When you’re diagnosed with heart disease, learning about treatments like the cardiac balloon procedure can help. It makes you feel more confident in your medical choices.
This method, also called cardiac balloon procedure or percutaneous coronary intervention (PCI), opens up blocked arteries. It’s used when arteries get narrow or blocked, often because of atherosclerosis.
Key Takeaways
- Understanding the cardiac balloon procedure can aid in medical decision-making.
- Balloon angioplasty is a minimally invasive treatment for narrowed or blocked coronary arteries.
- The procedure is also known as percutaneous coronary intervention (PCI).
- Atherosclerosis is a common cause of narrowed or blocked coronary arteries.
- Leading medical centers like Liv Hospital offer this treatment with a focus on patient care.
What is a Cardiac Balloon Procedure?

The cardiac balloon procedure, also known as balloon angioplasty, is a new way to treat narrowed arteries. It’s less invasive than old surgical methods. This makes it a big help in managing coronary artery disease.
Definition and Basic Concept
A balloon catheter is used in this procedure. It’s guided through a blood vessel to the narrowed area. Then, the balloon is inflated to open the artery, improving blood flow.
As the NIH explains, angioplasty makes the artery wider. This lets more blood flow, easing symptoms of coronary artery disease.
Common Names and Terminology
This procedure is also called balloon angioplasty or just angioplasty. It’s important to know these terms are often used the same way. Percutaneous transluminal angioplasty (PTCA) and coronary angioplasty are specific types used in coronary arteries.
The History and Evolution of Balloon Angioplasty
Charles Dotter’s work laid the foundation for balloon angioplasty in treating coronary artery disease. The balloon angioplasty procedure has seen many changes over the years.
Charles Dotter is known as the father of balloon cardiology. He introduced angioplasty in the 1960s. He used a catheter to widen narrowed arteries, starting a new era in treatments.
Early Development of the Technique
The early days of balloon angioplasty were filled with important milestones. At first, many doubted its success. But as technology got better and techniques improved, it became widely accepted.
The first successful angioplasty procedures were key. They showed that heart balloon procedures could be effective. This made balloon angioplasty a recognized treatment for coronary artery disease.
Modern Advancements in Technology
Recently, balloon cardiology has seen big improvements. Drug-coated stents and better balloon designs have been developed. These aim to lower the risk of complications and improve results for patients.
New technologies have been introduced, such as:
- Drug-eluting stents that reduce the risk of restenosis
- Advanced balloon materials that are more flexible and durable
- Improved imaging techniques for better stent placement
| Year | Milestone | Description |
| 1964 | First Angioplasty | Charles Dotter performs the first angioplasty on a human |
| 1977 | First Coronary Angioplasty | Andreas Gruentzig performs the first coronary angioplasty |
| 1990s | Stent Development | Introduction of stents to keep arteries open |
| 2000s | Drug-Eluting Stents | Development of drug-eluting stents to reduce restenosis |
The journey of balloon angioplasty is ongoing. Research and development keep pushing the boundaries of safety and effectiveness. As we look to the future, it’s clear that balloon angioplasty procedure will continue to play a vital role in heart care.
Understanding Coronary Artery Disease
To understand the importance of the cardiac balloon procedure, we must first grasp what it treats. Coronary artery disease affects the major blood vessels that feed the heart. The NHLBI explains that atherosclerosis, or plaque buildup, narrows or blocks these arteries.
Atherosclerosis and Plaque Formation
Atherosclerosis is when plaque, a mix of fat, cholesterol, and more, builds up in arteries. This buildup can narrow or block the arteries, cutting off blood to the heart. The cardiac balloon procedure helps by easing symptoms of angina and reducing heart damage during or after a heart attack.
The plaque formation process involves several steps:
- Damage to the inner artery layer
- Accumulation of lipids and inflammatory cells
- Formation of a fibrous cap over the plaque
- Potential rupture of the plaque, leading to a blockage
Symptoms and Diagnostic Methods
Coronary artery disease often develops slowly and may not show symptoms until a heart attack. Common symptoms include:
- Chest pain (angina)
- Shortness of breath
- Fatigue
- Pain or discomfort in the arms, back, neck, jaw, or stomach
Diagnostic methods for coronary artery disease include:
- Electrocardiogram (ECG or EKG): Measures the heart’s electrical activity.
- Stress Test: Checks how the heart works during activity.
- Coronary Angiography: Uses dye and X-rays to see the arteries.
- Cardiac CT Scan: Gives detailed images of the heart and its vessels.
