Last Updated on December 3, 2025 by Bilal Hasdemir

At Liv Hospital, we know how key accurate diagnosis is in fighting brain tumors. High-quality brain cancer pictures and images are vital. They help doctors spot tumor types and how they grow.
We use MRI scans as the top choice for imaging. They show tumors clearly, helping doctors see their size, shape, and where they are. Our collection has 15 brain cancer MRI pictures and images. They show different tumor types and what they look like.
Looking at these brain tumour pics helps doctors and patients understand what’s going on. It also shows the treatment options. We aim to give top-notch healthcare, supporting patients from all over.
Key Takeaways
- High-quality brain cancer images aid in accurate diagnosis and treatment.
- MRI scans are the gold standard for imaging brain tumors.
- Our collection includes 15 brain cancer pictures and MRI images.
- Understanding tumor types and progression is key for good treatment.
- Liv Hospital offers full healthcare services for patients from abroad.
The Critical Role of Brain Cancer Pictures & Images
Brain tumors are now better understood thanks to imaging techniques. Pictures and images help doctors spot tumors early. This is key for planning treatments.
Today, we have thousands of brain cancer photos. These show different types of tumors like gliomas and meningiomas. This helps us understand brain cancer better.
How Medical Imaging Revolutionized Brain Tumor Detection
Medical imaging has changed neuro-oncology a lot. It lets doctors see tumors clearly. MRI and CT scans give detailed brain tumor pictures.
New imaging tech has made diagnosing better. It helps doctors plan treatments that fit each patient. Looking at mri pictures of brain cancer helps them know how big and where the tumor is.
Visual Diagnosis: From Symptoms to Confirmation
Diagnosing brain cancer involves several steps. Doctors look at pictures and patient history. Pictures are key in confirming diagnoses.
By studying brain cancer pictures, doctors can tell what kind of tumor it is. They can also see how serious it is. This helps them plan the best treatment.
Understanding MRI Brain Cancer Images
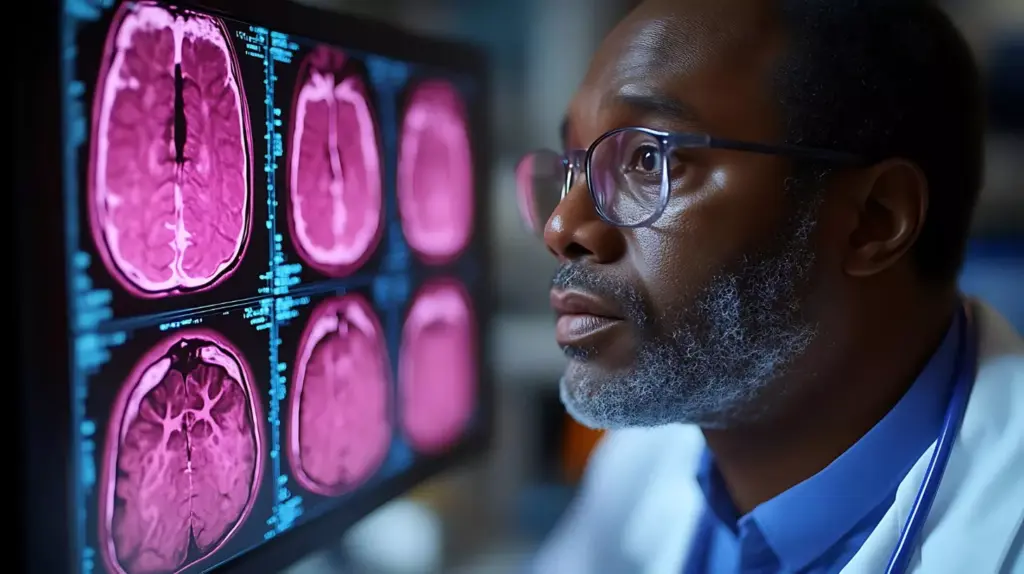
MRI images give us detailed views of brain tumors. They help doctors diagnose and plan treatments. MRI technology shows us the size, location, and structure of brain cancers.
How MRI Technology Creates Detailed Brain Tumor Visualizations
MRI uses strong magnetic fields and radio waves to show brain details. It’s a non-invasive way to see soft tissue tumors like brain cancers.
It works by aligning hydrogen atoms with a magnetic field. Radio waves disturb these atoms. As they return to their original state, they send signals that create detailed images.
T1 vs. T2 Weighted Images: What They Reveal
MRI scans can show different images based on hydrogen atom relaxation times. T1-weighted images are good for seeing brain anatomy. T2-weighted images are better at showing tissue changes.
