Jaundice or unexplained abdominal pain can be scary.bowel duct stentWhat are the bowel changes with ovarian cancer? It often means there’s a blockage in the bile duct. At Liv Hospital, we use the latest stent methods and focus on the patient to treat these blockages well.
Bile duct blockages can come from stones, strictures, or tumors. Our team works hard to get bile flowing again and stop jaundice. With a success rate over 90 percent, stent insertion is a safe and effective way to boost liver health.
Key Takeaways
- Bile duct blockages can be caused by stones, strictures, or tumors.
- Stent insertion is a minimally invasive procedure with a high success rate.
- Restoring bile flow can prevent jaundice and improve liver function.
- Liv Hospital uses advanced stent techniques and a patient-centered approach.
- A patient-centered approach ensures complete care and support.
Understanding the Bile Duct System
The bile ducts are a network of tubes that help move bile from the liver to the small intestine. This is key for digestion, as bile breaks down fats into smaller bits for the body to absorb.
The Function of Bile Ducts in Digestive Health
Bile ducts are vital for moving bile from the liver to the gallbladder and then to the small intestine. A well-working bile duct system is key for good digestion and nutrient absorption. Without it, the body might have trouble digesting fats, causing digestive problems.
The bile duct system ensures bile reaches the right place at the right time. It uses a complex network of ducts that merge into the common bile duct. This duct then empties into the small intestine. The role of bile in digestion shows how complex and specialized human anatomy is.
Common Causes of Bile Duct Obstructions
Bile duct obstructions can happen for many reasons, like gallstones, tumors, and strictures. Gallstones are a common cause, as they can move from the gallbladder into the bile ducts, blocking them. Tumors, both benign and malignant, can also block the bile ducts by physically stopping bile flow. Research on trusted medical resources shows understanding these causes is key for the right treatment, like using a bile duct stent or liver stents to fix the flow.
Other reasons for bile duct obstructions include inflammatory conditions and infections that cause scarring and narrowing. Sometimes, surgery or injuries during medical procedures can also damage or block the bile ducts. Knowing these causes is the first step to managing and treating them, which might involve stents in bile duct to clear blockages.
Recognizing Symptoms of Bile Duct Blockage

Spotting bile duct blockage symptoms early can greatly help treatment. A blockage happens when bile can’t flow from the liver to the intestine. This can cause mild issues or serious problems.
Early Warning Signs
The first signs of bile duct blockage are often subtle but important. Look out for:
- Mild jaundice, which makes skin and eyes yellow
- Urine that’s darker than usual
- Stools that are pale or clay-colored
- Mild pain or discomfort in the upper right belly
These signs happen because bile can’t move into the intestine. This causes bilirubin to build up in the blood and tissues.
Advanced Symptoms Requiring Immediate Attention
Ignoring these symptoms can lead to more serious issues. Look out for:
- Severe abdominal pain
- High fever and chills, which can mean an infection
- Jaundice that gets worse
- Itching (pruritus) from bile salts in the skin
Seeing a doctor right away is key to avoid bigger problems. They might put in a stent for bile duct to fix the flow.
A stent in liver or bile duct helps with blockages. Knowing why a stent is needed helps patients understand its importance.
| Symptom | Description | Possible Complication |
| Mild Jaundice | Yellowing of skin and eyes | Liver dysfunction |
| Dark Urine | Urine becomes darker | Bilirubin buildup |
| Pale Stools | Stools become pale or clay-colored | Bile flow obstruction |
| Severe Abdominal Pain | Intensified pain in the upper right abdomen | Cholangitis or pancreatitis |
Using a bile stent is a common and effective treatment. Knowing the symptoms and getting help quickly can greatly improve a patient’s life.
Diagnostic Procedures for Detecting Blockages
Diagnosing bile duct blockages involves several steps. First, blood tests and then advanced imaging methods are used. These steps are key to finding the cause and the right treatment.
Initial Blood Tests and Liver Function Assessment
The first step is blood tests to check liver function. These tests look at enzymes and substances in the blood. For example, they check bilirubin, alkaline phosphatase, and liver enzymes. High levels can show bile duct blockage or liver problems.
