Last Updated on November 27, 2025 by Bilal Hasdemir

Undergoing a myomectomy can be a significant decision, and understanding the implications of scars after the procedure is crucial for patients. We understand that concerns about scarring and recovery are paramount.
At Liv Hospital, we are committed to providing patient-centered care and utilizing minimally invasive techniques to minimize scarring and enhance the healing process. According to doctor laparoscopic myomectomy offers numerous benefits, including smaller scars and faster recovery.
Robotic myomectomy scars are typically smaller and less visible compared to those from open abdominal myomectomies, often consisting of tiny incisions on the abdomen. This is because the procedure uses minimally invasive techniques, resulting in a quicker recovery time.
Key Takeaways
- Robotic myomectomy scars are smaller and less visible.
- Minimally invasive techniques reduce scarring.
- Faster recovery is a significant benefit.
- Proper scar management can aid in healing.
- A healthy diet promotes faster recovery.
- Avoiding strenuous activities aids in recovery.
- Internal scarring from hysteroscopic myomectomy is rare.
What is a Myomectomy: Removing Fibroids While Preserving Fertility

Myomectomy is a surgical procedure that has gained significant attention for its ability to remove uterine fibroids while preserving fertility. This operation is particularly important for women who wish to maintain their reproductive capabilities. By conserving the uterus, myomectomy provides a viable solution for women suffering from fibroids.
According to medical experts like doctor laparoscopic myomectomy is a minimally invasive technique that achieves this goal by removing uterine fibroids while conserving the uterus. This approach is especially beneficial for women who want to preserve their fertility. The procedure involves the precise removal of myomas, ensuring minimal damage to the surrounding uterine tissue.
The Purpose of Myomectomy Procedures
The primary purpose of a myomectomy is to remove symptomatic uterine fibroids, which can cause a range of symptoms including heavy menstrual bleeding, pelvic pain, and pressure on surrounding organs. By eliminating these fibroids, myomectomy can significantly improve a woman’s quality of life. This procedure is particularly beneficial for women who are experiencing fertility issues due to the presence of fibroids.
Common Reasons Women Choose Myomectomy
Women choose myomectomy for various reasons, primarily to alleviate symptoms associated with uterine fibroids and to preserve their fertility. Some women may also opt for this procedure due to the potential for reduced recovery time compared to more invasive surgical options. The decision to undergo myomectomy is often made after careful consideration of the potential benefits and risks.
| Reasons for Choosing Myomectomy | Benefits |
|---|---|
| Symptom relief | Reduced heavy menstrual bleeding |
| Fertility preservation | Ability to conceive and carry a pregnancy |
| Minimally invasive options | Reduced recovery time and scarring |
By understanding the purpose and benefits of myomectomy, women can make informed decisions about their reproductive health. This procedure offers a valuable option for those seeking to remove uterine fibroids while preserving their fertility.
Types of Myomectomy Procedures: Comparing Surgical Approaches
There are multiple surgical approaches to myomectomy, ranging from traditional open surgery to advanced minimally invasive techniques. The choice of procedure depends on several factors, including the size, number, and location of fibroids, as well as the patient’s overall health and personal preferences.
Open Abdominal Myomectomy
Open abdominal myomectomy involves making a single incision in the abdomen to access the uterus. This traditional approach is often used for larger fibroids or when multiple fibroids are present. While it allows for direct visualization and removal of fibroids, it typically results in a longer recovery time compared to minimally invasive methods.
Laparoscopic Myomectomy
Laparoscopic myomectomy is a minimally invasive procedure where several small incisions are made to insert a laparoscope and surgical instruments. This approach offers the benefits of smaller scars, less postoperative pain, and quicker recovery. However, it requires advanced laparoscopic skills and may not be suitable for all patients.
