Last Updated on November 20, 2025 by Ugurkan Demir
Acute Lymphocytic Leukemia (ALL) is a serious and fast-growing blood cancer that affects both young people and adults, especially those over 50. At Liv Hospital, we focus on early diagnosis and rapid treatment to prevent severe outcomes and improve survival rates.
Understanding the complications of acute lymphocytic leukemia is essential for managing the disease effectively. Because cancer cells crowd the bone marrow, patients often develop anemia, low white blood cell counts, and increased infection risk. Other complications of acute lymphocytic leukemia can include bleeding, fatigue, and organ enlargement due to the spread of abnormal cells.
ALL accounts for about 2 percent of blood cancers in the U.S. and is more common in men than women, and in Caucasians compared to African Americans. At Liv Hospital, our team combines advanced treatments with compassionate care to help patients manage symptoms and reduce complications for a better quality of life.
Key Takeaways
- ALL is a rapidly progressing cancer requiring urgent attention to its complications.
- Complications can be life-threatening and are related to both the disease and treatments.
- Understanding and managing these complications is key for the best results.
- ALL incidence increases after age 50, affecting adults as well as children.
- Liv Hospital is known for its top-notch care in managing ALL and its complications.
Understanding Acute Lymphocytic Leukemia (ALL)
Acute Lymphocytic Leukemia (ALL) is a serious blood and bone marrow disease. It causes too many immature white blood cells. This is because of an overproduction in the bone marrow.
Definition and Pathophysiology
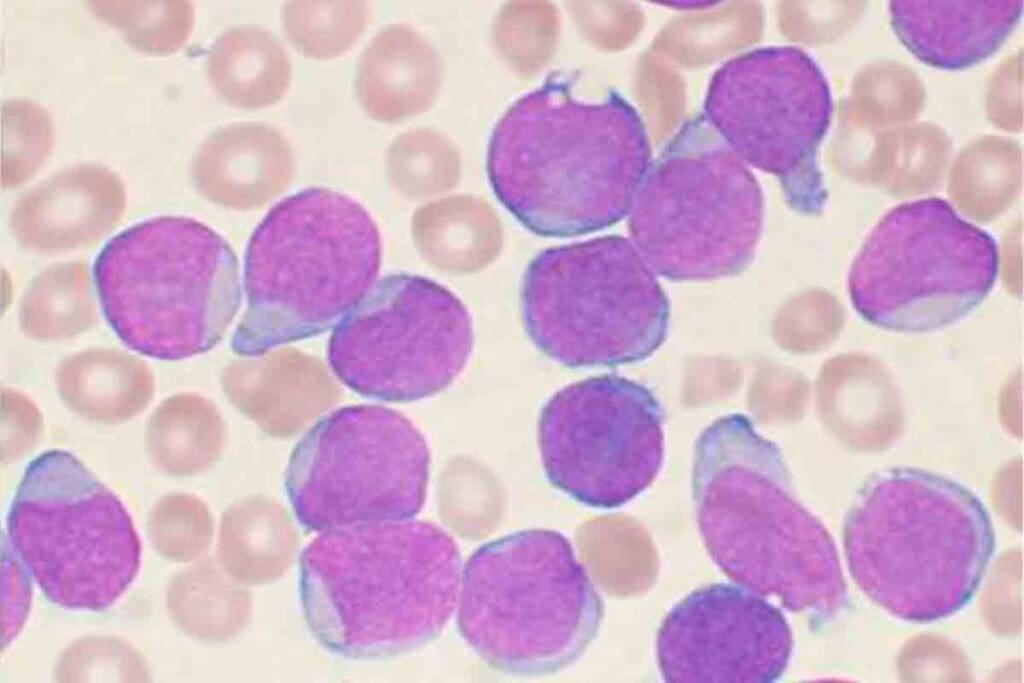
ALL is a cancer that makes too many immature white blood cells. These cells grow in the bone marrow. They push out normal cells, causing problems.
Genetic changes cause ALL. These changes let cells grow without control. They affect how cells work and grow.
A key sign of ALL is having too many immature cells in the blood and bone marrow.