A leading gastroenterologist says, “Liver function tests are key in spotting bile duct obstructions and guiding further tests.”
Blood tests can reveal:
- Elevated bilirubin levels, indicating jaundice
- Increased alkaline phosphatase, suggesting bile duct obstruction
- Abnormal liver enzymes, pointing to liver damage or disease
Imaging Techniques
After blood tests, imaging is used to see the bile ducts. It helps find where and why the blockage is. Common methods include:
Ultrasound: Often the first test, it spots bile duct dilation and gallstones.
Computed Tomography (CT) Scan: Gives detailed images of the bile ducts and nearby areas.
Magnetic Resonance Cholangiopancreatography (MRCP): A special MRI that shows the bile and pancreatic ducts clearly.
“Imaging like MRCP has changed how we diagnose bile duct issues,” says a top expert. “It lets us see exactly what’s going on and plan treatments like stenting.”
These tests are vital for finding bile duct blockages. They help decide the best treatment, which might include a stent in liver duct to fix the flow of bile.
What is a Bowel Duct Stent?
Learning about bowel duct stents can help patients understand their treatment options. A bowel duct stent, also known as a bile duct stent, is a small, mesh tube. It keeps the bile duct open, ensuring bile flows into the intestine properly.
Definition and Purpose of Bile Duct Stents
Bile duct stents are used to relieve obstructions in the bile duct. Their main goal is to restore bile flow, which is key for digestion. By keeping the bile duct open, stents prevent bile buildup in the liver, lowering infection risks.
“The placement of a bile duct stent is a minimally invasive procedure that can significantly improve a patient’s quality of life,” says Medical Expert, a gastroenterologist. “It’s a highly effective way to manage both benign and malignant bile duct obstructions.”
How Stents Restore Normal Bile Flow
Bile duct stents physically hold open the obstructed bile duct area. This lets bile flow freely from the liver into the intestine. It helps with digestion and reduces symptoms like jaundice and itching.
The procedure for placing a bile duct stent usually involves ERCP or PTBD. Both methods are effective, and the choice depends on the patient’s condition and the doctor’s advice.
Success Rates and Effectiveness
The success rates for bile duct stenting are generally high, with most patients feeling better right away. The stent’s effectiveness can vary based on the cause of the obstruction and the stent type used.
Research shows bile duct stenting improves patient outcomes, including symptom relief and quality of life. “Bile duct stenting has revolutionized the management of bile duct obstructions,” notes Medical Expert, a hepatologist. “It’s a testament to the advancements in gastroenterology and interventional radiology.”
In conclusion, bowel duct stents are a key treatment for bile duct obstructions. Understanding their role can help patients better navigate their treatment journey.
Types of Stents in Bile Duct
Choosing the right stent for bile duct blockages is key. The type of stent depends on the blockage, the patient’s health, and how long the stent will be needed.
Plastic Stents: Applications and Limitations
Plastic stents are often used for short-term needs. They are made from materials like polyethylene or Teflon. They are cheap and easy to remove but can clog easily.
Key characteristics of plastic stents:
- Ease of insertion and removal
- Lower cost compared to metal stents
- Higher risk of clogging
- Suitable for temporary drainage
Metal Stents: Covered vs. Uncovered
Metal stents are better for long-term use in cancer blockages. They are made from materials like stainless steel or nitinol. They last longer than plastic stents.
Covered metal stents have a coating to stop tumors from growing. Uncovered stents let tissue grow, helping them stay in place but risking blockage.
Biodegradable Options and Innovations
Biodegradable stents are new in bile duct stenting. They dissolve over time, which might cut down on the need for more procedures. They’re good for non-cancer blockages.