Robotic-Assisted Myomectomy
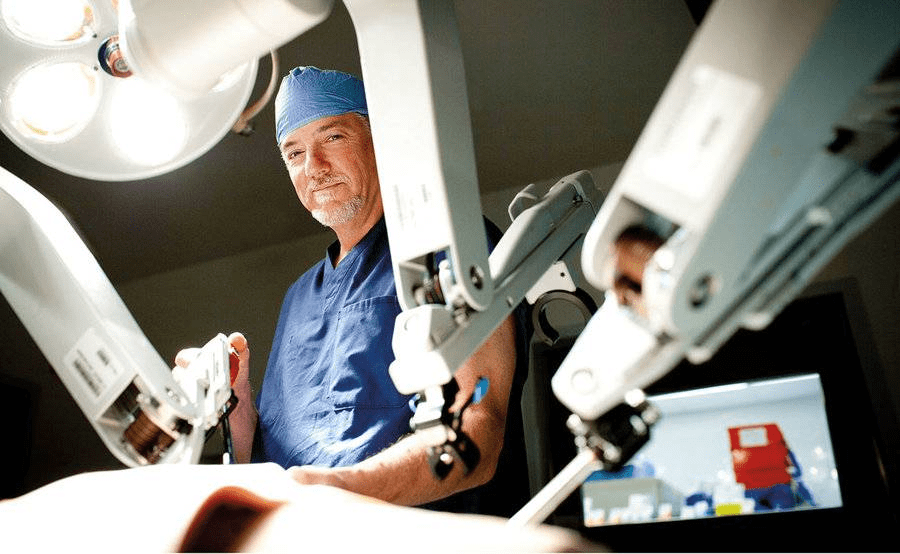
Robotic-assisted myomectomy utilizes a robotic system to enhance the surgeon’s capabilities, offering improved precision, flexibility, and visualization. This advanced technique allows for complex procedures to be performed through small incisions, potentially reducing recovery time and scarring. Robotic technology has revolutionized myomectomy by providing a high-definition, 3D view of the operating area, enabling surgeons to perform delicate dissections and suturing with enhanced accuracy.
Hysteroscopic Myomectomy
Hysteroscopic myomectomy is a procedure performed through the vagina, using a hysteroscope to visualize the inside of the uterus. It is particularly useful for removing submucosal fibroids that protrude into the uterine cavity. This approach is considered minimally invasive and does not require any external incisions, resulting in no visible scarring and typically a shorter recovery period.
Each of these myomectomy procedures has its indications, benefits, and potential drawbacks. The choice of surgical approach depends on various factors, including the patient’s specific condition, the surgeon’s expertise, and the available technology. By understanding the different types of myomectomy procedures, patients can make informed decisions about their treatment options.
- Open Abdominal Myomectomy: Traditional approach with a single abdominal incision.
- Laparoscopic Myomectomy: Minimally invasive with several small incisions.
- Robotic-Assisted Myomectomy: Advanced robotic technology for enhanced precision.
- Hysteroscopic Myomectomy: Procedure performed through the vagina, no external incisions.
Robotic Myomectomy Scars: Size, Appearance and Healing Process
When it comes to robotic myomectomy, patients often wonder about the size, appearance, and healing process of their scars. Robotic myomectomy scars are generally smaller and less visible compared to those from traditional open abdominal myomectomies. In this section, we will explore the typical incision patterns and sizes associated with robotic myomectomy, as well as how robotic technology creates smaller scars. We will also provide a visual comparison to traditional surgery scars, highlighting the benefits of robotic myomectomy.
Typical Incision Patterns and Sizes
Robotic myomectomy involves making several small incisions in the abdomen, typically ranging from 0.5 to 1.5 cm in length. These incisions are strategically placed to minimize visible scarring. The exact number and size of incisions can vary depending on the complexity of the procedure and the surgeon’s technique.
Key characteristics of robotic myomectomy incisions include:
- Small size, usually between 0.5 to 1.5 cm
- Strategic placement to minimize visible scarring
- Typically 3-4 incisions are made
- Incisions are usually made in the lower abdomen
How Robotic Technology Creates Smaller Scars
Robotic technology allows for more precise movements and smaller incisions compared to traditional open surgery. The robotic system’s enhanced dexterity and visualization enable surgeons to perform complex procedures with minimal tissue damage, resulting in smaller scars.
“The use of robotic technology in myomectomy has significantly reduced the size of scars, making it a more appealing option for women concerned about cosmetic outcomes.”