Prevalence Across Age Groups
ALL is the top cancer in kids. It’s a big part of childhood cancers. But it also happens in adults, more in some age groups.
More kids get ALL between 2 and 5 years old. Adults over 50 also see a rise in cases.
“The age distribution of ALL highlights the need for age-specific diagnostic and treatment approaches.”
Risk Factors and Genetic Considerations
ALL comes from genes and the environment. Things like benzene and radiation increase the risk.
Studies found genes linked to ALL risk. These include ARD5B, IKZF1, and CDKN2A. These genes can affect how likely someone is to get ALL and how well they might do in treatment.
- Genetic predisposition plays a significant role in the development of ALL.
- Environmental exposures can also contribute to the risk of developing ALL.
How Complications Develop in ALL

To understand complications in Acute Lymphocytic Leukemia (ALL), we need to look at the disease itself and how treatments affect it. Knowing how complications arise is key to improving patient care.
Disease-Related Pathological Processes
ALL causes the bone marrow to fail, leading to anemia, low platelets, and low white blood cells. Anemia makes people feel tired, weak, and short of breath. This greatly affects their quality of life.
The disease harms the bone marrow and immune system. Leukemic cells fill the bone marrow, reducing normal blood cell production.
Treatment-Induced Complications
Chemotherapy and radiation therapy for ALL can cause serious side effects. Chemotherapy kills cancer cells but also harms healthy cells, leading to hair loss, mouth sores, and infections.
Radiation therapy can cause long-term problems like cancer, hormone issues, and brain problems. It’s used for certain cases, like treating the brain or preparing for a stem cell transplant.
Risk Stratification for Complications
Doctors assess various factors to predict complications in ALL. This helps tailor treatments to reduce risks and improve results.
| Risk Factor | Description | Potential Complication |
| Age | Patients under 1 year or over 10 years | Increased risk of treatment-related toxicity |
| White Blood Cell Count at Diagnosis | High WBC count (>100,000/µL) | Tumor lysis syndrome, organ dysfunction |
| Genetic Abnormalities | Presence of certain genetic mutations (e.g., MLL rearrangement) | Poor response to treatment, increased risk of relapse |
Understanding these risk factors helps doctors create better treatment plans. This approach aims to reduce complications and improve patient outcomes.
Complications of Acute Lymphocytic Leukemia: Overview and Classification
Acute Lymphocytic Leukemia (ALL) comes with many complications. These can be grouped by when they happen, how they affect the patient, and if they can be prevented. Knowing about these complications is key to good care and management.
Acute vs. Chronic Complications
ALL complications are split into acute and chronic types. Acute complications happen right after diagnosis or during the first treatment. They include severe infections, bleeding, and tumor lysis syndrome.
Chronic complications appear later, sometimes years after treatment. These can be secondary cancers, heart disease, and brain problems.
Life-Threatening vs. Quality-of-Life Impacting Complications
Complications of ALL can also be divided by how serious they are. Life-threatening complications can cause serious illness or death if not treated right away. Examples are severe infections, brain problems, and heart issues.
Quality-of-life impacting complications aren’t as deadly but can really affect a patient’s life. These include tiredness, poor nutrition, and mental health issues.
Preventable vs. Inevitable Complications
Complications can also be grouped by if they can be prevented. Preventable complications can be avoided with the right steps, like using antibiotics to stop infections.
Inevitable complications are part of the disease or its treatment. They can’t be completely stopped, but their effects can be lessened with early action.
Understanding the types of complications in ALL helps doctors plan better. They can work on preventing, catching early, and managing these issues. This leads to better results for patients.
Complication #1: Severe Anemia
Severe anemia is a common problem in Acute Lymphocytic Leukemia (ALL). It happens when leukemic cells fill the bone marrow. This stops normal blood cell production, causing anemia.
Pathophysiology and Clinical Presentation
In ALL, anemia is caused by leukemic cells taking over the bone marrow. This makes it hard for the body to make red blood cells. Patients often feel tired, weak, and pale. They might also have trouble breathing.