Understanding coronary artery disease is key to seeing the cardiac balloon procedure’s role. It helps manage and treat the condition by addressing artery blockages. This can greatly improve heart health and lower the risk of heart attacks.
Medical Indications for the Cardiac Balloon Procedure
We use the cardiac balloon procedure for several important medical reasons. It helps restore blood flow to the heart. This is a key treatment for many heart conditions, giving patients relief and treatment options.
Treating Stable Angina
Stable angina causes chest pain or discomfort due to blocked arteries. The cardiac balloon procedure is often suggested for this condition. It aims to improve blood flow to the heart muscle.
The American Heart Association says angioplasty helps reduce chest pain from artery blockages.
Using the cardiac balloon procedure for stable angina has many benefits:
- Less frequent and severe angina episodes
- Improved quality of life through better physical ability
- Better overall heart health
Emergency Treatment During Heart Attacks
During a heart attack, quick action is vital. The balloon catheter angioplasty is a lifesaving procedure. It helps restore blood flow to the heart’s affected area.
The American College of Cardiology says primary PCI, which includes balloon angioplasty, is the best treatment for heart attacks. This is when it can be done quickly by skilled operators.
“Primary PCI is recommended over fibrinolytic therapy when it can be performed in a timely manner by experienced operators.”
Other Clinical Scenarios
The heart procedure balloon is also used in other situations. These include:
- In-stent restenosis, where a stent becomes blocked
- Complex coronary artery disease, with multiple blockages or hard-to-reach areas
The cardiac balloon procedure is a key treatment for coronary artery disease. It has greatly improved how we manage this condition. Knowing when to use it helps both patients and doctors make better choices.
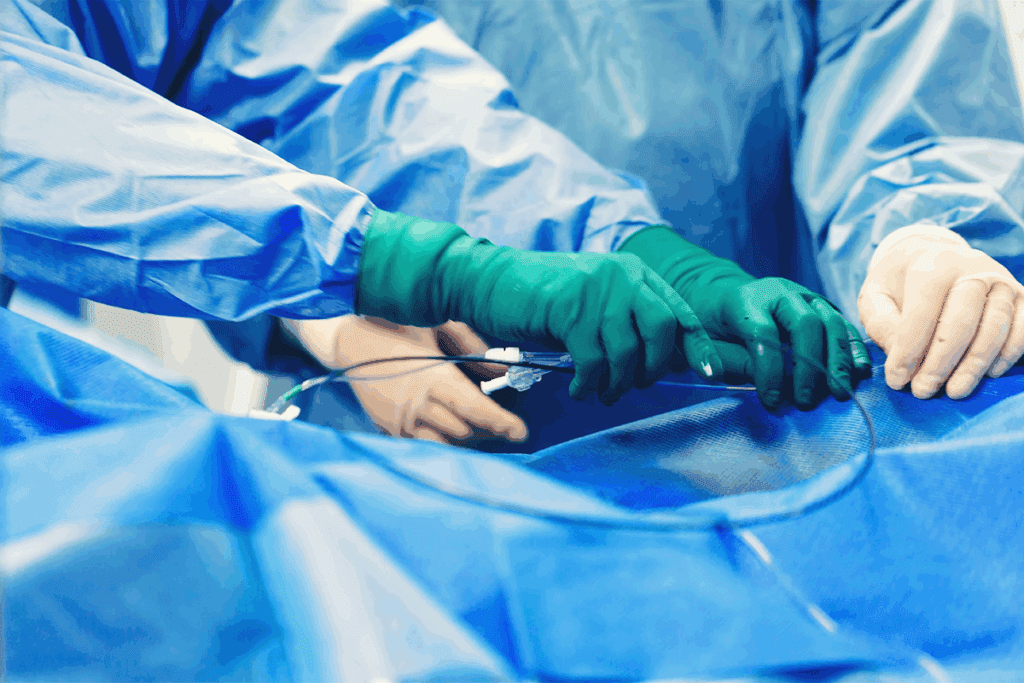
The Equipment Used in Balloon Angioplasty
Knowing about the tools in balloon angioplasty helps us see how complex it is. This treatment is made possible by advanced technology. This includes balloon catheters and stents.
Types of Balloon Catheters
Balloon catheters are key in angioplasty. They have a balloon tip that inflates to push plaque against artery walls. This improves blood flow. There are many types of balloon catheters, each for different needs.
Some key features of balloon catheters are:
- Diameter and length made for each patient
- Materials for flexibility and strength
- Safe inflation pressure
We use these catheters to move through arteries with care. We make sure the balloon is right at the blockage.
