Heart stents are small mesh tubes used to open narrowed or blocked arteries, helping to restore proper blood flow. However, some patients wonder, “do stents move?” It’s a common concern, especially after stent placement.
At Liv Hospital, Turkey’s leading healthcare provider, we understand how serious these issues can be. In this article, we’ll discuss the possible risks of heart stents, including what happens if a stent becomes blocked or shifts from its original position.
We’ll also explore the latest treatments and share expert advice to help you stay informed. Understanding the facts about “do stents move” and other stent-related concerns is essential for anyone living with a heart stent. Our goal is to help you feel confident and supported in your heart care journey.
Key Takeaways
- Heart stents can become blocked or displaced, leading to serious complications.
- Understanding the risks and latest treatments is key for patients with heart stents.
- Liv Hospital offers full care and advice for heart stent patients.
- Patients should know about the chance of stent replacement or blockage.
- Expert insights and the latest treatments help patients make smart choices.
Understanding Heart Stents and Their Purpose
Heart stents have changed how we treat coronary artery disease. They offer a less invasive way to help patients. These devices are key in keeping the arteries open for those with coronary artery disease.
What Are Heart Stents?
Heart stents are small, mesh-like tubes made of metal or other materials. They are used to keep arteries open after an angioplasty procedure. This helps improve blood flow to the heart, easing symptoms like chest pain and shortness of breath.
How Heart Stents Treat Coronary Artery Disease
Coronary artery disease (CAD) happens when arteries narrow or block due to plaque buildup. Heart stents treat CAD by keeping arteries open. According to Boston Scientific, stents keep the artery open, improving blood flow to the heart.
- Stents reduce the risk of artery closure
- They alleviate symptoms such as chest pain and shortness of breath
- Stents can improve overall heart health by ensuring adequate blood flow
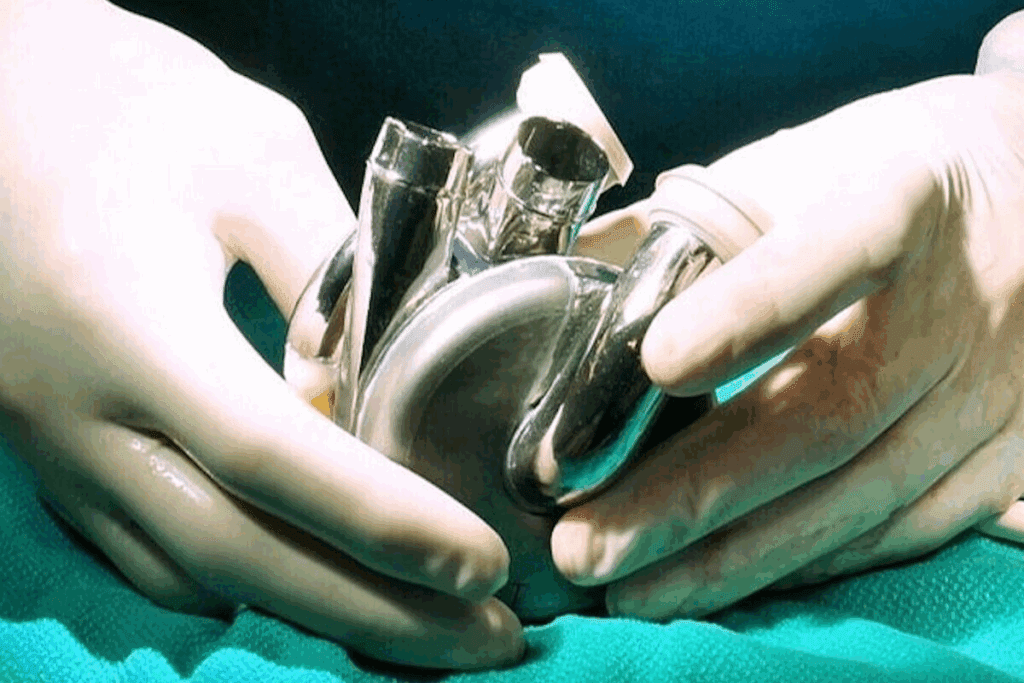
The Placement Procedure
The placement of a heart stent involves angioplasty. A catheter is inserted into the narrowed artery, and a balloon is inflated to widen it. Then, the stent is placed to keep the artery open. This is done under local anesthesia, and most patients go home the same day.