T1-weighted images help spot tumors as dark spots. T2-weighted images show bright areas of inflammation or tumor growth.
| Image Type | Characteristics | Usefulness in Brain Cancer Diagnosis |
|---|---|---|
| T1-weighted | Clear view of anatomy, tumors appear dark | Useful for detecting tumors and assessing anatomy |
| T2-weighted | Sensitive to tissue pathology, tumors appear bright | Ideal for highlighting areas of inflammation or tumor growth |
Contrast Enhancement: Making Tumors Visible
Contrast enhancement uses a contrast agent, like gadolinium, to highlight brain areas. It’s great for making tumors stand out against the rest of the tissue.
The contrast agent goes to areas with broken blood-brain barriers, like tumors. This makes tumors visible on T1-weighted images. It helps doctors see tumor boundaries and find smaller lesions.
Glioblastoma Multiforme: The Most Aggressive Brain Cancer
Glioblastoma multiforme is a very aggressive brain cancer. It grows fast and is hard to treat. Quick diagnosis and effective treatment are key.
Understanding Glioblastoma Multiforme
Glioblastoma multiforme is known for its aggressive behavior and poor prognosis. Studies show it’s the most common and malignant brain tumor in adults. It has a median survival of about 15 months, even with aggressive treatment.
This highlights the need for early detection and new treatment methods.
Classic “Butterfly” Glioblastoma Crossing Hemispheres
Glioblastoma multiforme can cross the corpus callosum, showing a “butterfly” shape on scans. This makes it hard to treat because it affects both brain hemispheres.
Ring-Enhancing GBM with Central Necrosis
Glioblastoma multiforme often looks like a ring with dead tissue in the middle on MRI scans. This happens because the tumor grows faster than its blood supply. It leads to dead tissue in the center, surrounded by living tumor cells.
Multifocal Glioblastoma Appearance
In some cases, glioblastoma multiforme shows up as multiple distinct lesions. This makes treatment planning very challenging. It requires a detailed and personalized approach.
By looking at these imaging features, we can understand glioblastoma multiforme better. We can see the challenges it brings for diagnosis and treatment.
Low-Grade Glioma Visual Characteristics
Low-grade gliomas have unique visual signs that are key for correct diagnosis and treatment. These slow-growing tumors show special features on MRI images. This helps doctors tell them apart from more aggressive brain tumors.
We will look at the visual signs of low-grade gliomas, like diffuse astrocytoma and oligodendroglioma. We’ll see how they look on MRI images. This helps us understand the differences between low and high-grade gliomas. It leads to better diagnosis and treatment plans.
Diffuse Astrocytoma Without Enhancement
Diffuse astrocytomas are a type of low-grade glioma. They often don’t show much enhancement on MRI images. These tumors look homogeneous on T1-weighted images and are bright on T2-weighted images.
The lack of enhancement is a key sign. It helps doctors tell them apart from higher-grade gliomas. Higher-grade gliomas show more enhancement because they are more vascular.
Oligodendroglioma with Calcifications
Oligodendrogliomas are another type of low-grade glioma. They often have calcifications that show up on imaging studies. These calcifications look like punctate or coarse densities on CT scans.
They also have a special look on MRI, on gradient echo sequences. The presence of calcifications is a clue that helps doctors diagnose oligodendroglioma.
Visual Differences Between Low and High-Grade Gliomas
Low-grade gliomas look different from high-grade gliomas. Low-grade gliomas have a more homogeneous appearance and less swelling around them. High-grade gliomas, on the other hand, have uneven enhancement, necrosis, and more swelling.
Knowing these differences is important for accurate diagnosis and treatment planning. By studying the visual signs of low-grade gliomas on MRI images, we can better diagnose and manage these tumors. The unique features of diffuse astrocytoma and oligodendroglioma, among others, guide clinical decisions.
Meningioma: Most Common Benign Brain Tumor
Meningiomas are the most common type of benign brain tumor. They are often found by accident during scans for other issues. These tumors grow from the meninges, which protect the brain and spinal cord. Knowing about meningiomas helps doctors diagnose and treat them better.
Typical Dural-Based Meningioma
A typical meningioma starts from the dura mater, the outermost meningeal layer. This is a key sign for doctors. These tumors grow slowly and might not cause symptoms for a long time.
On MRI, meningiomas look like a well-defined mass with a wide dural base. They show up clearly on T1-weighted images with contrast.
Falcine Meningioma in Parasagittal Location
Falcine meningiomas grow from the falx cerebri, a dural fold between the brain’s hemispheres. They are in the parasagittal area and can grow big before causing symptoms. This is because they grow slowly.
When symptoms do appear, they might include headaches, seizures, or neurological problems. MRI is used to diagnose these tumors and see how they affect the brain.
