are, your genes, and how well you respond to treatment. Thanks to new treatments, more people, even kids, are living longer.
What is the role of clinical trials in treating acute lymphoblastic leukemia?
Clinical trials are key in finding better treatments for ALL. They test new therapies and improve current ones. They also give patients access to new treatments.
How does LivHospital approach the treatment of acute lymphoblastic leukemia?
LivHospital focuses on top-notch care for ALL patients. They use teams of doctors, follow the latest treatment plans, and meet international care standards.
What is the significance of classification into B-cell and T-cell variants in ALL?
Knowing if you have B-cell or T-cell ALL matters a lot. It helps doctors decide how to treat you and what to expect. B-cell ALL is more common in kids, while T-cell ALL is more aggressive.
Are there known risk factors for developing acute lymphoblastic leukemia?
Yes, there are. Risk factors include your genes, some chemicals, and radiation therapy. Knowing these can help find and treat ALL early.
References
Pui, C.-H., Yang, J. J., Hunger, S. P., Pieters, R., Schrappe, M., Biondi, A., … & Mullighan, C. G. (2015). Childhood acute lymphoblastic leukemia: Progress through collaboration. Journal of Clinical Oncology, 33(27), 2938–2948. https://pubmed.ncbi.nlm.nih.gov/26304874/




































