Choosing the right post-operative diet is key to lasting health after bariatric surgery. At Liv Hospital, we help our patients with a detailed diet plan. This plan moves through stages, helping them smoothly transition to a healthier way of life.Master your bariatric post op diet with these 7 essential tips. This guide ensures your long-term success and health after surgery.
The journey starts with clear liquids. It then moves to full liquids, pureed foods, and soft foods before reaching solid foods. This step-by-step approach helps the body adjust and lowers the risk of problems.
Key Takeaways
- Follow a progressive dietary plan after bariatric surgery.
- Start with clear liquids and gradually move to more solid foods.
- Prioritize protein intake for optimal recovery.
- Stay hydrated throughout the recovery process.
- Consult with healthcare professionals for personalized guidance.
The Bariatric Surgery Journey and Nutritional Changes
Bariatric surgery changes how your body digests food. It’s not just about losing weight. It’s a big change that affects how your body handles food.
How Your Digestive System Changes After Surgery
After surgery, your digestive system changes. This can include a smaller stomach or different intestines. These changes affect how you absorb nutrients, so you need to eat differently.
The surgery limits how much food you can eat at once. It also changes how your body absorbs nutrients. So, it’s important to eat foods that are full of nutrients.
Why Proper Nutrition is Critical for Recovery and Results
Good nutrition is key for recovery and success after surgery. It helps your body heal and keeps your muscles strong. It also makes sure you get all the vitamins and minerals you need.
Eating the right foods after surgery is important for keeping weight off. It also helps avoid problems like nutritional deficiencies.
| Nutritional Aspect | Pre-Surgery | Post-Surgery |
| Eating Habits | Normal eating habits | Frequent, small meals |
| Nutrient Absorption | Normal absorption | Potential for reduced absorption of certain nutrients |
| Dietary Focus | Varied diet | High protein, nutrient-dense foods |
It’s important to understand and adapt to these changes. By choosing the right foods and eating habits, you can help your body recover well. This way, you can reach your weight loss goals in the long run.
Understanding the Bariatric Post Op Diet Progression

After bariatric surgery, patients must follow a carefully structured diet progression. This ensures proper healing and optimal weight loss results. The diet progression is designed to minimize complications and support the body’s adjustment to its new digestive system.
“The post-operative diet is a critical component of the bariatric surgery journey,” says a leading bariatric nutrition expert. “It requires patience, dedication, and a thorough understanding of the dietary stages.”
Stage 1: Clear Liquids (First Few Days)
The initial stage post-surgery involves consuming clear liquids. This stage is critical for allowing the stomach to heal without being strained by solid foods. Clear liquids include broths, electrolyte-rich beverages, and water. Patients are advised to sip slowly and avoid using straws to minimize swallowing air.
Stage 2: Full Liquids (1-2 Weeks Post-Surgery)
Once the patient has tolerated clear liquids, they can progress to full liquids. Full liquids provide more calories and nutrients. They may include milk, yogurt, and protein shakes. It’s essential to choose liquids that are nutrient-dense to support healing and satisfaction.
Stage 3: Pureed Foods (3-4 Weeks Post-Surgery)
Pureed foods mark the transition towards more substantial nutrition. Patients must blend their food to a smooth consistency. This stage introduces more variety in terms of flavors and nutrients, including pureed meats, vegetables, and fruits. Patients should continue to eat slowly and stop when they feel full.
Stage 4: Soft Foods (5-6 Weeks Post-Surgery)
The final stage before returning to a more normal diet involves eating soft foods. Examples include cooked pasta, scrambled eggs, and tender meats. Patients should continue to prioritize protein-rich foods and be mindful of their body’s signals of fullness and hunger.
By understanding and adhering to these dietary stages, patients can significantly enhance their recovery process. This sets them up for long-term success after bariatric surgery.