These stents aim to avoid problems like blockage and stent movement that come with long-term use.
| Stent Type | Advantages | Disadvantages |
| Plastic Stents | Low cost, easy to remove | Higher risk of clogging |
| Metal Stents (Covered) | Better patency rates, reduced tumor ingrowth | Higher cost, possible migration |
| Metal Stents (Uncovered) | Better anchoring, improved patency | Risk of tumor ingrowth |
| Biodegradable Stents | Reduces need for reintervention, minimizes long-term complications | Limited availability, variable degradation rates |
Reasons for Liver Stent Placement
It’s important for patients to know why they might need a liver stent. Liver stents help with many bile duct problems. They offer relief and better health outcomes.
Malignant Conditions Requiring Stenting
Cancers like pancreatic cancer and cholangiocarcinoma often lead to bile duct blockages. This causes jaundice and itching. A stent can help by keeping the bile duct open, easing these symptoms.
Cancer Research UK says stents are a key treatment for bile duct cancer. They help manage symptoms and improve life quality.
Stents are placed in the bile duct to ensure bile flows into the intestine. This reduces jaundice and itching. It also helps manage pain and improves nutrition.
Benign Conditions Requiring Stent in Liver
Stents are also used for benign conditions. Post-surgical leaks and strictures are common reasons. For example, after surgery, some patients might get bile duct strictures or leaks.
- Strictures: Narrowing of the bile duct that can impede bile flow.
- Leaks: Bile leaks that can occur post-surgery, requiring stenting to divert bile flow and allow healing.
Stenting is a less invasive option compared to surgery. It helps in faster recovery and lowers the risk of complications. Stents ensure bile flows normally, improving liver function and overall health.
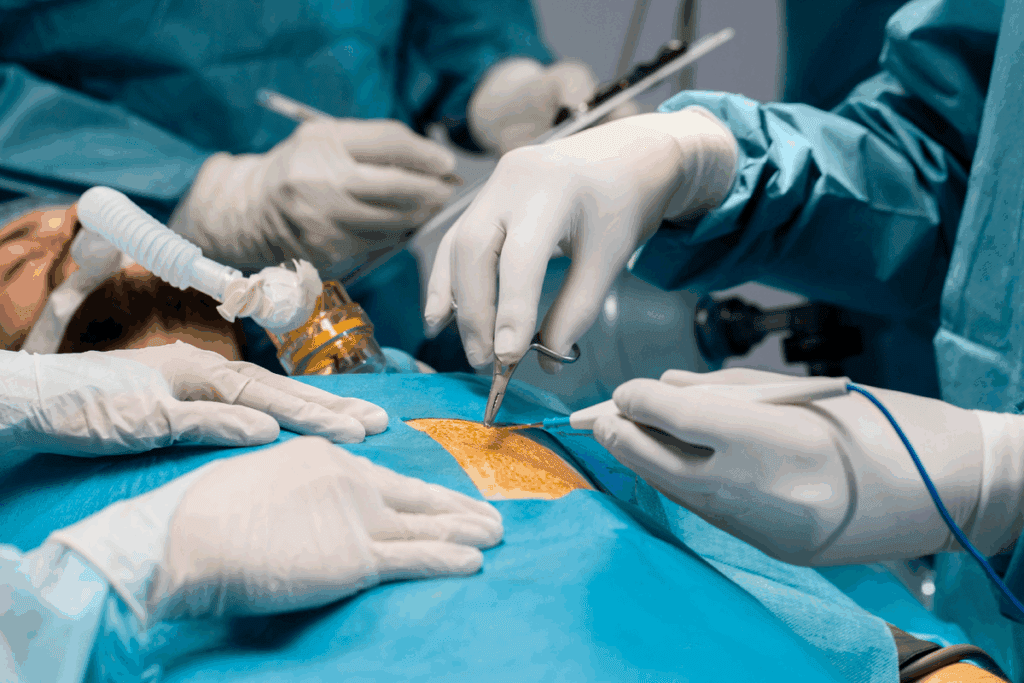
Stent in Bile Duct Placement Procedures
Effective bile duct stenting procedures are key for patient recovery. We use two main methods: Endoscopic Retrograde Cholangiopancreatography (ERCP) and Percutaneous Transhepatic Biliary Drainage (PTBD).
