
Millions of people use heart stents to keep their arteries open. But, a stent can get blocked, or restenosis, when the artery narrows again. This blocks blood flow to the heart. Find out what happens if a heart stent is blocked, causes, symptoms, and next steps.
This can happen months or years after the stent is put in. It’s more likely if you have atherosclerosis and don’t manage it well. At Liv Hospital, we focus on patient trust and safety. We offer top-notch care and proven solutions for each patient.
It’s key to know why stents fail, the signs, and what to do next. This helps keep your heart healthy and avoids emergencies. We’ll show you how to spot the warning signs and what steps to take.
Key Takeaways
- Blocked stents can occur months or years after the initial procedure.
- Atherosclerosis is a major risk factor for stent blockage.
- Recognizing the warning signs of stent blockage is critical for heart health.
- Liv Hospital provides internationally accredited care for patients with blocked stents.
- Understanding the causes and symptoms of stent blockage can help prevent emergencies.
Understanding Heart Stents and Their Function
Heart stents are small, mesh-like tubes that keep coronary arteries open. They have changed how we treat heart disease, making it less invasive than surgery.
What Is a Heart Stent?
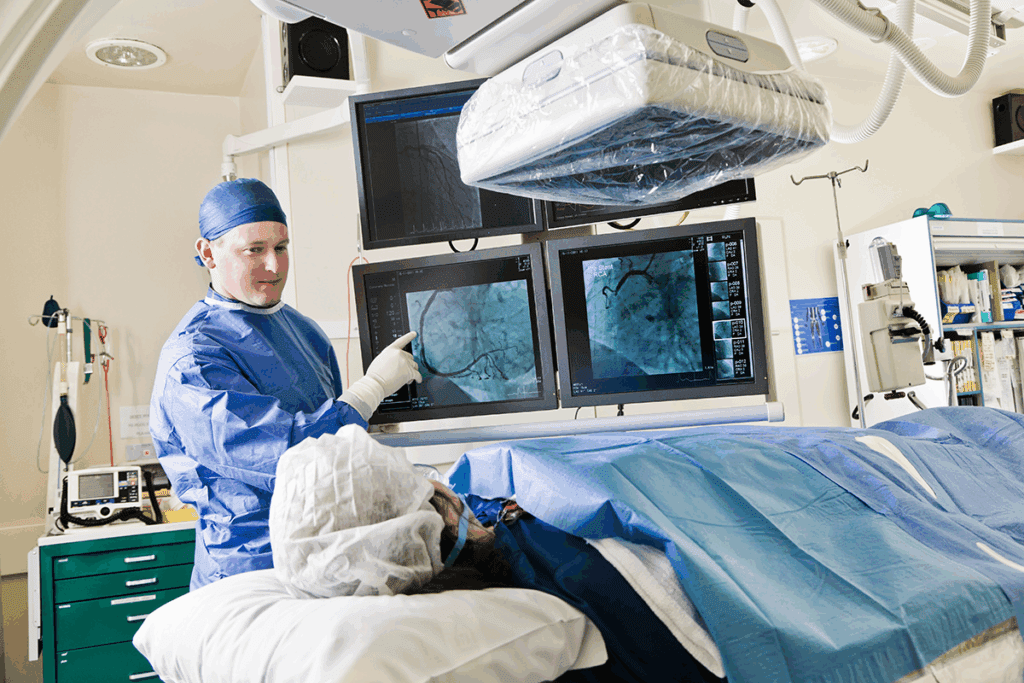
A heart stent is a tiny, metal mesh tube. It’s placed in a narrowed or blocked artery to improve blood flow. This is done during angioplasty, where a balloon first widens the artery.
How Stents Work to Improve Blood Flow
Stents keep the artery open, improving blood flow. They expand to fit the artery walls, preventing narrowing. A balloon is used to deploy the stent.
Stent placement involves several steps:
- Accessing the blocked artery through a small incision in the groin or arm.
