Last Updated on November 20, 2025 by Ugurkan Demir
Acute Lymphocytic Leukemia (ALL) is a complex disease. It causes lymphoid cells to grow out of control in the bone marrow. Understanding ALL’s mechanisms is key to better treatments and better patient care. At LivHospital, we focus on top-notch care and patient needs to offer the best treatments. Understand pathophysiology of acute lymphocytic leukaemia, its mechanisms, and how it affects blood cell function.
ALL is a blood and bone marrow cancer. Knowing how it works is vital for better diagnosis and treatment. We’ll look at the seven main parts of ALL’s pathophysiology. This will give us insights into its mechanisms and what it means for patients.
Key Takeaways
- Understanding the pathophysiology of ALL is vital for effective treatment.
- ALL is marked by the uncontrolled growth of lymphoid cells.
- Advanced, evidence-based treatments lead to better patient outcomes.
- LivHospital offers top care standards.
- A patient-first approach is key for complete care.
Understanding Acute Lymphocytic Leukemia: Definition and Classification

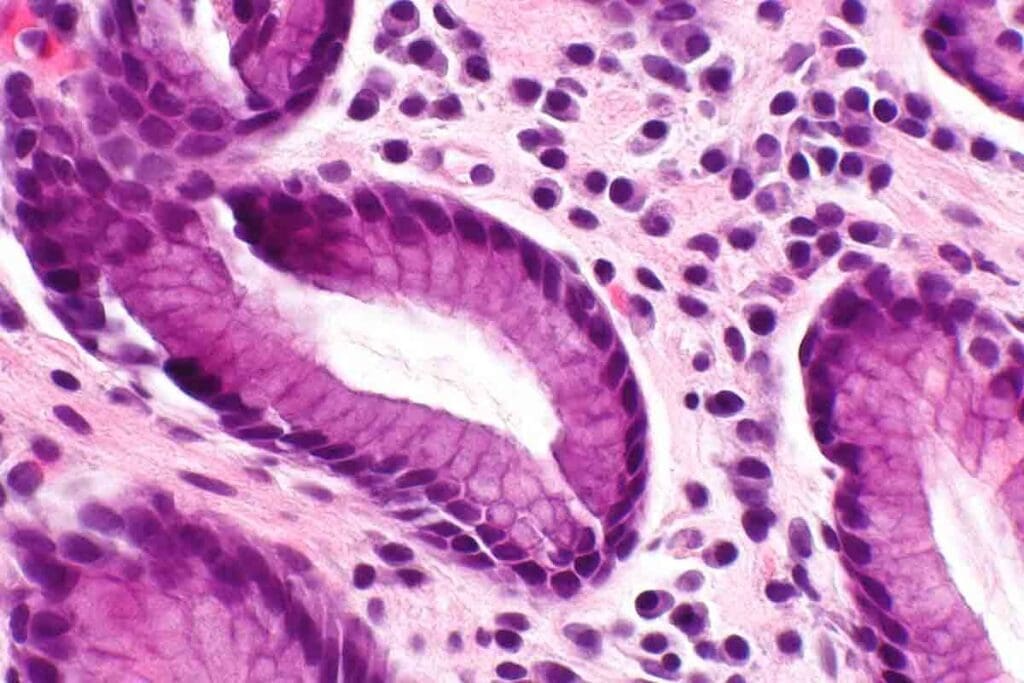
To understand Acute Lymphocytic Leukemia (ALL), we need to know its definition and classification. ALL is a type of leukemia where immature lymphoid cells grow too much. These cells can be B-cell or T-cell precursors. This shows how ALL affects lymphoid cells.
Distinguishing ALL from Other Leukemias
ALL is different from other leukemias because of the cell type and maturity. Doctors diagnose it by looking at bone marrow and blood. They check for lymphoblasts, which are signs of the disease.
Unlike Chronic Lymphocytic Leukemia (CLL), ALL has more immature cells. This is key to understanding ALL.