Visual Comparison to Traditional Surgery Scars
To illustrate the difference in scarring between robotic myomectomy and traditional open myomectomy, let’s consider the following comparison:
| Characteristics | Robotic Myomectomy | Traditional Open Myomectomy |
|---|---|---|
| Incision Size | 0.5-1.5 cm | 10-15 cm |
| Number of Incisions | 3-4 | 1 |
| Scar Visibility | Less visible | More visible |
| Healing Time | Faster | Slower |
As shown in the table, robotic myomectomy results in significantly smaller and less visible scars compared to traditional open myomectomy. This is a crucial consideration for many patients when choosing a surgical option.
Key Fact #1: Minimally Invasive Techniques Reduce External Scarring
Minimally invasive techniques have revolutionized the field of myomectomy, significantly reducing external scarring. These advanced surgical methods, particularly robotic myomectomy, offer patients a more cosmetically appealing outcome by minimizing the size and number of incisions.
How Robotic Precision Minimizes Tissue Damage
Robotic precision plays a crucial role in minimizing tissue damage during myomectomy procedures. The robotic system allows surgeons to perform intricate dissections with enhanced accuracy, reducing the risk of unnecessary tissue trauma. This precision not only aids in faster recovery but also contributes to less noticeable scarring.
According to studies on myomectomy outcomes, the use of robotic assistance in surgery can lead to improved patient satisfaction due to the reduced visibility of scars.
Benefits for Cosmetic Outcomes
The benefits of minimally invasive techniques for cosmetic outcomes are significant. By utilizing smaller incisions, these procedures result in less visible scarring. The cosmetic advantages are particularly important for patients who are concerned about the aesthetic impact of surgery.
| Technique | Incision Size | Cosmetic Outcome |
|---|---|---|
| Robotic Myomectomy | 0.5-1 cm | Minimal scarring |
| Laparoscopic Myomectomy | 1-2 cm | Moderate scarring |
| Open Myomectomy | 5-10 cm | Significant scarring |
The table above illustrates the comparative cosmetic outcomes of different myomectomy techniques. As shown, robotic myomectomy offers the most favorable cosmetic results due to its minimally invasive nature.
In conclusion, the use of minimally invasive techniques in myomectomy, particularly robotic myomectomy, significantly reduces external scarring. This not only enhances the cosmetic outcome but also contributes to a quicker recovery and improved patient satisfaction.
Key Fact #2: Hysteroscopic Myomectomy Leaves No External Scars
Unlike traditional surgical methods, hysteroscopic myomectomy is performed internally, resulting in no external scars. This procedure involves removing fibroids through the uterus, making it an attractive option for women who wish to avoid visible scarring.
The Internal Healing Process
The internal healing process after a hysteroscopic myomectomy is generally quick. Since the procedure is minimally invasive and doesn’t involve external incisions, the risk of complications is reduced. Patients typically experience less postoperative discomfort compared to more invasive surgical methods.
After the procedure, the body heals internally. The uterus begins to repair itself, and any internal swelling subsides within a few days. Proper postoperative care is essential to ensure a smooth recovery. Patients are usually advised to avoid strenuous activities and follow specific guidelines provided by their healthcare provider.
Candidates for Scarless Procedures
Hysteroscopic myomectomy is suitable for women with certain types of fibroids. Candidates for this procedure typically have fibroids that are accessible through the uterine cavity. The size, number, and location of the fibroids are critical factors in determining eligibility for hysteroscopic myomectomy.
According to doctor hysteroscopic myomectomy is a procedure that removes fibroids without making external incisions, resulting in no visible scars. This makes it an excellent option for women seeking to minimize the appearance of scarring.
| Candidate Characteristics | Description |
|---|---|
| Fibroid Location | Fibroids within the uterine cavity |
| Fibroid Size | Typically smaller fibroids |
| Number of Fibroids | Single or multiple, depending on location and size |
By understanding the internal healing process and identifying suitable candidates, healthcare providers can offer hysteroscopic myomectomy as a viable option for women seeking to remove fibroids without the concern of external scarring.
Key Fact #3: Recovery Timeline Varies by Procedure Type
The recovery period after a myomectomy can vary significantly depending on the surgical approach used. We understand that patients want to plan their recovery and return to normal activities as smoothly as possible.