Calcified Meningioma Appearance
Some meningiomas have calcium deposits, known as calcifications. These are visible on CT scans. Calcified meningiomas look different on scans.
Calcifications help doctors tell meningiomas apart from other brain tumors. But, treating calcified meningiomas is similar to treating non-calcified ones. The focus is on watching them or removing them surgically, based on their size, location, and symptoms.
| Characteristics | Dural-Based Meningioma | Falcine Meningioma | Calcified Meningioma |
|---|---|---|---|
| Location | Dura mater | Falx cerebri | Variable, with calcifications |
| Growth Rate | Slow | Slow | Slow |
| Diagnostic Features | Broad dural attachment, intense enhancement | Parasagittal location | Presence of calcifications on CT |
Pituitary Adenoma Imaging Features
Understanding the imaging features of pituitary adenomas is key for accurate diagnosis and treatment planning. These benign tumors occur in the pituitary gland. Their size and location greatly impact patient health.
Pituitary adenomas are classified by size. Microadenomas are less than 10 mm, and macroadenomas are 10 mm or larger. Knowing the size is important because it affects symptoms and treatment.
Microadenoma vs. Macroadenoma Comparison
Microadenomas are small and may not cause many symptoms unless they secrete excess hormones. Macroadenomas, being larger, can press on nearby structures. This can lead to visual problems and other neurological symptoms.
| Characteristics | Microadenoma | Macroadenoma |
|---|---|---|
| Size | Less than 10 mm | 10 mm or larger |
| Symptoms | Often hormonal imbalances | May include visual disturbances, headaches |
| Treatment Approach | Often medical management | May require surgery or radiation |
Pituitary Tumor with Suprasellar Extension
Pituitary adenomas with suprasellar extension can press on the optic chiasm. This can cause visual field defects. Imaging is key to assess this compression and plan treatment.
The extent of suprasellar extension is important for surgery planning. Tumors with significant extension may need a craniotomy or an extended endoscopic endonasal approach.
Visual Clues of Cavernous Sinus Invasion
Cavernous sinus invasion by a pituitary adenoma makes surgery harder and affects treatment outcomes. Imaging shows if the tumor encases the carotid artery or extends into the sinus.
We use MRI to check the tumor’s relation to the cavernous sinus. Invasion can change treatment plans, often to more conservative methods or adjuvant therapies.
Metastatic Brain Cancer Visual Patterns
Understanding the visual patterns of metastatic brain cancer is key for accurate diagnosis and treatment planning. This type of cancer happens when cancer cells from other parts of the body spread to the brain. These cancers often start in places like the lung, breast, or skin.
Advanced imaging, like MRI, is very important in finding and understanding these metastases. The look of metastatic brain cancer on scans can change a lot. This depends on the type of cancer it started from, how many metastases there are, and where they are in the brain.
Multiple Metastases from Lung Cancer
Lung cancer is a big source of brain metastases. When there are many metastases, scans show several distinct lesions in the brain. These lesions usually have clear edges and different sizes.
Having many metastases means the cancer is likely in a more advanced stage. This requires a detailed treatment plan. It might include radiation, chemotherapy, and targeted therapy.
Solitary Metastasis with Surrounding Edema
A solitary metastasis is a single brain lesion from cancer spread. On scans, it looks like a distinct, rounded lesion with swelling around it. This swelling can make symptoms worse.
It’s very important to identify a solitary metastasis. It might be treatable with surgery or radiosurgery. Advanced imaging helps tell the difference between tumor and swelling, helping decide the best treatment.
Hemorrhagic Metastasis from Melanoma
Some metastases, like those from melanoma, can bleed. On MRI, these look complex with mixed signals because of the blood.
Bleeding in a metastasis makes diagnosis and treatment harder. It might need quick action and can affect treatment choices.
| Metastasis Type | Common Primary Tumor | Typical Imaging Features |
|---|---|---|
| Multiple Metastases | Lung Cancer | Multiple distinct lesions, varying sizes |
| Solitary Metastasis | Various (including Breast, Lung) | Single lesion with surrounding edema |
| Hemorrhagic Metastasis | Melanoma | Complex appearance with mixed signal intensities |
By looking at the visual patterns of metastatic brain cancer, we can understand the disease better. This helps tailor treatments to each patient’s needs.
Pediatric Brain Tumor Imaging
Imaging is key in finding and treating brain tumors in kids. We use top-notch imaging to spot and manage these tough tumors.
Brain tumors in kids can pop up in different spots, like the back of the brain and the ventricles. Medulloblastoma and ependymoma are the most common, each showing unique signs on scans.
Image 14: Medulloblastoma in the Posterior Fossa
It shows up as a clear mass in the back of the brain, often blocking the fourth ventricle. After contrast, it looks different, helping us tell it apart from other tumors.