It’s important for patients to understand heart stents’ role in treating coronary artery disease. Knowing how stents work and what to expect during the procedure helps patients make informed decisions about their care.
Types of Heart Stents and Their Differences
There are many types of heart stents, each for different needs. The right stent depends on the patient’s health, disease severity, and the doctor’s advice.
Bare-Metal Stents
Bare-metal stents are made of metal mesh. They keep the artery open after angioplasty. They are:
- Made from stainless steel or other metals
- Less expensive than drug-eluting stents
- Require dual antiplatelet therapy for at least one month
But, bare-metal stents have a higher chance of restenosis than drug-eluting stents.
Drug-Eluting Stents
Drug-eluting stents have a special coating that prevents new tissue growth. This reduces the risk of restenosis. They:
- Release medication slowly over time
- Have a lower risk of restenosis compared to bare-metal stents
- Require dual antiplatelet therapy for a longer period, typically 6-12 months
Doctors often choose drug-eluting stents for complex cases or past stent failures.
Bioabsorbable Stents
Bioabsorbable stents are made to dissolve in the body over time. They:
- Provide temporary scaffolding to the artery
- Reduce the risk of long-term complications associated with metal stents
- Are being studied in clinical trials to assess their long-term efficacy
Bioabsorbable stents might be a better option than metal stents, possibly avoiding long-term antiplatelet therapy.
In summary, the type of heart stent used greatly affects treatment success for coronary artery disease. Knowing the differences between bare-metal, drug-eluting, and bioabsorbable stents helps doctors make better choices for their patients.
Coronary Artery Disease and Stent Treatment
Coronary artery disease is a major cause of heart problems. Stent treatment can help manage it, improving patient health. CAD happens when the heart’s main blood vessels get damaged or diseased. This damage is often due to plaque buildup.
Plaque is made of fat, cholesterol, and other materials. It can reduce blood flow to the heart. This can cause chest pain, shortness of breath, and other symptoms.
Understanding CAD and Its Progression
CAD can quietly progress for years. Some people don’t show symptoms until it’s too late. The disease gets worse as plaque builds up in the arteries.
High blood pressure, high cholesterol, smoking, diabetes, and family history of heart disease can make CAD worse.
Risk Factors for CAD Progression:
- High Blood Pressure
- High Cholesterol
- Smoking
- Diabetes
- Family History of Heart Disease
How Stents Address CAD Symptoms
Stents are small, mesh tubes that open up blocked arteries. They help restore blood flow to the heart. This can greatly reduce CAD symptoms, improving life quality.
Stent placement is a minimally invasive procedure called PCI. A catheter guides the stent to the blocked artery. Once in place, it expands to keep the artery open.
Long-term Management of CAD with Stents
Managing CAD with stents requires lifestyle changes, medication, and sometimes more procedures. Patients often take antiplatelet therapy to prevent blood clots. Regular check-ups are key to monitor the stent’s success and the arteries’ health.
| Management Strategy | Description |
| Lifestyle Changes | Dietary modifications, increased physical activity, smoking cessation |
| Medication | Antiplatelet therapy, cholesterol-lowering medications, beta-blockers |
| Regular Follow-Up | Monitoring stent effectiveness, overall coronary artery health |
When a Stent Gets Clogged: Restenosis Explained
Restenosis is when a stented artery gets narrower again. It’s a big worry for people with coronary artery disease. Knowing about it is key for those who’ve had stents put in.
What Is Restenosis?
Restenosis is when an artery gets narrow again after a stent is placed. It can cause chest pain to come back. It happens when cells grow inside the stent, making the artery smaller.
Risk Factors for Restenosis
There are several things that can make restenosis more likely. These include:
- Small stent size
- Long lesions
- Diabetes
- History of restenosis
Knowing these risk factors can help lower the chance of restenosis.
How Modern Stent Designs Reduce Restenosis Risk
New stent technology has made drug-eluting stents. These stents release medicine to stop cells from growing. This has greatly cut down on restenosis.
| Stent Type | Restenosis Rate | Description |
| Bare-Metal Stents | Higher | No drug elution; higher risk of tissue growth |
| Drug-Eluting Stents | Lower | Release medication to prevent tissue growth |
Understanding restenosis and its risks helps patients and doctors work together. This way, they can lower its chances and manage its effects.