The type of ALL, B-cell or T-cell, also matters. B-cell ALL is more common in kids, while T-cell ALL has a worse outlook.
Epidemiology and Risk Factors
ALL is the top cancer in kids, making up 75% of childhood leukemias, says the American Cancer Society. It affects kids and adults over 65 in two peaks.
Genetic conditions like Down syndrome and radiation exposure increase the risk. Knowing these risks helps in early detection and prevention.
Studies on ALL’s causes and risks are ongoing. They help find ways to prevent and treat the disease.
The Pathophysiology of Acute Lymphocytic Leukemia: An Overview
Acute Lymphocytic Leukemia (ALL) starts with a complex interaction between lymphoid cells and their surroundings. This process is shaped by genetics and the environment. It leads to the uncontrolled growth of lymphoid cells.
ALL is mainly split into two types: B-cell precursor ALL and T-cell precursor ALL. B-cell precursor ALL makes up about 80-85% of cases in kids and many adults. T-cell precursor ALL is more aggressive and harder to treat.
B-Cell vs. T-Cell Precursor Involvement
Knowing the difference between B-cell and T-cell ALL is key. B-cell ALL often has genetic changes like ETV6-RUNX1 fusion, which is good for kids. T-cell ALL, with changes like NOTCH1 mutations, can affect treatment success.
The bone marrow environment is vital in ALL’s growth and spread. It helps leukemic cells live and grow. The interaction between leukemic cells and their environment can make them resistant to treatment.
Bone Marrow Microenvironment in ALL Development
The bone marrow is full of different cells that help leukemic cells grow. These cells protect leukemic cells from chemotherapy, leading to leftover disease.
| Component | Role in ALL Development | Impact on Treatment |
| Stromal Cells | Provide growth factors and cytokines supporting leukemic cell survival | Contribute to chemotherapy resistance |
| Endothelial Cells | Regulate angiogenesis and provide a niche for leukemic cells | Influence disease progression and metastasis |
| Immune Cells | Modulate immune responses against leukemic cells | Affect graft-versus-leukemia effect in allogeneic transplantation |
Understanding ALL’s causes, including B-cell and T-cell precursors and the bone marrow, is key. By focusing on how leukemic cells interact with their environment, we can improve treatment.
Key Aspect 1: Genetic Alterations Driving ALL Development
Genetic changes are key in Acute Lymphocytic Leukemia (ALL). They mess up cell functions, causing cells to grow out of control and form tumors. Knowing about these changes is vital for finding good treatments.
Chromosomal Translocations in ALL
Chromosomal translocations are a big deal in ALL. They create fusion genes that start the leukemia. For example, the ETV6-RUNX1 fusion is seen in about 25% of kids with ALL. This fusion messes up blood cell making, leading to too many lymphoblasts.
Other important translocations include BCR-ABL1 from t(9;22) and MLL gene rearrangements. These changes affect how well a person does and help doctors choose treatments.
Gene Mutations and Deletions
Gene mutations and deletions also play a big role in ALL. For instance, IKZF1 mutations are common. These mess up lymphocyte growth and help start leukemia.
Deletions in CDKN2A/B genes are also seen a lot. They mess with cell cycle control, helping turn lymphoid cells cancerous. Knowing about these changes helps find new treatments.
The mix of these genetic changes makes ALL very different. This means doctors need to do a detailed genetic check to diagnose and plan treatment right.
Key Aspect 2: Dysregulated Cell Division and Proliferation
Understanding how cell division and growth go wrong is key to grasping Acute Lymphocytic Leukemia (ALL). In ALL, cells grow out of control because of genetic changes. These changes mess up how cells normally work.
Cell Cycle Checkpoint Disruptions
Cell cycle checkpoints are vital for keeping our DNA safe. In ALL, these checkpoints fail, letting damaged cells keep growing. Checkpoint disruptions let cancer cells ignore normal rules, helping the disease spread.
