
Sickle cell disease causes intense pain crises that can really disrupt life. It makes red blood cells misshapen, blocking tiny blood vessels. This leads to less oxygen, tissue damage, and pain.
Lana Quarles knows how tough it is when her son has Sickle Cell Disease (SCD). The pain can be so bad that families might look for better care elsewhere. We get how hard this condition is and how important caring, advanced care is.
It’s important to understand sickle cell disease to see its impact. Sickle cell disease (SCD) is a genetic disorder. It affects how red blood cells carry oxygen.
Sickle cell disease comes from a gene mutation. This mutation changes the hemoglobin in red blood cells. If you get two copies of this mutated gene, you might get sickle cell disease.
Inheriting the mutated gene can lead to different forms of the disease. This depends on whether you have two copies or one copy of the mutated gene.
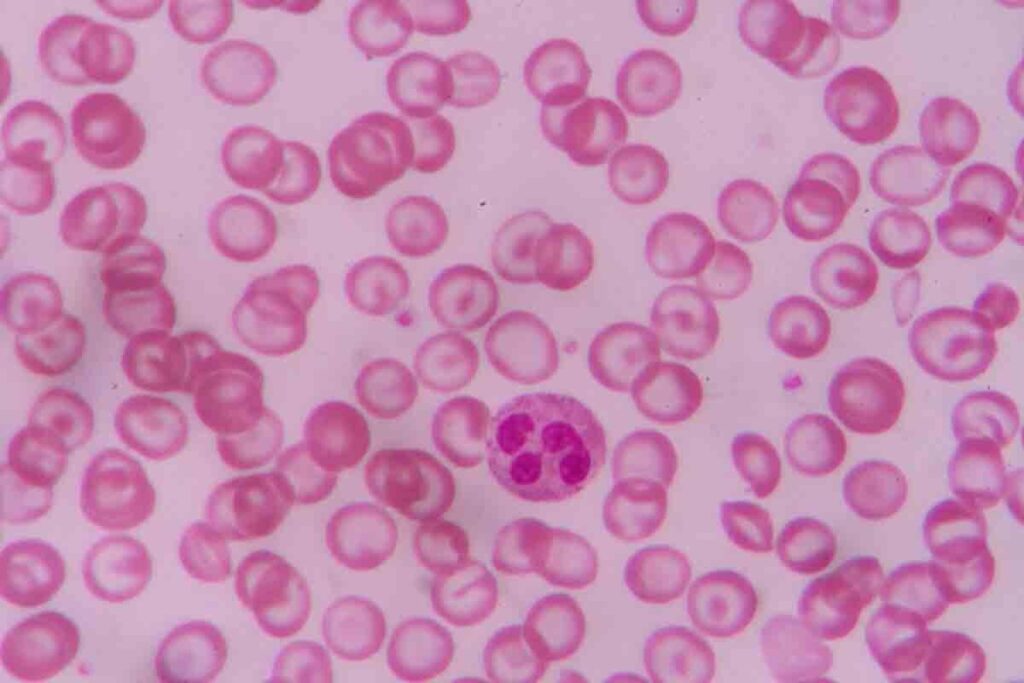
Abnormal hemoglobin makes red blood cells sickle shape when oxygen is low. These sickled cells break down faster and can block blood vessels. This causes many health problems.
The sickling of red blood cells shortens their life and makes them less efficient at carrying oxygen. This is why sickle cell disease is so challenging.
Sickle cell disease hits some groups harder than others. It’s most common in people of African descent. But it also affects those from the Mediterranean, South Asia, and Hispanic/Latin American backgrounds.
| Population | Prevalence of Sickle Cell Disease |
| African ancestry | 1 in 500 births |
| Hispanic/Latin American | 1 in 1,000 to 1 in 4,000 births |
| Mediterranean and South Asian | Variable, but significant prevalence |
Knowing who gets sickle cell disease helps with health efforts. It also helps in giving the right care to those affected.

To understand why sickle cell disease causes pain, we need to look at the underlying causes. This includes the role of sickled cells and how they block blood vessels. Sickle cell disease is a genetic disorder that affects how red blood cells are made.
Sickled red blood cells are stiff and can get stuck in small blood vessels. This causes blood flow to stop, leading to tissue damage and pain. Cold weather can make blood vessels constrict, which can block blood flow.
The process of blood vessels getting blocked is complex. It involves sickled red blood cells, the lining of blood vessels, white blood cells, and platelets. This interaction causes inflammation and makes the blockage worse.
When blood flow is blocked, tissues don’t get enough oxygen. This lack of oxygen causes cell damage and the release of pain-causing substances. This creates a cycle of pain and tissue damage.
The damage from lack of oxygen can last a long time. It can lead to chronic pain in some people. Understanding this is key to managing sickle cell disease pain.