Hysteroscopic Recovery (1-2 Weeks)
Hysteroscopic myomectomy, being a minimally invasive procedure, typically allows for quicker recovery. Most patients can return to their normal activities within 1-2 weeks. This procedure involves minimal discomfort and usually doesn’t require an overnight hospital stay.
Laparoscopic and Robotic Recovery (2-4 Weeks)
For laparoscopic and robotic myomectomy, the recovery time is generally longer than hysteroscopic procedures but shorter than open myomectomy. Patients usually take 2-4 weeks to recover and resume their normal activities. The precision of robotic technology can contribute to less tissue trauma, potentially leading to a smoother recovery.
Open Myomectomy Recovery (4-6 Weeks)
Open myomectomy, involving a larger incision, typically requires a longer recovery period. Patients often need 4-6 weeks to heal sufficiently to return to their usual activities. The extended recovery time is due to the more invasive nature of the procedure.
Factors Affecting Individual Healing Time
While general recovery times can be provided, individual healing times can vary based on several factors. These include the patient’s overall health, the size and number of fibroids removed, and the surgeon’s expertise. Additionally, post-operative care and adherence to the surgeon’s instructions play a crucial role in the recovery process.
We emphasize the importance of personalized care and follow-up appointments to monitor the healing process. By understanding the recovery timeline associated with different myomectomy procedures, patients can better prepare for their post-surgery period.
Key Fact #4: Week-by-Week Healing After Robotic Myomectomy
Understanding the recovery process after robotic myomectomy is crucial for patients to manage their expectations and healing journey effectively. We will guide you through the week-by-week healing process, highlighting key milestones and what to expect during your recovery.
First Week: Managing Discomfort and Initial Healing
The first week after robotic myomectomy is characterized by managing discomfort and initial healing. Patients typically experience some pain, bloating, and fatigue.
Weeks 2-3: Increasing Energy and Activity Levels
During weeks 2-3, patients usually start to notice an increase in energy levels and can gradually resume more activities. It’s essential to listen to your body and not overexert yourself, as this can impact the healing process. Gradual progression is key to a successful recovery.
Weeks 4-6: Return to Normal Activities
By weeks 4-6, most patients can return to their normal activities, including work and exercise. However, it’s crucial to continue following the post-operative instructions provided by your healthcare team to ensure a smooth recovery.
Beyond 6 Weeks: Long-term Scar Maturation
After six weeks, the focus shifts to long-term scar maturation. Scars will continue to evolve and mature over several months. Proper wound care and sun protection are vital during this phase to optimize the appearance of the scar.
| Recovery Phase | Key Milestones | Recommendations |
|---|---|---|
| First Week | Managing discomfort, initial healing | Follow post-operative care plan, rest |
| Weeks 2-3 | Increasing energy, resuming activities | Gradually increase activity levels, monitor body |
| Weeks 4-6 | Returning to normal activities | Continue post-operative instructions, resume work/exercise |
| Beyond 6 Weeks | Long-term scar maturation | Proper wound care, sun protection |
Key Fact #5: Scar Healing Follows Four Distinct Biological Phases
Scar healing occurs in four distinct phases, each crucial for optimal recovery. Understanding these phases can help patients better manage their expectations and care for their scars post-robotic myomectomy.
Inflammatory Response Phase (Days 1-5)
During the initial inflammatory response phase, the body begins to heal the wound by increasing blood flow to the area, bringing with it nutrients and cells necessary for repair. This phase is characterized by redness, swelling, and warmth around the incision site.
Proliferation Phase (Days 5-21)
The proliferation phase follows, where the body starts to rebuild tissue. New collagen is formed, and the wound begins to close. This phase is critical for establishing a strong foundation for the scar tissue.
Remodeling Phase (3 Weeks to 6 Months)
In the remodeling phase, the newly formed collagen is reorganized to improve the strength and appearance of the scar. The scar starts to flatten and become less noticeable.
Maturation Phase (6 Months to 2 Years)
The maturation phase is the final stage, where the scar continues to mature and improve in appearance. It can take up to two years for the scar to fully mature and fade.