Stent Thrombosis: Blood Clots and Your Stent
When a blood clot forms inside a stent, it’s called stent thrombosis. This is a serious condition that can be life-threatening. It’s important for patients with coronary stents to know the risks and how to prevent them.
Understanding Stent Thrombosis
Stent thrombosis is when a blood clot blocks the stent. This can cut off blood flow to the heart. It can lead to a heart attack or even death if not treated quickly.
The risk of stent thrombosis is higher in the first few months. But it can happen at any time.
We will discuss the different types of stent thrombosis. We’ll look at how they are classified based on when they happen.
Acute vs. Late Stent Thrombosis
Stent thrombosis is divided into two types based on when it happens. Acute stent thrombosis occurs within 24 hours. Late stent thrombosis happens after that.
Acute stent thrombosis is often due to problems during stent placement. Late stent thrombosis may be caused by stopping antiplatelet therapy or new lesions.
Preventive Measures and Medications
Preventing stent thrombosis is key for patients with coronary stents. Taking prescribed antiplatelet medications is important. These drugs stop platelets from sticking together and forming clots.
Regular check-ups with your doctor are also vital. Monitoring for stent thrombosis and addressing concerns quickly can improve outcomes. Quitting smoking and eating healthy are also important for your heart health.
Knowing the symptoms of stent thrombosis is also important. These include chest pain, shortness of breath, or signs of a heart attack. If you experience these symptoms, seek medical help right away.
Can Heart Stents Move Out of Place?
Patients often worry if their heart stent can move. We’re here to clear up any doubts.
Heart stents are meant to stay in the artery forever. They keep the artery open to improve blood flow. Though stents are placed carefully, sometimes they can move.
Causes of Stent Movement
Stent movement is rare but can happen for a few reasons. These include:
- Improper deployment during the initial procedure
- Vessel size mismatch, where the stent is not appropriately sized for the artery
- Mechanical forces within the artery that can cause the stent to migrate
A study in the Journal of the American College of Cardiology found stent migration is rare. This shows how important correct stent sizing and deployment are.
“The key to minimizing stent movement lies in precise procedural techniques and appropriate patient selection.”
Medical Expert, Interventional Cardiologist
Symptoms of Displaced Stents
If a stent moves, patients might notice some symptoms. These include:
| Symptom | Description |
| Chest Pain | Recurring or new chest pain due to the stent not being in its correct position |
| Shortness of Breath | Difficulty breathing or feeling winded even at rest |
| Abnormal Heartbeat | Palpitations or irregular heart rhythms |
Treatment for Stent Displacement
If a stent moves, treatment is needed. Options include:
- Additional stenting to correct the displacement and ensure proper blood flow
- Balloon angioplasty to adjust the stent’s position
- In some cases, more invasive procedures like coronary artery bypass grafting (CABG) may be considered
Patients should see their doctor if they have symptoms that might mean their stent has moved.
We tell our patients that while stent movement is possible, it’s rare. Most stents stay in place and work well, greatly improving patients’ lives.
Recognizing Stent Failure Symptoms
It’s important to know the signs of stent failure to get help quickly. A failed stent can cause serious health problems. So, spotting symptoms early is key.
Recurring Chest Pain and Angina
Chest pain or angina coming back is a big sign of stent failure. This pain might feel like what you had before the stent. If you feel chest pain again, see your doctor right away.
Common signs of angina from a failed stent include:
- Discomfort or pain in the chest, arms, back, neck, jaw, or stomach
- Pain that happens when you’re active or stressed
- Pain that goes away when you rest or take medicine
Shortness of Breath and Other Warning Signs
Other signs of stent failure include shortness of breath, feeling very tired, and swelling in your legs or feet. Don’t ignore these symptoms. They mean you need to see a doctor fast.
A medical expert says, “Spotting stent failure symptoms early can really help patients.”
“The key to managing stent failure lies in early detection and appropriate intervention.”
When to Seek Emergency Care
If you have severe chest pain, trouble breathing, or other serious symptoms, call for emergency help right away. These could be signs of a heart attack.
| Symptom | Description | Action |
| Severe Chest Pain | Crushing or squeezing sensation in the chest | Call emergency services |
| Shortness of Breath | Difficulty breathing or feeling winded at rest | Seek immediate medical attention |
| Dizziness or Fainting | Feeling lightheaded or passing out | Consult a healthcare provider urgently |
Knowing the signs of stent failure is vital for your heart health. If you notice anything odd, contact your doctor without delay.