Key clinical features include:
- Fatigue and generalized weakness
- Pale skin and mucous membranes
- Shortness of breath and dizziness
- Tachycardia and heart failure in severe cases
Diagnostic Evaluation
To diagnose severe anemia in ALL, doctors do a lot of tests. They check the blood count, reticulocyte count, and look at red blood cells under a microscope.
Diagnostic tests for severe anemia include:
- Complete Blood Count (CBC)
- Reticulocyte count
- Peripheral blood smear
- Bone marrow aspiration and biopsy
Treatment Approaches: Transfusions and Erythropoiesis-Stimulating Agents
Treating severe anemia in ALL aims to fix the problem and ease symptoms. Doctors often give red blood cell transfusions to quickly boost red blood cell levels. They might also use erythropoiesis-stimulating agents to help make more red blood cells. But, this depends on the situation.
Treatment strategies include:
- Red blood cell transfusions to rapidly improve oxygen delivery
- Erythropoiesis-stimulating agents to enhance red blood cell production
- Addressing the underlying cause, such as treating the ALL
- Monitoring and managing possible anemia complications
Complication #2: Thrombocytopenia and Hemorrhagic Events
Thrombocytopenia and hemorrhagic events are big problems in Acute Lymphocytic Leukemia (ALL). They affect how well patients do and their quality of life. These issues come from the disease and its treatment, messing with platelet count and function.
Mechanisms of Platelet Dysfunction in ALL
In ALL, low platelets are mainly because of cancer cells in the bone marrow. This stops platelets from being made. Chemotherapy also hurts the bone marrow, making it harder to make platelets. The disease changes the bone marrow and makes bad platelets.
Clinical Manifestations of Bleeding
Bleeding in ALL patients can be from small spots to serious bleeding. The risk of bleeding is higher when platelets are very low. Doctors check platelet count, function, and other blood tests to see the risk.
Management Strategies
Handling thrombocytopenia and bleeding in ALL needs a few steps. Platelet transfusions help by raising platelet counts and lowering bleeding risk. It’s also key to fix the cause of low platelets, like changing chemotherapy or treating the leukemia.
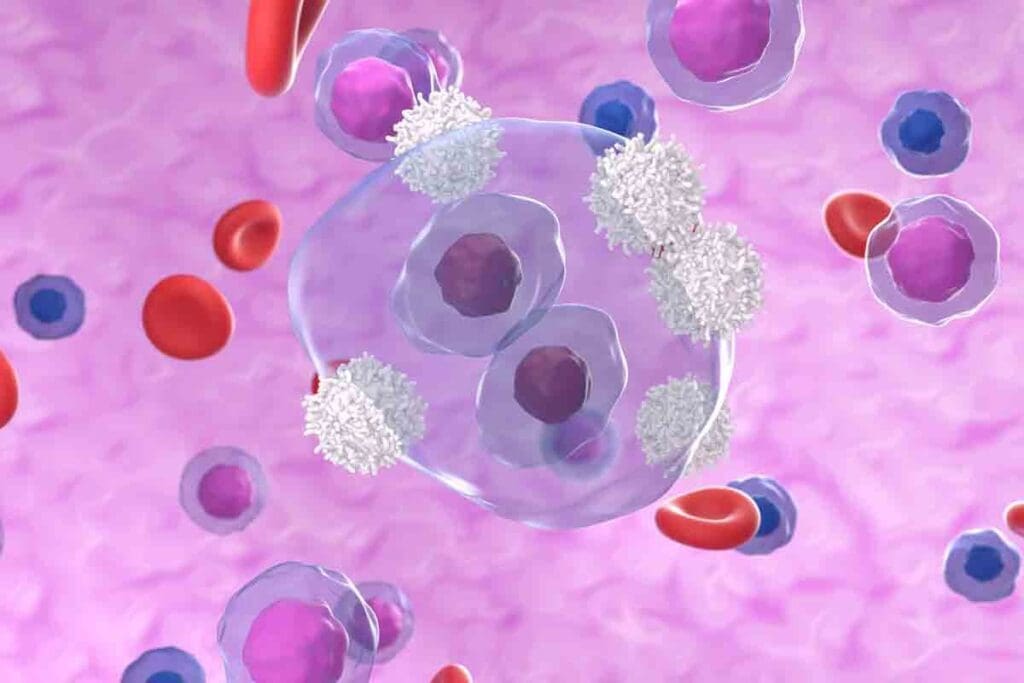
Complication #3: Neutropenia and Infectious Complications
Neutropenia is a big problem for people with Acute Lymphocytic Leukemia (ALL). It makes them more likely to get sick. This is because they have too few neutrophils, which fight off infections.