Stent Technology
A stent, a small mesh tube, is often used during angioplasty. It keeps the artery open. The National Heart, Lung, and Blood Institute says stents support the artery and improve blood flow.
There are different stents, like:
| Stent Type | Description | Clinical Use |
| Bare-metal stents | Simple metal mesh | Commonly used for straightforward cases |
| Drug-eluting stents | Coated with medication to prevent restenosis | Used for patients at higher risk of artery re-narrowing |
| Bioresorbable stents | Absorbable material that dissolves over time | Ideal for certain patient groups, reducing long-term complications |
The right stent depends on the patient’s history and the blockage’s details.
Understanding the tools in balloon angioplasty shows how detailed this life-saving procedure is. The mix of advanced balloon catheters and stents has changed how we treat heart disease.
Preparing for Your Cardiac Balloon Procedure
Getting ready for your cardiac balloon procedure is key. Your healthcare team will guide you every step of the way. They want to make sure your experience is smooth and successful.
Pre-Procedure Testing and Evaluation
Before your cardiac balloon catheter procedure, tests will check your heart. You might have blood tests, ECGs, and imaging like X-rays or ultrasounds. These tests help figure out how bad your heart disease is and if there are risks.
It’s important to follow your doctor’s instructions for these tests. This ensures you get accurate results. Your doctor will also ask about your medical history. This includes any allergies or past reactions to medicines.
Medication Adjustments
Your doctor might tell you to change your medications before the balloon catheterization procedure. This could mean stopping some medicines that might make bleeding more likely or interact with the procedure’s drugs. Tell your healthcare team about all your medicines, including blood thinners and diabetes drugs.
Following your doctor’s advice on medication changes is key. It helps reduce risks and makes the procedure more likely to succeed.
Day-of-Procedure Instructions
On the day of your heart catheter balloon procedure, you’ll get specific instructions. These might include fasting, what to wear, and how to get to the hospital. You’ll also be told who should drive you home after.
Following these instructions is vital for a safe and smooth experience. If you have questions or concerns, always ask your healthcare provider.
By following the pre-procedure instructions and guidelines, you can help make your cardiac balloon procedure a success. This will also help you recover smoothly.
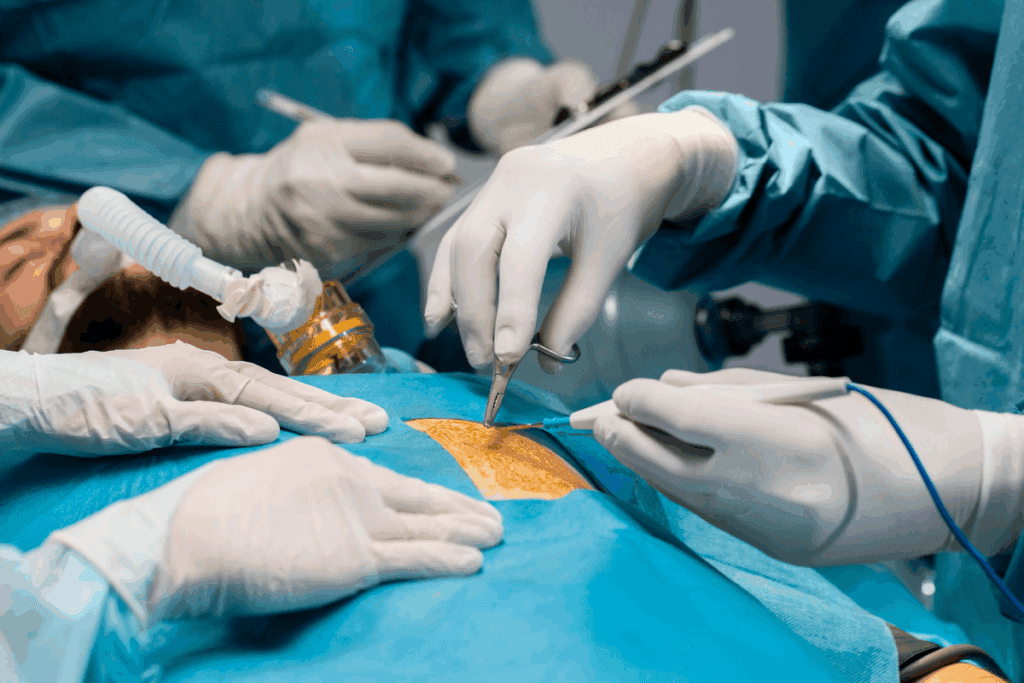
Step-by-Step: How the Cardiac Balloon Procedure Works
The cardiac balloon procedure is a detailed process to open blocked heart arteries. We’ll guide you through each step, from start to finish. This will help you know what to expect.