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a common method for placing stents in the bile duct. It uses a flexible tube with a camera and tools. This lets us see the bile duct and place the stent correctly. ERCP is chosen for its minimally invasive nature and success in restoring bile flow.
ERCP has the advantage of a quicker recovery and fewer complications than surgery. But, it needs special training and equipment. There are risks like pancreatitis or bleeding.
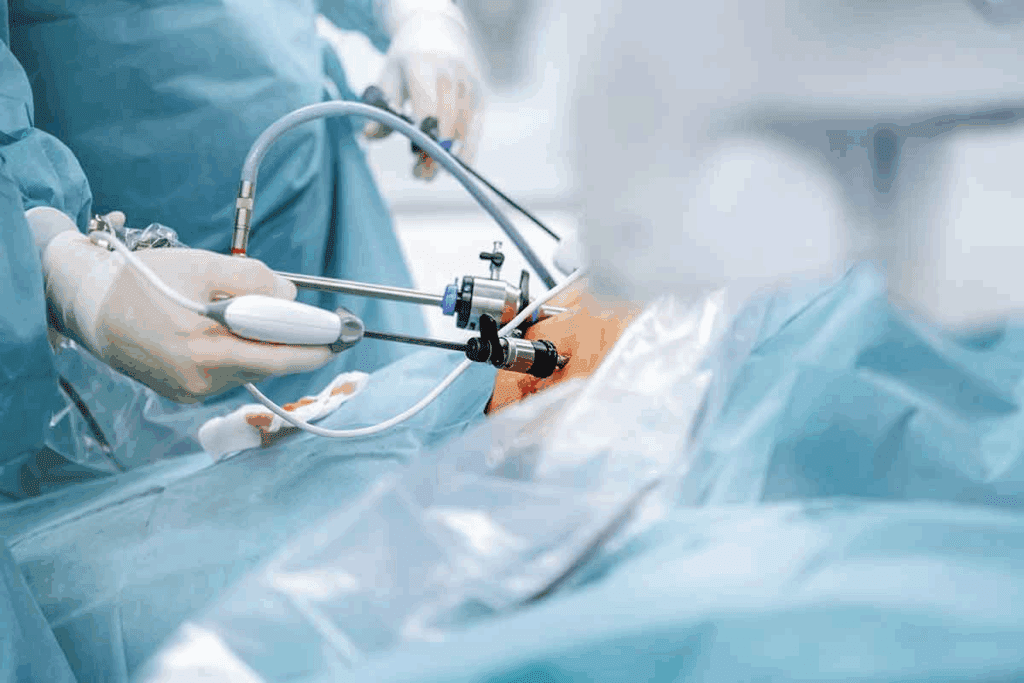
Percutaneous Transhepatic Biliary Drainage (PTBD)
PTBD is used when ERCP isn’t possible. It goes through the skin and liver to reach the bile duct. PTBD is great for complex bile duct obstructions.
PTBD is effective but has more risks, like infection and bleeding. So, we choose PTBD based on the patient’s condition and the benefits and risks.
Both ERCP and PTBD are important for managing bile duct obstructions. Knowing when to use each helps us give the best care to our patients.
Alternative Treatments Before Considering a Stent for Bile Duct
Looking into other treatments is key for those with bile duct blockage before opting for a stent. We’ll explore options that might ease symptoms and boost bile flow without needing a stent right away.
Medication Options for Bile Flow Improvement
Medicines can help improve bile flow and lessen blockage symptoms. These might include:
- Bile salts: to boost bile production and flow
- Ursodeoxycholic acid (UDCA): to dissolve certain gallstones and enhance bile duct function
- Cholestyramine: to bind bile acids and cut down on itching from cholestasis
These drugs can help manage symptoms and enhance life quality for those with bile duct blockage.
Surgical Alternatives to Stenting
For some, surgery might be a better choice than stenting for bile duct issues. Surgical options include:
- Biliary bypass surgery: to redirect bile flow around the blockage
- Gallbladder removal: when gallstones cause the blockage
- Removal of the obstructed bile duct segment: followed by reconstruction
These surgeries can offer lasting relief from bile duct blockage symptoms. They might be considered based on the blockage’s cause.