The inflammatory response is also important in sickle cell disease pain. When sickled red blood cells interact with blood vessel walls, it starts an inflammatory process. This process releases substances that increase pain perception.
| Pathophysiological Mechanism | Effect on Sickle Cell Disease Pain |
| Sickled Cells and Vascular Occlusion | Leads to tissue ischemia and pain due to obstruction of blood flow. |
| Tissue Hypoxia and Damage | Results in cellular damage and release of pain-producing substances. |
| Inflammatory Response | Enhances pain perception through the release of cytokines and inflammatory mediators. |
Understanding these mechanisms helps healthcare providers find better ways to manage sickle cell disease pain.
It’s key to understand vaso-occlusive crisis to manage sickle cell disease well. A vaso-occlusive crisis, or sickle cell crisis, happens when sickled red blood cells block small blood vessels. This leads to tissue ischemia and pain.
A vaso-occlusive crisis is when sickled red blood cells block blood vessels. This causes poor blood flow to organs and tissues. It results in ischemia and infarction, causing severe pain and possibly harming organs.
The process starts with abnormal hemoglobin S polymerizing under low oxygen. This makes red blood cells sickle-shaped. These sickled cells are less flexible and more likely to get stuck in small blood vessels.
Several factors can trigger a vaso-occlusive crisis. These include:
Knowing these triggers can help prevent or lessen vaso-occlusive crises.
The progression of a vaso-occlusive crisis varies among people. It often starts with pain, which can be mild or severe. If not treated right, it can lead to serious issues like acute chest syndrome and organ damage.
People with sickle cell disease should know their triggers. They should stay hydrated and avoid extreme temperatures to lessen crisis frequency and severity.
People with sickle cell disease face different kinds of pain. Knowing these types is key to managing their pain well.
Acute pain episodes, or vaso-occlusive crises, are common in sickle cell disease. They happen when sickled red blood cells block blood vessels. This causes tissue ischemia and pain.
These episodes can be very intense and last a long time. Often, they need quick medical help.
Many with sickle cell disease also deal with chronic pain. This pain comes from ongoing inflammation, organ damage, or other disease complications.
Managing chronic pain needs a full plan. This includes medicines and other non-medical ways to help.
Neuropathic pain is another type in sickle cell disease. It’s caused by nerve damage or problems. This pain feels like burning, shooting, or stabbing.
Studies show that combining therapy and mindfulness can help manage this pain.
| Type of Pain | Characteristics | Management Strategies |
| Acute Pain Episodes | Sudden onset, variable intensity, often severe | Immediate medical attention, pain relief medications, hydration |
| Chronic Pain Syndromes | Ongoing, persistent pain, may be accompanied by organ damage | Comprehensive pain management plans, including pharmacological and non-pharmacological approaches |
| Neuropathic Pain | Burning, shooting, or stabbing sensations, often due to nerve damage | Specific neuropathic pain medications, alternative therapies like acupuncture |
Understanding the various pains in sickle cell disease helps doctors create better treatment plans. These plans are made to meet each patient’s unique needs.
Understanding pain in sickle cell disease is key to better management. Sickle cell disease causes pain due to blood vessel blockages. This pain is not just from tissue damage but also from changes in how the nervous system processes pain.
Peripheral sensitization makes pain sensors more sensitive due to inflammation. In SCD, blood vessel blockages cause inflammation. This makes pain sensors more active, leading to increased pain perception.
Inflammatory mediators like bradykinin and prostaglandins are key in this process. They make pain sensors more easily triggered, leading to more pain during a crisis.
Central sensitization makes the brain and spinal cord more sensitive to pain. This happens when the body keeps sending pain signals, like in SCD. It can lead to chronic pain and increased sensitivity to pain.
SCD pain management is complex because of central sensitization. It shows that treating pain requires addressing both the body’s pain signals and the brain’s response.
Pain memory and anticipation play big roles in SCD pain. Past pain experiences can affect how current pain is felt. Anticipating pain can also make it worse, creating a cycle of fear and increased sensitivity.
Understanding these factors is vital for effective pain management. It helps healthcare providers offer more complete care to those with SCD.
Biochemical mediators play a big role in sickle cell disease pain. They work together in complex ways to cause the painful crises seen in the condition.
Substance P is a neuropeptide that helps send pain signals. It is released by certain nerve fibers and works on the neurokinin-1 receptor. This helps in transmitting pain. In sickle cell disease, substance P makes pain worse.
“Substance P is involved in the transmission of pain signals and is a key mediator in the pain associated with sickle cell disease.”
Studies have found that substance P levels go up during pain crises. This makes the pain felt by patients even worse.
Cytokines are small proteins that help cells talk to each other. In sickle cell disease, cytokines like TNF-alpha and IL-1β are higher. They make the inflammation worse, which increases pain.
| Cytokine | Role in Sickle Cell Disease |
| TNF-alpha | Promotes inflammation and pain |
| IL-1β | Enhances inflammatory response |
| IL-6 | Involved in acute phase response |
Inflammatory markers, like C-reactive protein (CRP), also go up. This shows there’s ongoing inflammation that adds to the pain.
Endothelial dysfunction is key in sickle cell disease. The endothelium helps control blood vessel tone. When it doesn’t work right, it leads to more inflammation and clotting. This makes the disease harder to manage.