As noted by a medical professional,
“Understanding the biological phases of scar healing can significantly improve patient outcomes and satisfaction.”
| Phase | Duration | Characteristics |
|---|---|---|
| Inflammatory Response | Days 1-5 | Redness, swelling, warmth |
| Proliferation | Days 5-21 | Tissue rebuilding, collagen formation |
| Remodeling | 3 Weeks to 6 Months | Collagen reorganization, scar flattening |
| Maturation | 6 Months to 2 Years | Scar maturation, fading |
Key Fact #6: Optimal Healing Requires Proper Wound Care and Nutrition
The road to recovery after robotic myomectomy involves not just rest, but also careful wound care and nutritional support. We understand that optimal healing is crucial for patients after myomectomy, and proper wound care and nutrition play a significant role in promoting optimal healing.
Wound Care Essentials
Proper wound care is essential for minimizing the risk of complications and promoting optimal healing. This includes keeping the wound clean and dry, following the doctor’s instructions for dressing changes, and monitoring for signs of infection.
- Keep the wound clean and dry
- Follow the doctor’s instructions for dressing changes
- Monitor for signs of infection
Protecting New Scars from the Sun
Protecting new scars from the sun is crucial for preventing discoloration and promoting optimal healing. We recommend using sun protection measures such as sunscreen with at least SPF 30 and covering the scar with clothing when going outdoors.
- Use sunscreen with at least SPF 30
- Cover the scar with clothing when going outdoors
Nutritional Support for Healing
Adequate nutrition is vital for tissue repair and optimal healing. Key nutrients include protein for tissue repair, vitamin C for collagen synthesis, and zinc for wound healing.
- Protein for tissue repair
- Vitamin C for collagen synthesis
- Zinc for wound healing
Consulting Your Doctor About Scar Concerns
If you have scar concerns, such as redness, swelling, or discharge, it’s essential to consult your doctor. We are here to support you throughout your recovery journey.
Conclusion: Making Informed Decisions About Myomectomy Options
We believe that making informed decisions about myomectomy options is crucial for patients. Understanding the different procedures, including robotic myomectomy, hysteroscopic myomectomy, and laparoscopic myomectomy, enables patients to choose the best option for their individual needs.
Doctor insights and resources on robotic surgery provide valuable information to help patients make informed decisions. By considering factors such as recovery time, scarring, and overall health benefits, patients can select the most suitable myomectomy option.
Ultimately, we empower patients to take control of their care by providing comprehensive information on myomectomy options. This enables them to make informed decisions that align with their personal preferences and health goals.
FAQ
What is the typical size and appearance of robotic myomectomy scars?
Robotic myomectomy scars are typically smaller and less visible compared to those from open abdominal myomectomies, often consisting of tiny incisions on the abdomen.
How do laparoscopic and robotic myomectomy scars compare to open abdominal myomectomy scars?
Laparoscopic and robotic myomectomy scars are generally smaller and less visible due to the use of minimally invasive techniques, reducing external scarring and promoting quicker healing.
Does hysteroscopic myomectomy leave external scars?
No, hysteroscopic myomectomy does not leave external scars, as it involves removing fibroids through the uterus without making external incisions, emphasizing a faster recovery and minimal postoperative discomfort.
What is the average recovery time for hysteroscopic myomectomy?
The average recovery time for hysteroscopic myomectomy is between 1-2 weeks.
How long does it take to recover from laparoscopic and robotic myomectomies?
Laparoscopic and robotic myomectomies generally allow return to normal activities within 2-4 weeks, with complete healing varying by individual.
What are the phases of scar healing after a myomectomy?
Scar healing follows four distinct biological phases: inflammatory response, proliferation, remodeling, and maturation, which can extend up to two years for full scar fading and softening.
How can I promote optimal healing after myomectomy?
Optimal healing can be promoted through proper wound care, sun protection, nutrition, and regular follow-ups.
What type of myomectomy is best for preserving fertility?
Myomectomy is a surgical procedure designed to remove uterine fibroids while preserving the uterus, making it an ideal option for women who wish to maintain their fertility.
How does robotic precision minimize tissue damage during myomectomy?
Robotic precision minimizes tissue damage by using precise robotic instruments, reducing the risk of complications and promoting better cosmetic outcomes.