A study on cancer biology points out, “The integrity of cell cycle checkpoints is critical for stopping genetic mistakes from spreading.” (
This is a key part of cancer growth, as it lets cells build up mutations that lead to tumors.
)
Role of c-MYC in Leukemic Cell Proliferation
c-MYC is a gene that helps cells grow and is often out of control in ALL. When c-MYC is not working right, cancer cells grow too fast. Research shows that too much c-MYC is bad news for many cancers, including ALL.
Looking closely at c-MYC’s role in ALL shows how it affects cell growth and death. c-MYC turns on genes that help cancer cells multiply, making the disease worse.
Hyperdiploidy and Hypodiploidy
Hyperdiploidy and hypodiploidy are big deals in ALL because they affect how well the disease does. Hyperdiploidy means more chromosomes and is usually better. Hypodiploidy means fewer chromosomes and is worse.
| Chromosomal Abnormality | Prognosis | Characteristics |
| Hyperdiploidy | Favorable | More than 50 chromosomes per cancer cell, often means better treatment response. |
| Hypodiploidy | Poor | Fewer than 44 chromosomes per cancer cell, means treatment won’t work as well and relapse risk is higher. |
Knowing about these chromosome issues is key for figuring out the best treatment for ALL patients. Telling hyperdiploidy from hypodiploidy helps doctors plan the right treatment for each person.
Key Aspect 3: Impaired Apoptosis Mechanisms
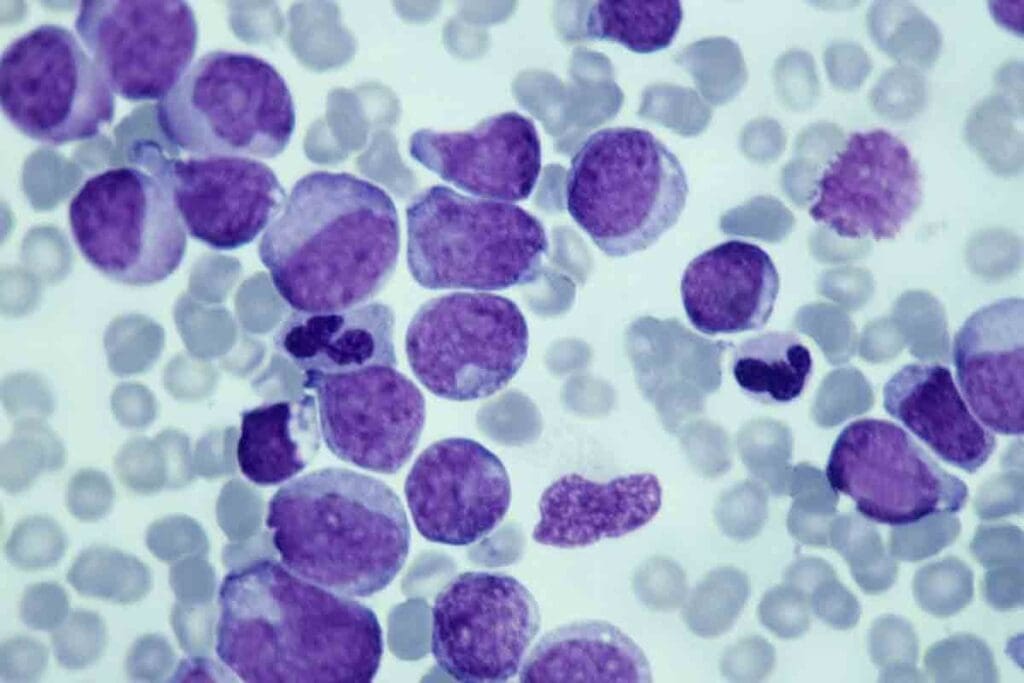
Acute Lymphocytic Leukemia (ALL) is marked by a failure in apoptosis. This failure lets leukemic cells avoid dying. Apoptosis is a process that removes damaged or unwanted cells from the body. In ALL, this process is broken, allowing leukemic cells to grow and multiply without control.