- Using a catheter to guide the stent to the blocked area.
- Deploying the stent using a balloon to expand it.
- Ensuring the stent is properly positioned and expanded.
Types of Cardiac Stents and Their Effectiveness
There are several types of cardiac stents, each with its own benefits. The most common include:
- Bare-metal stents: The original stents, made of stainless steel or other metals. They are effective but may cause tissue growth.
- Drug-eluting stents: Coated with medication to prevent artery narrowing. They are the preferred choice due to their effectiveness.
- Bioresorbable stents: These stents dissolve over time, potentially reducing complications. They are being studied in clinical trials.
Knowing about the different stents and their effectiveness is key for patients and doctors. While stents work well, sometimes they may not stay open. This raises questions about whether they can be removed or replaced. The decision to replace a stent depends on several factors, including why it failed and the patient’s health.
What Happens If a Heart Stent Is Blocked?

Knowing what happens when a heart stent gets blocked is key to keeping your heart healthy. A heart stent is a small, mesh-like device that helps blood flow to the heart. But sometimes, it can get blocked, leading to stent restenosis or stent thrombosis. We’ll look at how stent restenosis happens, how long it takes, and the risks involved.
The Process of Stent Restenosis
Stent restenosis is when the artery narrows again after a stent is put in. This happens because the body reacts to the stent, growing new tissue that can block it. It’s a complex process involving inflammation and the growth of smooth muscle cells.
Key factors contributing to stent restenosis include:
- Injury to the artery wall during stent placement
- Inflammation caused by the stent
- Proliferation and migration of smooth muscle cells
- Neointimal hyperplasia, or the excessive growth of new tissue
Timeframe for Stent Blockage Development
Restenosis can happen at any time after a stent is placed. It usually occurs 3 to 6 months later, but it can happen years after. The exact time depends on the stent type, the patient’s health, and how well they follow their medication.
It’s important for patients to follow their post-procedure care and go to follow-up appointments to check on their stent.
Prevalence and Risk Statistics
The chance of stent restenosis varies based on the stent type and patient health. Drug-eluting stents, which release medication to prevent cell growth, have a lower rate of restenosis than bare-metal stents.
Research shows that drug-eluting stents have a restenosis rate of 5-10%, while bare-metal stents have a rate of 20-30%.
| Stent Type | Restenosis Rate |
| Drug-Eluting Stents | 5-10% |
| Bare-Metal Stents | 20-30% |
Understanding the risks and how stent blockage happens is key to managing and preventing it. By knowing the signs and taking steps to prevent it, patients can lower their risk of complications.
Common Causes of Stent Blockage
After a stent is placed, several biological and mechanical processes can contribute to its blockage. It’s important to understand these factors to manage and prevent complications.
Atherosclerosis Progression
Atherosclerosis is the buildup of fatty deposits and cholesterol inside your arteries. Even with a stent, atherosclerosis can continue to progress. This can lead to the stented area narrowing again. Factors like high blood pressure, high cholesterol, and smoking can influence this process.
Stent Thrombosis: Blood Clots Within Stents
Stent thrombosis is when a blood clot forms inside the stent. This is a serious complication that can cause a heart attack. The risk is highest in the first few months but can happen at any time. Factors that increase the risk include stopping antiplatelet therapy too soon, drug resistance, and certain medical conditions.
Neointimal Hyperplasia: Tissue Growth Around Stents
Neointimal hyperplasia is the growth of tissue around the stent, causing it to narrow. This is the body’s natural response to the stent. While drug-eluting stents have reduced this, it’s a possible cause of blockage.
Mechanical Factors Affecting Stent Performance
Mechanical factors can also affect stent blockage. For example, a stent can collapse or become dislodged, leading to blockage or complications. The stent’s design and deployment technique also play a role. It’s rare, but stents can collapse or move, impacting their effectiveness.