Essential Tip #1: Master Your Protein Requirements
Getting enough protein is key for recovery and success after bariatric surgery. Protein helps keep muscles strong, aids in healing, and keeps your diet balanced.
Why You Need 60-80g of Protein Daily
It’s important for bariatric patients to eat 60-80 grams of protein every day. This helps keep muscles from shrinking and supports healing. It also helps control hunger and fullness.
- Maintaining muscle mass
- Supporting the healing of tissues
- Regulating hunger and satiety hormones
By eating this amount, patients can support their body’s needs and stay healthy.
Best Protein Sources for Bariatric Patients
Finding the right protein sources is important. Some top choices for bariatric patients are:
- Lean meats (chicken, turkey, lean beef)
- Fish and seafood
- Eggs
- Low-fat dairy products
- Protein supplements (if recommended by a healthcare provider)
Tracking and Meeting Your Protein Goals
To make sure you get enough protein, try these tips:
- Keep a food diary to track your daily protein intake.
- Use a protein tracking app to monitor your progress.
- Consult with a nutritionist to create a personalized meal plan.
These strategies help bariatric patients track and meet their protein goals. This supports their health and recovery.
Essential Tip #2: Navigate Caloric Progression Strategically
Managing caloric progression is key to a successful bariatric journey. After surgery, your body’s nutritional needs change a lot. It’s important to control your caloric intake for recovery, weight loss, and health.
First Month: Managing 300-600 Calories Daily
In the first month, patients eat very few calories, from 300 to 600 per day. This helps the stomach heal and promotes weight loss. Focus on foods rich in nutrients to meet your daily needs, even with low calories.
Nutritional Considerations for the First Month:
- Prioritize protein-rich foods and supplements.
- Choose low-calorie, nutrient-dense liquids and pureed foods.
- Stay hydrated by drinking fluids between meals.
Months 2-12: Transitioning to 900-1,000 Calories
As you move into the second month and beyond, your caloric needs increase. You’ll aim for 900 to 1,000 calories per day. This allows for a more varied diet with soft foods and eventually solids.
Key Considerations for Months 2-12:
- Continue to prioritize protein intake.
- Gradually introduce a variety of soft, nutrient-dense foods.
- Monitor your body’s response to the increased caloric intake and adjust as needed.
Year 1 and Beyond: Stabilizing at Appropriate Caloric Intake
By the end of the first year, most patients find a stable caloric intake. This supports weight loss and nutritional needs. The exact intake varies based on age, sex, weight, activity level, and health.
| Stage | Caloric Intake | Nutritional Focus |
| First Month | 300-600 calories | Nutrient-dense, high-protein liquids and pureed foods |
| Months 2-12 | 900-1,000 calories | Varied diet with soft, nutrient-dense foods; high protein |
| Year 1 and Beyond | Stabilized caloric intake | Balanced diet supporting weight loss maintenance and overall health |
Strategically managing caloric progression is key to a successful bariatric journey. By adapting to changing caloric needs, patients can improve their weight loss and health.
Essential Tip #3: Implement Proper Hydration Techniques
Hydration is key for bariatric surgery patients to recover well and succeed. It helps with health, nutrient absorption, and prevents problems.
Meeting Daily Fluid Requirements Without Stretching Your Pouch
Bariatric patients need to drink at least 48 fluid ounces (1.5 liters) a day. To do this without filling up the stomach, drink fluids all day long.
Tips for Proper Hydration:
- Drink slowly and in small amounts.
- Avoid drinking during meals.
- Choose water or low-calorie drinks.
The 30-Minute Rule: Separating Fluids from Meals
To keep the stomach pouch right, wait 30 minutes after eating to drink. This helps keep the pouch’s size and aids digestion.
Recognizing and Preventing Dehydration
Dehydration is a big risk for bariatric patients. Signs include dizziness, dry mouth, and dark urine. To avoid dehydration, watch your fluid intake closely and adjust as needed.