Anti-Apoptotic Protein Overexpression
One major reason for this failure is the overproduction of anti-apoptotic proteins. BCL-2, a known anti-apoptotic protein, is often found in high amounts in ALL cells. This high level stops caspases from working, which are key to apoptosis. This means leukemic cells can keep living and growing.
Studies show that high levels of BCL-2 make leukemia harder to treat and lead to worse outcomes.
“The BCL-2 family proteins play a critical role in apoptosis, and their imbalance is common in many blood cancers.”
Tumor Suppressor Gene Inactivation
Another important factor is the shutdown of tumor suppressor genes. Tumor suppressor genes help control cell growth and start apoptosis when DNA is damaged. In ALL, these genes are often turned off by mutations or deletions. This leads to cells growing and surviving without control.
The loss of TP53, a key tumor suppressor gene, is very significant. TP53 mutations are linked to a poor prognosis and resistance to treatment in ALL.
Survival Signaling in Leukemic Blasts
Survival signaling pathways also help leukemic blasts stay alive. These pathways involve complex interactions between different molecules. They can lead to the activation of anti-apoptotic proteins. Understanding these pathways is key to creating targeted treatments that kill leukemic cells.
In summary, the failure of apoptosis is a key part of ALL’s disease process. The overproduction of anti-apoptotic proteins, the shutdown of tumor suppressor genes, and the activation of survival signaling pathways all help leukemic cells survive and grow. More research is needed to find better treatments for ALL.
Key Aspect 4: Disrupted Signaling Pathways
Disrupted signaling pathways are key in Acute Lymphocytic Leukemia (ALL). These pathways help control cell growth, differentiation, and survival. In ALL, several important pathways are changed, helping the disease grow and spread.
PI3K/Akt Pathway Alterations
The PI3K/Akt pathway is often changed in ALL, helping cells live longer and grow more. Changes can happen through different ways, like mutations in parts of the pathway. This pathway helps leukemic cells by stopping them from dying and helping them use energy.
Studies show the PI3K/Akt pathway could be a good target for treatment in ALL. Researchers are looking at drugs that can kill leukemic cells by stopping this pathway.
JAK-STAT Signaling Abnormalities
The JAK-STAT pathway is also important in ALL, helping cells grow and survive. Changes in this pathway can make STAT proteins always active, helping leukemic cells grow and live longer. Some ALL patients have mutations in genes of the JAK-STAT pathway.
| Pathway Component | Alteration in ALL | Consequence |
| JAK2 | Mutations | Constitutive activation of STAT proteins |
| STAT5 | Phosphorylation | Enhanced cell survival and proliferation |
Notch Signaling in T-Cell ALL
Notch signaling is very important in T-cell ALL. It helps in T-cell development and differentiation. Activating mutations in NOTCH1 are common in T-ALL, causing abnormal Notch signaling.
The Notch pathway works with other pathways like PI3K/Akt and NF-κB to help leukemic cells grow. Targeting Notch signaling is seen as a promising treatment for T-ALL.
In summary, disrupted signaling pathways are a key feature of ALL. They help leukemic cells survive, grow, and resist treatment. Understanding these changes is vital for finding new treatments to help patients.
Key Aspect 5: Bone Marrow Failure Mechanisms
Leukemic cells in the bone marrow stop normal blood cell production. This leads to bone marrow failure in ALL patients. It affects the production of different blood cells, causing various symptoms.
Development of Anemia
Anemia is a common problem in ALL due to bone marrow failure. It happens because there are fewer red blood cells. Leukemic cells in the bone marrow reduce red blood cell production.
Chemotherapy and other treatments can make anemia worse. It’s important to manage anemia well to improve patient outcomes.
Neutropenia and Infection Risk
Neutropenia is when there are too few neutrophils. This is a problem in ALL due to bone marrow failure. It makes it hard for the body to fight off infections.
Infection risk management is key for ALL patients. We need to watch neutrophil counts and take steps to prevent infections. This includes using antibiotics and G-CSF when needed.