Catheter Insertion and Navigation
The first step is inserting a catheter into the blocked artery. We use a local anesthetic to numb the area where the catheter goes in, usually in the groin or arm. Then, the catheter is guided through the blood vessels to the blocked coronary artery using advanced imaging.
According to the American College of Cardiology, the procedure involves guiding a catheter through a blood vessel to the affected area. This precise navigation is key for the procedure’s success.
Balloon Inflation Technique
With the catheter in place, a balloon angioplasty is done. The balloon is placed at the blockage and inflated to clear the plaque, widening the artery. This inflation lasts a few seconds to a minute, and the balloon may be inflated and deflated several times to ensure the artery is fully open.
Stent Placement Process
After the balloon angioplasty, a stent is placed to keep the artery open. The stent is a small, mesh-like tube that is deployed at the site of the blockage. It stays in the artery permanently, helping to keep blood flowing and preventing the artery from narrowing again.
We use the latest stent technology for the best patient outcomes. The stent placement is a vital part of the cardiac balloon procedure. It offers long-term benefits for those with coronary artery disease.
Recovery and Aftercare Following Angioplasty
After a cardiac balloon procedure, patients start a critical recovery phase. This phase needs careful watching and following specific rules. We know this time can feel both hopeful and scary. But with the right care and advice, patients can get through it well.
Immediate Post-Procedure Care
Right after angioplasty, we watch patients closely for any problems or reactions. We check the site where the catheter was put for bleeding or swelling. We also keep an eye on their vital signs. Patients usually stay under watch for a few hours to make sure they’re okay.
Key aspects of immediate care include:
- Monitoring for bleeding or hematoma at the catheter insertion site
- Observing for signs of allergic reactions or complications
- Managing pain or discomfort
- Ensuring the patient is stable before discharge
Hospital Discharge Guidelines
Before leaving the hospital, patients get clear instructions for home care. We stress the importance of following these to avoid problems and ensure a smooth recovery. This includes how to take medications, care for the site, and what activities to avoid or do.
Discharge instructions typically cover:
- Medication regimen and possible side effects
- Care for the catheter insertion site
- Activity levels and restrictions
- Follow-up appointment scheduling
Long-term Recovery Timeline
Recovery time varies, but most people can get back to normal in a few days to a week. We tell patients to slowly start doing more and listen to their body. Rest when needed.
| Recovery Stage | Timeline | Activities |
| Immediate Recovery | 0-24 hours | Rest, monitor for complications |
| Early Recovery | 1-3 days | Gradually increase activity, follow medication regimen |
| Advanced Recovery | 1-2 weeks | Resume most normal activities, attend follow-up appointments |
Going to follow-up appointments is key to checking how well the angioplasty worked and to talk about any worries.
By following your healthcare team’s advice, you can have a good recovery and enjoy the benefits of the cardiac balloon procedure. We’re here to support you, giving the care and guidance you need for the best health.
Benefits and Limitations of the Cardiac Balloon Procedure
The cardiac balloon procedure is a key treatment for coronary artery disease. It’s known as balloon angioplasty. This method is popular because it’s minimally invasive and has a quick recovery time.
Advantages Over Traditional Surgery
The cardiac balloon procedure has many benefits over traditional surgery. Minimal invasiveness is a big plus. It only needs a small incision, usually in the groin or arm. This lowers the risk of complications and speeds up healing.
Another big plus is the quick recovery time. Most people can get back to normal in just a few days to a week. This is much faster than the recovery time for traditional surgery.
Potential Risks and Complications
Even though it’s generally safe, the cardiac balloon procedure has some risks. The NIH says angioplasty is mostly safe but can cause bleeding, infection, and damage to blood vessels.
Some patients might face restenosis, or the arteries getting narrow again. But, drug-eluting stents have made this problem much less common.
Long-term Effectiveness and Outcomes
The long-term success of the cardiac balloon procedure varies. Studies show it can greatly improve symptoms and quality of life for many with coronary artery disease.
But, it’s important to remember that it doesn’t cure coronary artery disease. Patients must keep managing their condition through lifestyle changes and, if needed, more treatments.
In summary, the cardiac balloon procedure is a valuable option for many with coronary artery disease. It offers a good mix of effectiveness and safety.
Alternative Treatments to Balloon Angioplasty
There are many ways to treat coronary artery disease, not just balloon angioplasty. Some patients might not be good candidates for this procedure. Others might choose other treatments instead.