Daily Fluid Intake Guidelines:
| Time of Day | Fluid Intake |
| Morning | 16 oz (0.5 liters) |
| Afternoon | 16 oz (0.5 liters) |
| Evening | 16 oz (0.5 liters) |
By following these hydration tips, bariatric patients can keep their health up and make their surgery a success.
Essential Tip #4: Master Portion Control for Lifelong Success
Mastering portion control is key for lasting success after bariatric surgery. It’s not just about eating the right foods. It’s also about knowing how much to eat. By controlling portions, patients can keep their weight off and boost their health.
Using Appropriate Dishware for Your New Stomach Size
Using the right dishware is a smart way to control portions. Smaller plates and bowls help you see and stick to the right amounts. This simple change can greatly improve your eating habits.
Smaller dishware tricks your mind into feeling full with less food. It helps you adjust to new eating habits after surgery. It’s a practical step towards a healthier food relationship.
The Importance of Slow, Mindful Eating
Eating slowly and mindfully is key for portion control. Mindful eating means focusing on the eating experience, both physically and emotionally. It helps you better understand when you’re hungry or full.
Slow eating prevents overeating by letting your body signal when it’s full. It’s good to chew food well and pause between bites. This makes eating more intentional.
Recognizing True Hunger and Fullness Cues
It’s important to know and listen to your hunger and fullness cues. After bariatric surgery, your stomach is much smaller. So, it’s critical to eat when hungry and stop when you’re comfortably full.
- Listen to your body’s hunger and fullness signals.
- Don’t eat because of emotions.
- Stop eating when you’re satisfied, not when you’re stuffed.
By mastering these skills, bariatric patients can better control their food intake. This supports their long-term weight loss goals and overall health.
Essential Tip #5: Commit to Lifelong Nutritional Supplementation
Nutritional supplements are a lifelong need for those who have had weight loss surgery. After surgery, the body can’t absorb nutrients as well. This makes supplements key for staying healthy.
Essential Vitamins After Weight Loss Surgery
Patients after bariatric surgery face a high risk of vitamin deficiencies. This is because their stomach is smaller and digestion changes. Vitamin B12 is very important because it’s harder to absorb after surgery. Other important vitamins include Vitamin D for bones and Folate to prevent anemia.
Vitamin A and Vitamin E are also vital. They help keep skin healthy and eyes working well, and boost the immune system. It’s important to keep an eye on vitamin levels to avoid shortages.
Mineral Supplementation to Prevent Deficiencies
Minerals like Iron, Calcium, and Zinc are essential for many body functions. After surgery, the body may not absorb these minerals as well. This can lead to a lack of them.
Iron deficiency is common, but it’s more common in women who menstruate. Calcium is important for strong bones, and Zinc helps with healing and fighting off infections. Regular blood tests can catch mineral shortages early.
Creating a Sustainable Supplement Routine
Having a consistent supplement routine is vital for long-term health after surgery. Patients should talk to their doctor to find the right supplements. Multivitamins made for bariatric patients can help fill nutritional gaps.
It’s important to make a routine that’s easy to stick to. This could be setting reminders or taking supplements with meals. Regular check-ups with your doctor will help adjust your supplements as needed.
Essential Tip #6: Develop a Sustainable Meal Planning System
Creating a meal plan that’s both healthy and sustainable is key to losing weight after bariatric surgery. A good meal plan meets your nutritional needs and helps keep your weight healthy over time.