Thrombocytopenia and Bleeding Complications
Thrombocytopenia is when there are not enough platelets. It happens because the bone marrow can’t make enough platelets. This increases the risk of bleeding.
To manage thrombocytopenia, we use platelet transfusions. We also consider thrombopoietin receptor agonists to help make more platelets.
In summary, bone marrow failure in ALL causes many blood-related problems. Understanding these issues helps us find better ways to manage them. This improves patient outcomes.
Key Aspect 6: Central Nervous System Infiltration
Leukemic cells can invade the central nervous system (CNS) in Acute Lymphocytic Leukemia (ALL). This is a big problem, mainly in high-risk cases. It greatly affects how well treatment works.
Role of VEGF-A Expression
Vascular Endothelial Growth Factor-A (VEGF-A) is key in making new blood vessels. It’s linked to cancer growth, including ALL. VEGF-A makes blood vessels more open and helps new blood vessels grow. This can let leukemic cells get into the CNS.
Research shows that more VEGF-A means more chance of ALL cells getting into the brain. This happens because VEGF-A helps break down the blood-brain barrier. This barrier is what keeps bad stuff out of the brain.
CD56/NCAM Overexpression and CNS Disease
CD56, or Neural Cell Adhesion Molecule (NCAM), is found in some ALL cases. It’s linked to brain involvement. CD56/NCAM helps leukemic cells stick and move through the blood-brain barrier. This helps them get into the CNS.
CD56/NCAM on leukemic cells also helps them survive and grow in the brain. This is because it lets them fit better with the brain’s environment.
Blood-Brain Barrier Penetration Mechanisms
The blood-brain barrier (BBB) keeps most stuff out of the CNS. In ALL, leukemic cells find ways to get past it. They do this by breaking down tight junctions and making more adhesion molecules.
Knowing how they do this is key. It helps in making treatments that stop or fix CNS problems in ALL patients.
Key Aspect 7: Chemotherapy Resistance Development
Chemotherapy resistance in ALL comes from several factors. These include drug efflux, changes in drug metabolism, and protection from the microenvironment. Knowing these mechanisms is key to finding better treatments.
Drug Efflux Mechanisms
Drug efflux means chemotherapeutic agents are pushed out of leukemic cells. This makes the drugs less effective. The P-glycoprotein (P-gp) efflux pump is a major player in this process.
A study found that P-gp overexpression is linked to a poor prognosis in many leukemias, including ALL.
“The development of multidrug resistance is a major obstacle to successful chemotherapy in ALL patients.”
Altered Drug Metabolism
Changes in drug metabolism also play a part in resistance. Enzymes in drug metabolism can change how leukemic cells react to chemotherapy. For example, gene variations can affect drug effectiveness and toxicity.
Microenvironmental Protection of Leukemic Cells
The bone marrow microenvironment helps protect leukemic cells from chemotherapy. Cells like stromal and immune cells, along with signaling pathways, are involved. This interaction can activate survival pathways, making cells more resistant to drugs.
Understanding chemotherapy resistance in ALL is vital for better treatments. By tackling these challenges, we aim to improve outcomes for ALL patients.
Immunological Aspects and Minimal Residual Disease
Acute Lymphocytic Leukemia (ALL) is a disease where the immune system and cancer cells interact in complex ways. ALL causes lymphoblasts to grow and spread to organs like the bone marrow and spleen. The immune system tries to fight these cells but the cancer finds ways to avoid being detected and destroyed.
Immune Evasion Strategies
Leukemic cells in ALL use several tricks to avoid being found and killed by the immune system. One trick is to express PD-L1, which stops T cells from working properly. Immune checkpoint blockade is a new treatment that tries to stop this trick.
“The expression of PD-L1 on leukemic cells is a significant mechanism of immune evasion, making it a promising target for treatment.”
Another trick is to change the area around the cancer cells to make it harder for the immune system to attack. This is done by releasing chemicals that suppress the immune response and by attracting cells that calm down the immune system.