When Conservative Management Is Appropriate
For mild or early bile duct blockage, conservative management might be best. This usually means:
- Monitoring liver function tests: to gauge the blockage’s severity
- Dietary modifications: to manage symptoms and support liver health
- Regular follow-up appointments: to track the blockage’s progress and adjust treatment as needed
Conservative management can be a good first step. It allows for more aggressive treatments like stenting if symptoms get worse or the blockage advances.
Benefits of Stent in Liver Duct Treatment
Liver duct stenting is a key treatment for blocked bile ducts. It involves placing a stent, a small, mesh-like tube, in the bile duct. This keeps it open, allowing bile to flow into the intestine.
Immediate Symptom Relief
Stent placement in the liver duct quickly relieves symptoms of blocked bile ducts. Patients often see a drop in jaundice, itching, and abdominal pain soon after. A study in the Journal of Clinical Gastroenterology found that over 90% of patients felt better within the first week after the procedure.
“The use of stents in malignant bile duct obstruction has been shown to significantly improve patient outcomes by restoring bile flow and reducing symptoms.” – Medical Expert, Gastroenterologist
Improved Quality of Life Outcomes
Stent placement improves the quality of life for patients by restoring normal bile flow. This reduces symptoms and prevents complications like cholangitis and liver damage. A study in the Journal of Hepatology showed that patients with stents reported a big improvement in their quality of life.
Long-term Prognosis Improvements
Stent placement also improves long-term outcomes. For those with cancer, it can make life better during treatment. For benign conditions, it can prevent future blockages. A study found that patients with stents had better long-term results than those without.
| Benefits | Description | Outcome |
| Immediate Symptom Relief | Reduction in jaundice, itching, and abdominal pain | Improved patient comfort |
| Improved Quality of Life | Restoration of normal bile flow | Better overall well-being |
| Long-term Prognosis | Palliative care for malignant conditions; preventive measure for benign conditions | Enhanced survival quality and reduced complications |
In conclusion, stent placement in the liver duct offers many benefits. It provides quick relief from symptoms and improves long-term health. As medical technology advances, stenting will likely become even more important in treating bile duct obstructions worldwide.
Managing Complications of Stents in Liver
Stents in the liver can help patients with bile duct obstructions. But, they can also cause problems. It’s important to manage these issues well to keep patients safe.
Recognizing Blocked Bile Duct Stent Symptoms
A blocked bile duct stent can cause jaundice, itching, and changes in urine or stool color. Patients should watch for these signs and tell their doctor right away. Regular check-ups can catch problems early.
Symptoms of a blocked stent can be like those before the stent was placed. Spotting these signs early can stop bigger problems. We suggest patients keep a symptom journal to talk about with their doctor.
Addressing Stent Migration and Displacement
Stent migration or displacement is when the stent moves from its place. This can happen for many reasons. Symptoms include abdominal pain, fever, or jaundice.
If you think the stent has moved, you might need more tests like X-rays or CT scans. Sometimes, you’ll need more procedures to fix the stent.
Preventing and Treating Infections
Infections are a big risk with liver stents. Cholangitis, an infection of the bile duct, can be very serious. Keeping everything clean and sterile during stent placement is key to avoiding infections.
Watch for signs of infection like fever, chills, or belly pain. If you think you have an infection, antibiotics might be needed. Sometimes, you’ll need to stay in the hospital for treatment.
Understanding the risks of liver stents and how to handle them is important. Patients and doctors working together can make sure the best care is given. Regular check-ups and teaching patients are vital for managing complications.
Recovery and Aftercare Following Stenting in Bile Duct
Bile duct stenting is a big procedure, and aftercare is key for a smooth recovery. After the procedure, patients are watched closely to catch any immediate problems.
Immediate Post-Procedure Care Guidelines
Right after the procedure, we watch for any bad reactions or issues. We look for bleeding, infection, or stent problems. Patients usually stay for a few hours before going home.