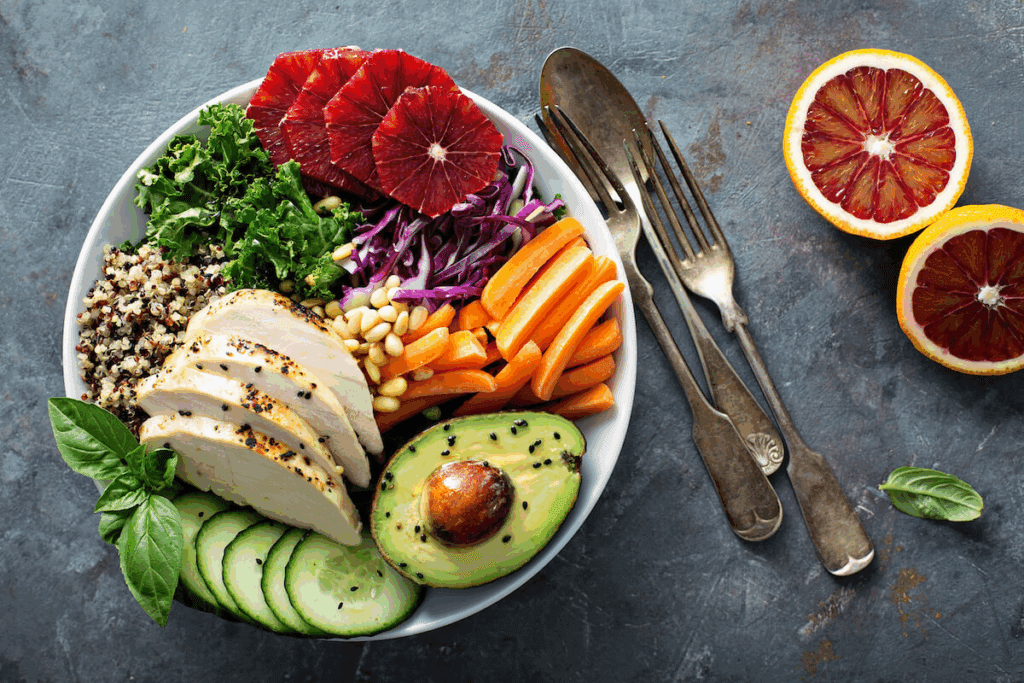
Creating Balanced Meals with Adequate Nutrition
Balanced meals are vital to avoid nutrient deficiencies. Include a variety of food groups in your diet. Lean proteins like chicken, fish, and tofu are essential for your body’s recovery and upkeep.
Adding vegetables and whole grains to your meals gives you vital vitamins and minerals. They also help you feel full. Try to have a colorful plate to get a wide range of nutrients.
Batch Cooking and Meal Prep Strategies
Batch cooking and meal prep help keep your diet consistent. Preparing meals ahead of time means you always have healthy options, even when you’re busy.
- Plan your meals for the week ahead of time.
- Cook in bulk to save time and reduce food waste.
- Portion out your meals into individual containers for easy grab-and-go options.
Sample Meal Plans for Different Post-Op Stages
Meal plans should change as you progress in your recovery. Here are some tips for meal plans at different stages:
| Post-Op Stage | Meal Plan Focus | Sample Foods |
| Clear Liquids | Hydration and electrolytes | Broth, electrolyte-rich beverages |
| Pureed Foods | Protein-rich, smooth textures | Pureed chicken, yogurt |
| Soft Foods | Gradual introduction of solid foods | Soft fruits, cooked vegetables |
By creating a sustainable meal planning system, you ensure your body gets the nutrients it needs for recovery and long-term health.
Essential Tip #7: Build a Supportive Environment
Creating a supportive environment is key to your success after surgery. A good support system helps you deal with surgery challenges. It keeps you on track with your diet and health goals.
Communicating Your Dietary Needs with Family and Friends
Talking to your loved ones about your diet is important. Teach them about your new eating habits. Explain what foods you can have and the need for small portions.
Tips for Communicating Dietary Needs:
- Share your meal plans and dietary restrictions with family and friends.
- Ask for their support in preparing suitable meals.
- Explain the consequences of not following your dietary plan.
Finding Support Groups and Resources
Joining a support group can be very helpful. These groups let you share experiences and advice with others. You’ll find people who understand your journey.
Benefits of Support Groups:
- Emotional support and understanding from peers.