Understanding these causes of stent blockage is key for both patients and healthcare providers. Recognizing the factors that can lead to stent failure helps us take steps to minimize risks. This ensures the best outcomes for those with heart stents.
Risk Factors for Developing Blocked Stents
Knowing what can cause blocked stents is key to managing and preventing them. Certain health conditions, lifestyle choices, and how well you follow your medication can all play a part. These factors can greatly affect the chance of a stent getting blocked.
Medical Conditions That Increase Risk
Some health issues can make stents more likely to get blocked. For example, diabetes can slow down healing and raise the risk of restenosis. Studies show that people with diabetes are more at risk because of insulin resistance and inflammation
Chronic kidney disease also makes stent placement harder and raises the risk of blockage. The link between kidney health and heart health means patients with kidney disease need extra care and monitoring.
“Patients with diabetes or chronic kidney disease require closer surveillance for possible stent problems.”
Lifestyle Factors Contributing to Stent Failure
Our lifestyle choices also affect the risk of stent blockage. Smoking, for instance, is a big risk factor that can make atherosclerosis worse and increase stent failure chances. Eating too much saturated fat and cholesterol can also lead to new blockages.
- Stopping smoking is key to lowering stent blockage risk.
- Eating more fruits, vegetables, and whole grains is good for your heart.
- Staying active helps keep your blood vessels healthy.
Medication Non-Compliance Issues
Following your medication is very important to prevent stent blockage. Antiplatelet therapy is a must after a stent to stop blood clots. Not taking your antiplatelet meds can lead to stent thrombosis, a serious condition.
It’s important for patients to know how vital their meds are. They should talk to their doctors about any problems they have with their medication.
By understanding these risk factors, doctors can create better plans to lower the chance of stent blockage. This can lead to better health outcomes for patients.
Recognizing Symptoms of a Blocked Stent
It’s important to know the signs of a blocked heart stent. This is because a blocked stent can lead to serious problems, like a heart attack. Knowing the warning signs helps you get medical help fast.
Chest Pain and Angina Patterns
Chest pain, or angina, is a key symptom of a blocked stent. This pain feels like pressure or tightness in the chest. It might spread to the arms, back, neck, jaw, or stomach.
The pain’s feel can change. It might feel like the pain you had before the stent, or it could be different. Remember, not all chest pain means a blocked stent. But, any new or changing pain should be checked by a doctor.
Shortness of Breath and Fatigue
People with a blocked stent might also feel short of breath or tired. This is because the heart isn’t getting enough blood. It makes it hard for the body to work right.
Shortness of breath is often worse when you’re active or lying down. Fatigue can be very strong, making it hard to do daily things and live well.
Other Warning Signs to Monitor
There are other signs that might mean a blocked stent. These include:
- Palpitations or irregular heartbeats
- Dizziness or lightheadedness
- Nausea or loss of appetite
- Cold sweats
- Pain or discomfort in the arms or legs
These symptoms can mean different things. But, if you have a heart stent, they mean you need to see a doctor right away.
When Symptoms Require Emergency Medical Care
If you have severe chest pain that lasts more than a few minutes, get help fast. Also, seek emergency care for symptoms like trouble breathing, severe dizziness, or losing consciousness. These could be signs of a heart attack or a serious blockage in the stent.
| Symptom | Description | Action |
| Chest Pain | Pressure or tightness in the chest, possibly radiating to other areas | Seek medical attention if new or changing |
| Shortness of Breath | Difficulty breathing, specially during activity or when lying down | Consult a doctor if persistent or severe |
| Fatigue | Unusual tiredness affecting daily activities | Discuss with a healthcare provider if impacting quality of life |
Knowing the signs of a blocked stent can help a lot. It ensures you get medical help quickly. If you’re worried about symptoms, talk to your doctor right away.
Potential Complications of Stent Blockage
When a heart stent gets blocked, serious problems can happen. These issues are big risks for heart health. We’ll look at these problems and what they mean for people with coronary stents.