Diagnosing Problems with Existing Stents
To check on heart stents, we use advanced methods. We look at how well stents work and any problems they might have. This is done through different imaging techniques.
Imaging Techniques for Stent Evaluation
There are several ways to check on heart stents. These include:
- Angiography: Gives clear pictures of the arteries and stent.
- Intravascular Ultrasound (IVUS): Shows detailed images of the stent and the artery around it.
- Optical Coherence Tomography (OCT): Provides detailed views of the stent and artery.
| Imaging Technique | Description | Benefits |
| Angiography | Detailed images of coronary arteries and stent | Checks if the stent is open and finds blockages |
| IVUS | High-resolution images of stent and artery | Looks at how well the stent fits and finds problems like restenosis |
| OCT | Detailed cross-sectional images of stent and artery | Measures stent size accurately and finds small issues |
Are Stents Visible on Chest X-rays?
Most stents show up on chest X-rays. But, how well they show depends on the stent’s material and design. For example, coronary stents made from certain metals are easier to see.
MRI Compatibility with Heart Stents
Most heart stents are safe for MRI scans. But, it’s important to tell your doctor before getting an MRI.
Always check with your doctor about your stent’s MRI safety. This helps ensure safe and accurate imaging.
How to Know If You Need a Stent
Are you feeling chest pain or shortness of breath? You might wonder if you need a stent. We’ll help you figure out if a stent is the right choice for you.
Common Symptoms Indicating Stent Necessity
Some symptoms suggest you might need a stent. These include:
- Chest Pain (Angina): Feeling pain or discomfort in your chest that spreads to your arms, back, neck, jaw, or stomach.
- Shortness of Breath: Feeling like you can’t catch your breath, even when you’re sitting or lying down.
- Fatigue: Feeling extremely tired or weak, even after resting.
These symptoms often point to coronary artery disease (CAD). This is when your arteries get narrowed or blocked by plaque.
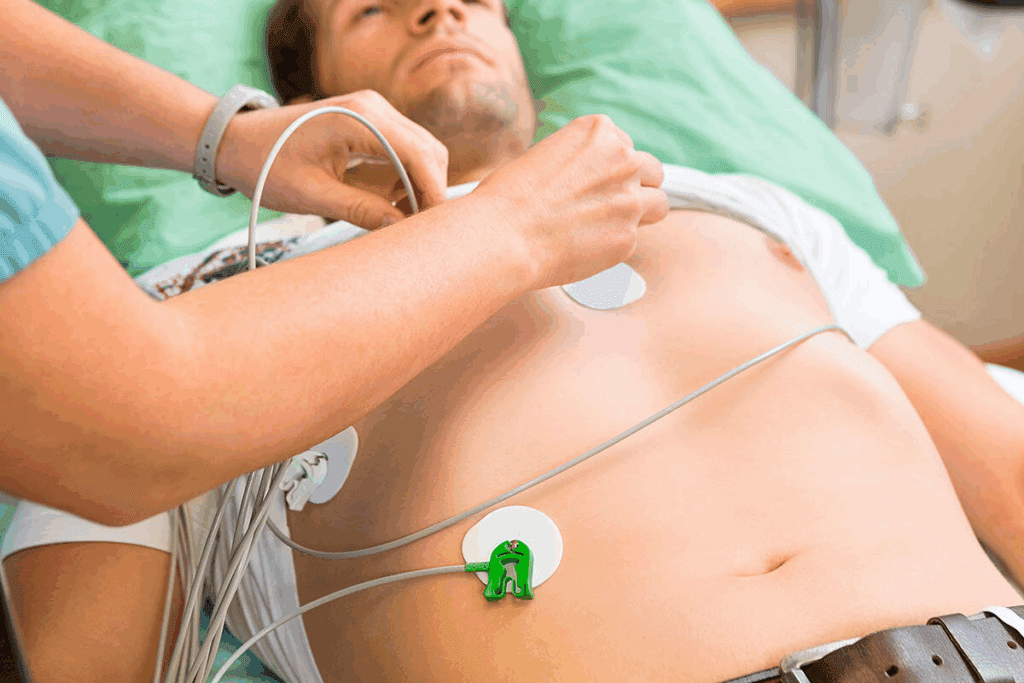
Diagnostic Tests for Determining Stent Need
Your doctor might suggest several tests to see if you need a stent:
- Stress Test: This test checks how your heart works when you’re active.