The mix of biochemical mediators and endothelial dysfunction makes pain in sickle cell disease worse. Knowing how these work together is important for finding new treatments.
Understanding the role of biochemical mediators in sickle cell disease pain helps us manage it better. This improves the lives of those with the condition.
Sickle cell trait and sickle cell disease are not the same. Sickle cell disease is a serious condition where red blood cells sickle. Sickle cell trait means you carry one normal and one abnormal hemoglobin gene.
The main difference is in the genes. People with sickle cell trait have one normal and one abnormal gene. They are carriers but usually don’t get sick. Those with sickle cell disease have two abnormal genes and get the disease.
Most people with SCD are Black. This shows why genetic screening is key in this group.
Those with sickle cell trait usually don’t have bad symptoms. But, they might feel some effects at high altitudes or when very active. People with sickle cell disease often have pain, anemia, and other problems because of sickled red blood cells.
No, sickle cell trait can’t become sickle cell disease. It’s a carrier state. The chance of having a sickle cell disease child depends on both parents’ genes. If both parents are carriers, there’s a 25% chance with each child.
Knowing the genetic risks helps with family planning and health care choices.
Sickle cell disease causes more than just pain. People with this disease face serious health problems. These issues can affect their life quality and health.
Acute chest syndrome (ACS) is a big problem for those with sickle cell disease. It shows up as a new spot on a chest X-ray, often with fever, breathing issues, or chest pain. ACS can happen for many reasons, like infections or blood clots in the lungs.
Managing ACS means acting fast. Patients need oxygen, fluids, and sometimes blood transfusions to lower the bad hemoglobin S.
Stroke is a big worry for kids with sickle cell disease. It can happen because of blood clots or aneurysms. Other brain problems, like silent strokes, can also cause issues with thinking and growing.
Sickle cell disease can harm many organs. This is because of blood clots and too much breakdown of red blood cells. The spleen, kidneys, liver, and heart are often affected. For example, the spleen can get damaged and stop working, and the kidneys can suffer from too much breakdown over time.
Preventive measures and early treatment are key. They help manage these problems and improve life for those with sickle cell disease.
Managing sickle cell pain and crisis needs a mix of strategies. This includes preventive steps, medicines, and lifestyle changes. It’s key to improve life quality for those with sickle cell disease.
Preventing sickle cell crises is vital. Here are ways to do it:
Staying hydrated is very important. Dehydration can lead to a crisis. Drinking lots of water and avoiding diuretics helps keep hydration levels right.
Medicines are key in managing sickle cell pain. These include:
Hydroxyurea can cut down on painful crises. It may also lessen the need for blood transfusions.
There are also non-medical ways to manage pain:
A comprehensive management plan with these methods can greatly improve life quality for those with sickle cell disease.
Knowing when to seek emergency care is critical. Severe pain not helped by meds, acute chest syndrome symptoms, or infection signs need immediate help.
“Understanding when to seek emergency care is key to prevent serious complications from sickle cell disease.”
Living with sickle cell disease needs a detailed plan to handle its challenges. We’ve looked at the basics of SCD, its causes, and the problems it brings. This includes painful crises and ongoing pain issues.
Effective management of SCD requires a team of experts. It also needs preventive steps and treatments. At Liv Hospital, we aim to give top-notch care to patients from around the world. We focus on creating a supportive space to improve life quality for those with SCD.
It’s key to know the difference between sickle cell disease and trait for proper care. By taking a complete approach to SCD management, we aim to lessen the impact of crises. This helps improve the health and happiness of those affected.
Sickle cell trait means you have one normal and one abnormal hemoglobin gene. Sickle cell disease means you have two abnormal genes. Sickle cell trait usually doesn’t cause health problems. But sickle cell disease can lead to serious issues like pain crises.
No, sickle cell trait can’t turn into sickle cell disease. It’s a harmless condition that doesn’t get worse. But people with sickle cell trait can pass the abnormal gene to their kids.
Symptoms of sickle cell disease vary. They often include pain, anemia, infections, and other issues. Pain crises are common and can be caused by dehydration, cold, or stress.
Doctors use a blood test to find abnormal hemoglobin to diagnose sickle cell disease. They can also test for it before a baby is born.
Sickle cell disease can cause serious problems. These include acute chest syndrome, stroke, neurological issues, and organ damage. These can be very dangerous and need quick medical help.
Managing sickle cell pain involves several steps. This includes using medicines, staying hydrated, resting, and avoiding things that can trigger pain.
Usually, people with sickle cell trait don’t have symptoms. But sometimes, they might have issues like hematuria or splenic infarction. This can happen under stress or at high altitudes.
A vaso-occlusive crisis happens when sickled red blood cells block blood vessels. This causes pain and tissue damage. It can be triggered by dehydration or cold.
Sickle cell disease makes red blood cells misshapen and rigid. This leads to their early destruction and blocks blood vessels. It causes anemia, pain, and other problems.
Sickle cell disease can cause neurological issues. These include stroke, seizures, and cognitive problems. These can happen due to vaso-occlusive crises or other disease-related reasons.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us