Heart Attack Risk and Warning Signs
A blocked stent raises the chance of a heart attack. Warning signs include sudden chest pain, shortness of breath, and dizziness. It’s key to spot these signs fast for quick medical help.
Acute Stent Thrombosis Dangers
Acute stent thrombosis is a blood clot in the stent. It’s very dangerous and needs quick medical help to avoid serious heart damage.
Long-term Cardiac Damage and Implications
Stent blockages or failures can harm the heart over time. This might lead to heart failure. Proper management and follow-up care are key to avoid these risks.
It’s important for heart stent patients to know about these risks. By watching for warning signs and getting the right care, people can lower their risk of serious heart problems.
Can Stents Be Removed or Replaced?
Patients often wonder if a heart stent can be removed or replaced when it fails. The answer is not simple. It depends on the stent type and why it failed.
Why Heart Stents Cannot Be Surgically Removed
Heart stents are meant to stay in the body forever. Unlike some other medical devices, stents are not typically removed surgically because they become part of the artery wall. The body covers the stent with its own cells, making removal risky and often unnecessary.
Removing a stent could damage the artery badly. This could lead to serious problems. So, doctors usually choose other treatments for a blocked or failed stent.
Options for Treating Failed Stents
Even though stents can’t be removed, there are ways to treat failed stents. These include:
- Repeat angioplasty and stenting
- Medication to manage symptoms and prevent further blockage
- Bypass surgery in some cases
Doctors choose the best option based on the patient’s condition and the stent failure details.
The Process of Stent Replacement
Often, a new stent can be put inside the old one. This is called in-stent stenting or nested stenting. This method can improve blood flow without removing the original stent. The decision to use a new stent depends on the patient’s health and the artery’s condition.
Mechanical Issues: Can Stents Collapse or Move?
Stents can rarely have mechanical problems. These include collapsing or moving from where they were placed. These issues are more common with certain stent types and can be affected by the patient’s anatomy.
Thanks to new stent technology, these problems are much less common. This makes stents a safer and more effective treatment for heart disease.
In summary, while stents can’t be removed surgically, there are many ways to manage failed stents. Knowing these options is key for both patients and doctors to make the best care choices.
Diagnosing a Blocked Heart Stent
Diagnosing a blocked heart stent is a detailed process. It starts with initial checks, imaging tests, and lab work. When symptoms suggest a blocked stent, doctors use a specific method to confirm it and find the right treatment.
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check-up. We look at symptoms like chest pain or trouble breathing. We also check the patient’s heart health.
This initial check helps us spot signs of a blocked stent. It guides us to more tests to confirm the diagnosis.
During the physical exam, we search for signs of heart problems. These can be abnormal heart sounds or fluid buildup. They show if the heart is under stress.
Imaging Tests and Procedures
Imaging tests are key in finding blocked stents. Some tests used are:
- Coronary Angiography: This is the top test for stent blockage. It uses dye to see the stent and check if it’s open.
- Stress Testing: This test checks how the heart works under stress. It uses exercise or medicine to increase heart rate.
- Coronary CT Angiography: This non-invasive test uses CT scans to see the coronary arteries and check the stent.
Laboratory Tests and Biomarkers
Laboratory tests are also vital in diagnosing and managing blocked stents. Key tests include:
- Cardiac Biomarkers: Tests for troponin and other enzymes show if the heart is damaged or under stress.
- Lipid Profile: This test checks cholesterol levels and other lipids. It helps see if atherosclerosis is getting worse.
- Blood Glucose and HbA1c: These tests are important for managing diabetes. It’s a risk factor for stent blockage.
By combining these diagnostic tests, we can accurately find a blocked heart stent. Then, we can plan an effective treatment.
Treatment Options for Blocked Stents
There are many ways to treat blocked stents, from medicines to surgery. The right treatment depends on how bad the blockage is, the patient’s health, and the stent’s type.