Immunophenotypic Classification
Immunophenotyping is key for diagnosing and classifying ALL. It uses flow cytometry to look at cell surface markers to identify lymphoblasts. There are mainly two types: B-cell precursor ALL (BCP-ALL) and T-cell ALL (T-ALL).
| Immunophenotype | Markers | Clinical Significance |
| B-cell precursor ALL | CD19, CD10, CD22 | Most common subtype in children |
| T-cell ALL | CD2, CD3, CD7 | Often associated with higher risk |
Detection and Significance of Minimal Residual Disease
Minimal residual disease (MRD) is when cancer cells are left after treatment. MRD is important because it shows how well the treatment worked and how likely a relapse is. Flow cytometry and PCR are used to find these cells even when there are very few.
MRD is important for deciding on treatment plans. It can also help find relapse early, so treatment can start sooner.
In summary, understanding ALL’s immune interactions, evasion strategies, and MRD is key to better treatments. By using this knowledge, we can make treatments more effective and tailored to each patient.
Conclusion: Translating Pathophysiological Insights into Clinical Practice
Understanding Acute Lymphocytic Leukemia (ALL) is key to better treatments. We’ve looked at seven important aspects of ALL’s pathophysiology. These insights help us understand how to treat the disease.
By using these insights in treatment, we can help patients more. ALL is complex, involving genetics, molecules, and environment. So, we need a detailed approach to treat it.
As we learn more about ALL, we can make treatments better. This means targeting specific parts of the disease. StatPearls says knowing how ALL works is vital for good treatments.
By using what we know about ALL in treatment, we can improve care. This makes treatment more tailored to each patient’s needs.
FAQ
What is Acute Lymphocytic Leukemia (ALL)?
Acute Lymphocytic Leukemia (ALL) is a blood and bone marrow cancer. It happens when immature lymphoid cells grow too much.
What are the different subtypes of Acute Lymphocytic Leukemia?
ALL has two main types: B-lymphoblastic leukemia/lymphoma and T-lymphoblastic leukemia/lymphoma. They differ based on the type of lymphoid cell involved.
What are the risk factors associated with developing Acute Lymphocytic Leukemia?
Risk factors for ALL include genetic predisposition and exposure to toxins. Previous radiation therapy and certain genetic syndromes also increase the risk.
How do genetic alterations contribute to the development of ALL?
Genetic changes, like chromosomal translocations and gene mutations, are key in ALL. They disrupt normal cell functions and help leukemic cells grow.
What is the role of the bone marrow microenvironment in ALL development?
The bone marrow microenvironment supports the growth of leukemic cells. It’s vital for ALL development and progression.
How does chemotherapy resistance develop in Acute Lymphocytic Leukemia?
Chemotherapy resistance in ALL arises from several factors. These include drug efflux, altered drug metabolism, and protection by the microenvironment.
What is minimal residual disease in the context of ALL?
Minimal residual disease (MRD) is when leukemic cells stay in the body after treatment. It’s a key factor in predicting ALL outcomes.
How is Acute Lymphocytic Leukemia diagnosed?
ALL diagnosis involves blood tests, bone marrow biopsy, and imaging studies. These help find leukemic cells and assess disease extent.
What is the significance of CNS infiltration in Acute Lymphocytic Leukemia?
CNS infiltration is a critical aspect of ALL. It can lead to central nervous system involvement, impacting treatment success.
How do disrupted signaling pathways contribute to the development of ALL?
Disrupted pathways, like PI3K/Akt, JAK-STAT, and Notch, are vital in ALL. They help leukemic cells survive and grow.
References
- Li, J. F., Dai, Y. T., Lilljebjörn, H., Shen, S. H., Cui, B. W., Bai, L., … & Qian, M. (2018). Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proceedings of the National Academy of Sciences, 115(50), E11711–E11720. https://pubmed.ncbi.nlm.nih.gov/30487239/