Medication-Based Approaches
For some, taking medicine can be a good alternative. These drugs can help control symptoms, slow the disease, and lower heart attack risk.
- Antiplatelet agents: Medications like aspirin and clopidogrel prevent blood clots.
- Beta-blockers: These drugs make the heart work less and need less oxygen.
- Statins: Statins lower cholesterol, which slows artery plaque buildup.
- Nitrates: Nitrates improve blood flow to the heart, easing chest pain.
The American Heart Association says, “medicines can manage symptoms and slow disease progression.”
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses blocked arteries with grafts. These grafts usually come from the leg or chest. It’s often chosen for complex or multiple blockages.
The surgery involves:
- Getting a graft vessel from another body part.
- Attaching one graft end to the aorta and the other to the blocked artery.
- By-passing the blockage, restoring blood flow to the heart.
Newer Minimally Invasive Techniques
New, less invasive methods are being explored for treating coronary artery disease. These include:
- Rotational atherectomy: A method that uses a rotating burr to clear plaque.
- Laser angioplasty: Uses laser energy to remove plaque.
- Specialized stents: Drug-eluting stents and other advanced stent technologies.
These new techniques offer hope for those not suited for traditional balloon angioplasty or CABG.
Conclusion
We’ve looked into the cardiac balloon procedure, a key treatment for coronary artery disease. This method, also known as balloon angioplasty or heart balloon procedure, has changed how we treat blocked arteries.
In this article, we covered the cardiac balloon procedure’s history, when it’s used, and the tools and steps involved. We also talked about its advantages and downsides, plus other treatment options.
Choosing the cardiac balloon procedure is a big step towards better heart health. We suggest talking to a healthcare provider to find the best treatment for you.
FAQ
What is a cardiac balloon procedure?
A cardiac balloon procedure, also known as balloon angioplasty, is a minimally invasive treatment. It’s used to widen narrowed or blocked coronary arteries. We use a balloon catheter to push plaque against the artery walls, improving blood flow to the heart.
What is the purpose of a balloon catheter in angioplasty?
The balloon catheter is key in angioplasty. It’s used to widen narrowed or blocked arteries, improving blood flow. The balloon is inflated to push the plaque, then deflated and removed. Often, a stent is left to keep the artery open.
How is a cardiac balloon procedure performed?
To perform the procedure, we insert a catheter through an artery in the leg or arm. It’s guided to the affected coronary artery. The balloon is then inflated to widen the artery, and a stent may be placed. The whole process is done under local anesthesia and mild sedation.
What are the benefits of a cardiac balloon procedure?
The benefits include better blood flow to the heart and reduced angina symptoms. It also lowers the risk of heart attack. Plus, it’s less invasive than traditional surgery, leading to quicker recovery.
What are the possible risks and complications of a cardiac balloon procedure?
While safe, the procedure can have risks like bleeding and infection. There’s also a chance of artery or tissue damage. Though rare, stent thrombosis or restenosis can occur, thanks to modern stent technology.
How long does it take to recover from a cardiac balloon procedure?
Recovery time varies, but most can get back to normal in a few days to a week. We monitor patients for hours after and may keep them in the hospital briefly. Full recovery and return to strenuous activities can take several weeks.
What is the role of stent technology in cardiac balloon procedures?
Stent technology is vital in keeping the artery open after the procedure. We use stents to prevent restenosis and improve outcomes. Modern stents are designed to be more durable and less prone to thrombosis.
Are there alternative treatments to balloon angioplasty?
Yes, alternatives include medication, coronary artery bypass grafting (CABG), and newer techniques. The choice depends on the patient’s condition and overall health.
Can I undergo a cardiac balloon procedure if I have other health conditions?
Suitability depends on the condition’s severity and its impact on health. We evaluate each patient individually, considering their risk profile and medical history.
How effective is a cardiac balloon procedure in treating coronary artery disease?
It’s an effective treatment for coronary artery disease, improving blood flow and symptoms. Long-term success depends on other health conditions and lifestyle choices.
References
Neumann, F. J., Sousa-Uva, M., Ahlsson, A., Alfonso, F., Banning, A. P., Benedetto, U., Byrne, R. A., Collet, J. P., Falk, V., Head, S. J., Jüni, P., Kastrati, A., Koller, A., Kristensen, S. D., Niebauer, J., Richter, D. J., Seferovic, P. M., Sibbing, D., Stefanini, G. G., … ESC Scientific Document Group. (2019). 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal, 40(2), 87–165.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6342407/



