- Access to valuable resources and information.
- Motivation and accountability.
Many surgery centers and healthcare providers offer support groups. Online forums and social media groups are also great for connecting with others who have had surgery.
Working with Nutrition Professionals Long-Term
Success after surgery needs ongoing nutrition advice. A dietitian or nutritionist can guide you through your new diet. They help with the challenges of your new eating habits.
Benefits of Long-Term Nutritional Support:
- Personalized dietary planning.
- Ongoing monitoring of nutritional deficiencies.
- Guidance on adapting your diet as your body changes.
With a supportive environment, including understanding family, support groups, and nutrition experts, you can achieve long-term success after surgery.
Long-Term Diet After Gastric Bypass Surgery
Gastric bypass surgery starts a new diet chapter. It needs careful planning and commitment. As patients recover, their diet needs change. They need a long-term plan for nutritional balance and sustainability.
Nutritional Considerations 1-2 Years Post-Surgery
One to two years after surgery, patients usually eat 900-1,000 calories a day. They focus on lean proteins and vegetables. This helps meet nutritional needs without overloading the stomach.
| Nutrient | Recommended Daily Intake | Food Sources |
| Protein | 60-80g | Lean meats, fish, eggs, dairy |
| Vegetables | 5 servings | Leafy greens, broccoli, bell peppers |
| Fruits | 3-4 servings | Berries, citrus fruits, apples |
Managing Dumping Syndrome Through Diet
Dumping syndrome can happen after gastric bypass surgery. It causes nausea, vomiting, diarrhea, and stomach cramps. To manage it, eat smaller meals often and avoid sugary foods.
- Eat smaller, more frequent meals
- Avoid high-sugar foods and drinks
- Choose complex carbohydrates over simple ones
Preventing Weight Regain Through Proper Nutrition
To avoid weight gain after surgery, focus on proper nutrition and portion control. Eat a balanced diet, watch your calories, and eat mindfully. This helps recognize hunger and fullness.
By sticking to these tips, patients can keep their weight off long-term.
2-3 Years Post Gastric Sleeve Diet Maintenance
Two to three years after gastric sleeve surgery, patients usually find a stable point in their diet. They have adjusted to new eating habits and aim to keep their weight loss. The focus now is on long-term weight management and health.
Stabilizing at 63-67g Protein and 1,000 Calories
By this time, patients stabilize their intake at 63-67 grams of protein and 1,000 calories. This amount supports their energy and keeps them at a healthy weight. Protein is key for muscle and health.
| Nutrient | Recommended Daily Intake |
| Protein | 63-67 grams |
| Calories | 1,000 |
Addressing Common Nutritional Challenges
Despite progress, patients may face nutritional challenges. Issues include vitamin deficiencies, not enough protein, and dehydration. Regular monitoring and adjustments can help solve these problems.
- Vitamin B12 deficiency
- Iron deficiency
- Dehydration
Adapting Your Diet as Your Body Changes
As the body changes, dietary needs may also change. It’s important to be flexible and adjust as needed. Working with a healthcare provider or nutritionist can help tailor the diet.
Maintaining a balanced diet after gastric sleeve surgery is a long-term effort. Understanding nutritional needs and challenges helps patients navigate their journey.
Overcoming Common Nutritional Challenges After Bariatric Surgery
After bariatric surgery, managing nutrition is key for recovery and weight control. Patients face many nutritional challenges that can affect their health and weight loss success.
Addressing Food Intolerances and Sensitivities
Food intolerances and sensitivities are common after bariatric surgery. These can happen due to changes in digestion, smaller stomach, and how nutrients are absorbed. Common symptoms include nausea, vomiting, diarrhea, and abdominal pain. To tackle these issues, patients should:
- Keep a food diary to track symptoms and identify trigger foods
- Eat small, frequent meals to reduce digestive stress
- Avoid foods high in sugar, fat, and spice
- Choose foods that are easy to digest, such as lean proteins and cooked vegetables
As “The Journal of the Academy of Nutrition and Dietetics” notes, “Identifying and avoiding trigger foods is key for managing symptoms and ensuring nutritional adequacy.”