Medication Approaches and Antiplatelet Therapy
Medicine is key in treating blocked stents. Doctors often use antiplatelet therapy to stop blood clots. This usually includes aspirin and P2Y12 inhibitors like clopidogrel. How long you take these medicines depends on the stent and your health risks.
Key Medications for Stent Management:
- Aspirin
- P2Y12 inhibitors (e.g., clopidogrel, ticagrelor)
- Other antiplatelet agents
Repeat Angioplasty and Stenting Procedures
If a stent gets blocked again, you might need more angioplasty and stenting. This method uses a balloon to open the blockage and might include a new stent.
“The use of drug-coated balloons and stents has improved outcomes in patients with stent restenosis,” according to recent clinical guidelines.
Here’s a look at different ways to treat blocked stents:
| Treatment Approach | Success Rate | Complications |
| Medication Only | Moderate | Bleeding risks |
| Repeat Angioplasty/Stenting | High | Restenosis, thrombosis |
| Bypass Surgery | High | Surgical risks, recovery time |
Bypass Surgery Considerations
For complex blockages or when stents fail, CABG might be suggested. CABG is a surgery that bypasses the blocked artery with a graft.
Emerging Treatment Technologies
New technologies like bioabsorbable stents and drug delivery systems are being studied. These aim to better outcomes and cut down on repeat procedures.
As cardiology advances, treating blocked stents will get better. We’ll see more effective and less invasive options for patients.
Conclusion: Living Well with Heart Stents
Living with heart stents means taking care of your heart in many ways. Knowing the signs of a blocked stent is key. If a stent gets blocked, it can lead to serious problems, like a heart attack.
To avoid stent blockage, follow your doctor’s advice on medicine and lifestyle changes. Regular check-ups with your doctor are also important. This helps keep your stent working right and your heart healthy. With these steps, people with heart stents can lower their risk of problems and live better.
We stress the need for a full care plan. This includes eating well, exercising often, and managing stress. By being proactive in their care, patients with heart stents can handle the challenges of managing their stents. They can keep their heart in top shape.
FAQ
What happens if a heart stent is blocked?
A blocked heart stent can cut down blood flow to the heart. This might cause chest pain, shortness of breath, or even a heart attack. We’ll look at why this happens, the signs, and how to treat it.
Can stents be removed and replaced?
Stents can’t be taken out by surgery, but we can fix them with more procedures if they block or fail. We’ll talk about how to treat failed stents, like using more stents or surgery.
What are the symptoms of a blocked stent?
Symptoms of a blocked stent include chest pain, shortness of breath, and feeling tired. It’s key to know these signs and get help right away if you notice them.
Can a stent be removed?
No, heart stents can’t be removed by surgery. Once in, they stay there forever. But, we can fix blocked or failed stents with more treatments.
What causes stent blockage?
Stent blockage can come from atherosclerosis, stent thrombosis, or other issues. Knowing why it happens helps us prevent or manage it.
Can stents collapse or move?
Stents rarely collapse or move, but it can happen. We’ll look at why this might happen and how we fix it.
How is stent blockage diagnosed?
To find out if a stent is blocked, we use tests like imaging and lab work. These help us see if and how bad the blockage is.
What are the treatment options for blocked stents?
For blocked stents, we can use medicine, more stenting, surgery, or new tech. We’ll go over these options to find the best way to treat blocked stents.
Can heart stents be replaced?
Even though stents can’t be removed, we can do more procedures to fix them. This includes putting in new stents or other methods to get blood flowing again.
How can I prevent stent blockage?
To stop stent blockage, manage risks, follow your meds, and live a healthy lifestyle. We’ll share tips to keep your stent healthy and avoid blockage.
References
- Siontis, G. C. M., et al. (2023). Restenosis of stented coronary arteries. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK545139/