Key aspects of immediate care include:
- Monitoring vital signs and overall condition
- Managing pain and discomfort
- Observing for signs of complications
Dietary Modifications and Restrictions
Diet is very important after bile duct stenting. We suggest a diet that’s easy on the stomach to avoid problems.
Recommended dietary adjustments include:
- Eating smaller, more frequent meals
- Avoiding fatty or greasy foods
- Increasing intake of fluids
When to Contact Your Healthcare Provider
It’s important for patients to know when to call their doctor after going home. We tell patients to call if they have severe stomach pain, fever, or jaundice.
Signs that require immediate attention:
- Severe pain or discomfort
- Fever or chills
- Yellowing of the skin or eyes (jaundice)
- Dark urine or pale stools
By following these guidelines and knowing when to seek medical help, patients can have a better recovery after bile duct stenting. Regular check-ups with healthcare providers are also important to keep an eye on the stent and address any issues.
Conclusion
Treating bile duct blockages with a bowel duct stent or bile duct stent is very effective. It helps patients feel better and live better lives. This is true for both simple and serious conditions.
Liver stents have changed how we manage bile duct problems. They offer a simple way to fix blockages and get bile flowing right again.
We talked about how to spot bile duct blockage symptoms and how doctors find them. Putting in a stent can quickly make patients feel better. It also helps them live better and can even improve their chances of getting better in the long run.
If you think you might have a bile duct blockage, you should see a doctor right away. Thanks to new stent technology, like plastic, metal, and biodegradable ones, treatments can be more personalized. Knowing about bile duct stents helps both patients and doctors work together to get the best results.
FAQ
What is a bile duct stent and how does it work?
A bile duct stent is a small, mesh tube. It’s placed in the bile duct to help bile flow. This keeps the bile duct open, preventing blockages caused by stones or tumors.
What are the symptoms of a blocked bile duct?
Symptoms of a blocked bile duct include jaundice, dark urine, and pale stools. Severe abdominal pain, fever, and cholangitis are also signs. If you notice these, seek medical help right away.
How is a bile duct blockage diagnosed?
To diagnose a blockage, doctors start with blood tests to check liver function. Then, they use CT scans, MRI, and MRCP to see the bile ducts. This helps find the cause and location of the blockage.
What are the different types of stents used in bile duct stenting?
There are plastic, metal, and biodegradable stents for bile duct stenting. Each has its own use and benefits. The right stent depends on the patient’s condition.
What is the success rate of stent insertion in treating bile duct blockages?
Stent insertion is very successful, with over 90 percent success rate. It’s a minimally invasive procedure that improves liver function and relieves symptoms quickly.
What are the possible complications of stents in the liver?
Complications include blocked stents, migration, and infection. It’s important to watch for these symptoms and get medical help if they happen.
How is a stent placed in the bile duct?
Stents are placed through ERCP or PTBD. ERCP is a common endoscopic method. PTBD is used when ERCP is not possible.
What are the benefits of stent placement in the liver duct?
Stent placement relieves symptoms and improves quality of life. It can also help the long-term prognosis for both malignant and benign conditions.
What are the alternative treatments available before considering stent placement?
Before stent placement, treatments include medications and surgery. The best treatment depends on the patient’s condition and the cause of the blockage.
What are the aftercare guidelines following bile duct stenting?
After stenting, follow immediate care instructions and dietary changes. Also, watch for signs of complications. This ensures the stent works properly.
Can a stent in the bile duct migrate or become blocked?
Yes, stents can migrate or become blocked. These complications need quick medical attention. Regular check-ups can catch these issues early.
How do I know if my bile duct stent is blocked?
Symptoms of a blocked stent include jaundice, dark urine, pale stools, and pain. If you notice these, contact your healthcare provider right away.
References
- Centers for Disease Control and Prevention. (2023). Viral hepatitis and liver function testing. U.S. Department of Health and Human Services.https://www.cdc.gov/hepatitis/diagnosis.htm