Breaking Through Weight Loss Plateaus
Weight loss plateaus are a common challenge after bariatric surgery. These happen when the body gets used to the new diet, and weight loss slows or stops. To get past a plateau, try these strategies:
- Reassess your caloric intake and adjust as needed
- Increase physical activity to boost metabolism
- Review your protein intake to ensure it meets post-surgery needs
- Consult with a healthcare provider or a registered dietitian for personalized advice
A well-balanced diet combined with regular physical activity can help restart weight loss.
When to Consult Your Bariatric Team About Diet
Knowing when to seek help from your bariatric team about diet is important. Consult your team if you experience:
- Persistent or severe nutritional deficiencies
- Unmanageable food intolerances or sensitivities
- A weight loss plateau that doesn’t respond to dietary changes
- Any signs of dehydration or other complications
“Regular follow-up with a bariatric team is vital for addressing nutritional challenges and ensuring long-term success after bariatric surgery.”
By being proactive and informed, patients can overcome common nutritional challenges and achieve their weight loss goals.
Conclusion: Embracing Your Lifelong Nutritional Journey
Starting a bariatric post op diet is a big step towards lasting weight loss and better health. You’ve learned that success comes from a lifelong journey of healthy eating and lifestyle changes.
By following the 7 essential tips in this article, you can handle the new diet challenges. Learning about protein, calorie intake, and staying hydrated are key to success.
Success over time comes from making lasting changes in your diet and lifestyle. By sticking to a healthy journey, you can fully benefit from your surgery. This leads to a healthy weight and better overall health.
Remember, your bariatric post op diet is a long-term promise to your health. By focusing on your nutritional needs and making smart choices, you can live a healthier, happier life.
FAQ
What is the typical calorie intake for bariatric patients 1 year after surgery?
Bariatric patients usually need 900-1,200 calories a day. This amount can change based on the surgery type and individual needs.
How much protein should I consume after bariatric surgery?
It’s recommended to eat 60-80 grams of protein daily. This helps with healing, muscle, and overall health.
What are the stages of the bariatric post-op diet?
The diet stages are clear liquids, full liquids, pureed foods, and soft foods. These stages progress over weeks after surgery.
How do I manage dumping syndrome after gastric bypass surgery?
To manage dumping syndrome, avoid high-sugar and high-fat foods. Eat smaller meals and choose nutrient-rich foods to prevent symptoms.
What are the best protein sources for bariatric patients?
Good protein sources include lean meats, fish, eggs, dairy, and bariatric-specific protein supplements.
How can I prevent dehydration after bariatric surgery?
To prevent dehydration, drink fluids all day, not with meals. Make sure your urine is pale yellow or clear.
What nutritional supplements are essential after bariatric surgery?
Key supplements include multivitamins, vitamin B12, iron, and calcium. They help prevent deficiencies and support health.
How do I manage food intolerances after bariatric surgery?
Manage food intolerances by avoiding trigger foods and introducing new foods slowly. Get guidance from a healthcare provider or nutritionist.
What is the long-term diet after gastric sleeve surgery?
The long-term diet focuses on balanced, nutrient-rich meals and enough protein. It also involves careful calorie management for weight loss and health.
How can I prevent weight regain after bariatric surgery?
To prevent weight regain, eat healthily, stay hydrated, exercise, and keep up with healthcare appointments.
What are the common nutritional challenges after bariatric surgery?
Common challenges include managing protein, preventing deficiencies, handling food intolerances, and keeping a balanced diet for health and weight loss.
References
National Health Service. (2021). Bariatric surgery – Eating. nhs.uk. https://www.nhs.uk/conditions/weight-loss-surgery/eating/