- Coronary Angiography: This uses dye and X-rays to see your coronary arteries and find blockages.
- Electrocardiogram (ECG or EKG): This records your heart’s electrical activity.
These tests help your doctor understand how severe your CAD is. They’ll then decide if a stent is needed.
Discussing Stent Options with Your Doctor
If tests show you need a stent, talk to your doctor about your options. Here are important things to consider:
- Type of Stent: There are bare-metal and drug-eluting stents, each with its own benefits and risks.
- Procedure Details: Learn about the stent placement process, including its risks and benefits.
- Lifestyle Changes: Find out about the lifestyle changes you might need to make after getting a stent.
By talking to your doctor, you can make a well-informed decision about getting a stent.
Treatment Options for Failed or Blocked Stents
When a heart stent fails or gets blocked, there are several ways to fix it. The right treatment depends on how bad the blockage is, the patient’s health, and the stent type.
Medication Adjustments
Changing medications can sometimes help. We might adjust antiplatelet drugs to stop clots or other meds for underlying issues causing stent failure.
Balloon Angioplasty for Restenosis
Balloon angioplasty is a common fix for stent restenosis. A small balloon is used to widen the artery. This can help restore blood flow and ease symptoms.
Placing a New Stent Inside the Old One
In some cases, we might put a new stent inside the old one. This “stent-in-stent” method works well for complex blockages. It helps open the artery more and improves blood flow.
Bypass Surgery as an Alternative
For complex or multiple blockages, or when other methods don’t work, CABG surgery might be needed. CABG creates a bypass around the blocked artery. This improves blood flow to the heart.
Talking to a healthcare provider is key to finding the right treatment for failed or blocked stents. Every case is different, and a tailored approach is best.
- Medication adjustments can help manage symptoms and potentially improve stent function.
- Balloon angioplasty is used to treat restenosis within a stent.
- Placing a new stent inside the old one can be effective for complex blockages.
- Bypass surgery is considered for complex or multiple blockages.
Conclusion
It’s important to know about the problems that can happen with heart stents. These include a stent getting clogged or blocked. Many things can cause these issues, like restenosis and stent thrombosis.
For patients with heart stents, getting regular check-ups is key. Taking your medicine as told is also very important. If a stent does get blocked, doctors might use balloon angioplasty or replace the stent.
At Liv Hospital, we aim to give top-notch care to our patients. Our skilled cardiologists and healthcare team offer full support and advice. By being informed and proactive, patients can lower the risks of heart stent problems and keep their heart healthy.
FAQ
Can stents move out of place?
Stents can rarely move out of place. This might happen due to bad placement or stress on the stent. If this happens, you might feel chest pain or have trouble breathing. You should see a doctor right away.
Can you have an MRI with heart stents?
Most heart stents work well with MRI scans. But, always tell your doctor about your stent before getting an MRI. This ensures your safety and the MRI’s compatibility.
How do you know if you need a stent?
Doctors use tests like angiograms and echocardiograms to check for blockages. Symptoms like chest pain or shortness of breath also hint at the need for a stent.
What happens if a stent gets blocked?
A blocked stent can cause serious problems like chest pain or even a heart attack. You need to see a doctor quickly to fix the blockage.
Are stents visible on chest X-rays?
Yes, most stents show up on chest X-rays. This helps doctors check if the stent is in the right place. But, the visibility can depend on the stent’s material and design.
What are the symptoms of stent failure?
Signs of stent failure include chest pain, shortness of breath, or other heart flow issues. If you notice these symptoms, get medical help fast.
Can a stent be placed inside another stent?
Yes, sometimes a new stent is put inside an old one. This is done during an angioplasty to fix problems like restenosis.
How do you feel when you need a stent?
You might feel chest pain, shortness of breath, or get tired easily. These signs mean your heart isn’t getting enough blood. A stent can help fix this.
What is stent thrombosis?
Stent thrombosis is when a blood clot forms in the stent. It’s a serious issue that needs quick medical help. It might involve changing medications or doing more procedures.
Can CAD be managed with stents?
Yes, stents are key in managing coronary artery disease. They keep arteries open and improve blood flow. But, managing CAD also involves lifestyle changes and other treatments.
References
- Jang, S., & Lee, W. (2024). The NITRATE-OCT study: Inorganic nitrate reduces in-stent restenosis. The Lancet Regional Health – Europe. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00464-4/fulltext