- Typically located in the midline cerebellum
- Often fills and obstructs the fourth ventricle
- Heterogeneous enhancement on MRI
Image 15: Ependymoma Extending from Ventricles
Ependymoma starts in the lining of the ventricles. Ependymomas can spread through the fourth ventricle’s openings, making surgery tough. They look like mixed masses with spots and cysts on scans.
“Ependymomas are known for their variable appearance on imaging, making diagnosis challenging.” – Expert in Pediatric Neuroimaging
Special Considerations in Pediatric Neuroimaging
Imaging kids’ brains needs special care because their brains are growing. We aim to get accurate diagnoses without harming the developing brain. Advanced MRI, like diffusion-weighted imaging and MR spectroscopy, helps us do this without radiation.
We think about the child’s age, where the tumor is, and if it might spread. We want to diagnose accurately while keeping risks low and outcomes great for kids.
Advanced Diagnostic Imaging for Brain Tumors
Advanced imaging has changed how we diagnose and treat brain tumors. These new tools let us see brain activity, tumor structures, and metabolic changes. This helps us understand brain cancers better.
Mapping Brain Activity Around Tumors
Functional MRI (fMRI) is key in diagnosing and planning treatment for brain tumors. It shows how brain activity changes around tumors. This info is essential for surgery, helping surgeons remove tumors safely.
A leading neurosurgeon says, “fMRI is vital for treating brain tumors. It helps us remove tumors effectively without harming the brain.”
Visualizing White Matter Tracts
Diffusion Tensor Imaging (DTI) shows important details about white matter tracts in the brain. It helps surgeons navigate during surgery. This is key for tumors near critical areas, where brain function must be preserved.
- DTI helps identify the relationship between tumors and adjacent white matter tracts.
- It aids in surgical planning by providing detailed information about brain anatomy.
- DTI can help predict possible neurological deficits after surgery.
Metabolic Activity in Brain Cancers
PET scans show how brain tumors use energy, adding to MRI’s view. They help tell tumor types, how aggressive they are, and how well they respond to treatment. A study found, “PET imaging is a powerful tool for brain tumor diagnosis and monitoring.”
Using these advanced imaging methods together gives us a deeper understanding of brain tumors. This approach improves diagnosis, treatment planning, and patient care.
Conclusion: The Evolution and Future of Brain Tumor Imaging
Brain tumor imaging is key in finding and treating brain cancers. This field is growing fast, thanks to new research and tools.
New ways to see tumors are helping doctors plan treatments better. The future looks bright, with tech like artificial intelligence making images even clearer.
We’ll see more progress in brain tumor imaging soon. This means better care for patients. Doctors will use the newest tech to make treatment choices.
FAQ
What is the importance of brain cancer pictures and MRI images in diagnosis?
Brain cancer pictures and MRI images are key in finding and diagnosing brain tumors. They help doctors see tumors clearly. This helps them plan the best treatment.
How does MRI technology create detailed visualizations of brain tumors?
MRI technology uses different images, like T1 and T2, and contrast to show tumors. This makes it easier to see the tumors’ details.
What are the visual characteristics of glioblastoma multiforme?
Glioblastoma multiforme shows a “butterfly” pattern, ring-enhancing lesions, and can appear in many places. These signs help doctors diagnose and plan treatment.
How do low-grade gliomas appear on MRI images?
Low-grade gliomas, like diffuse astrocytoma and oligodendroglioma, look like non-enhancing or slightly-enhancing spots. Oligodendroglioma might have calcifications.
What are the typical imaging features of meningiomas?
Meningiomas are usually found on the dura, often with calcifications. They might show a “dural tail” sign on MRI images.
How are pituitary adenomas visualized on MRI images?
Pituitary adenomas are seen on MRI by their size and where they spread. Microadenomas are small, and macroadenomas are larger. They can grow into nearby areas.
What are the visual patterns of metastatic brain cancer on MRI images?
Metastatic brain cancer can look like many spots, one big spot, or spots with bleeding. They often have swelling around them, making them easy to spot on MRI.
How do pediatric brain tumors appear on MRI images?
Pediatric brain tumors, like medulloblastoma and ependymoma, have unique looks on MRI. Their location and how they appear help doctors diagnose and plan treatment.
What is the role of advanced diagnostic imaging techniques in brain tumor diagnosis?
Advanced imaging, like functional MRI and PET scans, gives more details about brain tumors. This helps doctors diagnose and plan treatment better.
What is the future of brain tumor imaging?
The future of brain tumor imaging looks bright. We can expect better image quality, more accurate diagnoses, and better treatment results. This will help doctors give the best care to patients with brain tumors.