Bacterial, Viral, and Fungal Infections in ALL
ALL patients can get sick from many different germs. Bacterial infections are a big worry, with germs like Escherichia coli and Staphylococcus aureus being common. Viral infections, like the flu and RSV, are also serious. Fungal infections, caused by Candida and Aspergillus, are another big concern, mainly for those with long-lasting neutropenia.
Fever and Neutropenia: A Medical Emergency
Fever in a neutropenic patient is a medical emergency. It might be the only sign of an infection. This is because neutropenia can hide signs of infection like pus or swelling. Quick action is needed to avoid serious problems or death.
Prophylactic Strategies
To lower the risk of infections, doctors use several strategies. They give antimicrobial medicines to prevent infections. They also use G-CSF to help make more neutrophils, which shortens the time of neutropenia.
Treatment Approaches for Established Infections
When an infection is found, doctors start treatment right away. They use broad-spectrum antibiotics that might change based on test results and how the patient is doing. They also use antiviral and antifungal medicines for viral or fungal infections. Supportive care, like staying hydrated and getting enough nutrients, is also key in managing infections.
Complication #4: Central Nervous System (CNS) Involvement
Acute Lymphocytic Leukemia can affect the central nervous system, making treatment harder. It needs special tests and treatments to manage well.
Epidemiology and Risk Factors for CNS Infiltration
CNS involvement happens in some ALL patients. Certain genetic issues, high white blood cell counts, and specific cell markers increase this risk.
We look at these factors to plan treatments better. Knowing the risks helps us prevent and improve outcomes.
| Risk Factor | Description | Impact on CNS Involvement |
| Genetic Abnormalities | Specific chromosomal abnormalities | Increased risk |
| High WBC Count | Elevated white blood cell count at diagnosis | Higher risk of CNS infiltration |
| Immunophenotypic Features | Certain cell surface markers | Variable risk based on markers |
Neurological Manifestations and Diagnosis
CNS involvement can cause headaches, vomiting, and serious neurological problems. We diagnose it through a lumbar puncture, checking the cerebrospinal fluid for cancer cells.
Early detection is key for managing it well. We use advanced tests to find CNS involvement quickly.
CNS-Directed Therapy
Treatment for CNS involvement includes special therapies. These can be intrathecal chemotherapy, systemic chemotherapy, or cranial radiation. The choice depends on how much the CNS is involved and the patient’s health.
We customize treatments to fit each patient. We aim for the best results while avoiding long-term brain problems.
Long-term Neurological Sequelae
People who survive ALL with CNS involvement may face long-term brain issues. These can include memory problems, hormonal disorders, and new cancers. It’s important to follow up with them long-term to manage these problems.
Multidisciplinary care is key to reducing these long-term effects. It helps improve the quality of life for survivors.
Complication #5: Tumor Lysis Syndrome
Tumor lysis syndrome is a serious problem in ALL treatment. It happens when many cancer cells die fast, releasing their contents into the blood. This causes severe imbalances in electrolytes and can be very dangerous.
Pathophysiology and Risk Assessment
The cause of tumor lysis syndrome is the quick death of cancer cells, usually after chemotherapy. This death releases potassium, phosphate, and nucleic acids into the blood. The breakdown of nucleic acids to uric acid can cause hyperuricemia, and the potassium release can lead to hyperkalemia. People with a lot of cancer cells, fast-growing leukemia, or intense chemotherapy are at higher risk.
To assess risk, we look for signs like a high white blood cell count at diagnosis, big tumors, or kidney problems before treatment. Spotting these signs early helps us take steps to prevent the syndrome.
Clinical and Laboratory Manifestations
The symptoms of tumor lysis syndrome include cardiac arrhythmias from high potassium, neuromuscular irritability from low calcium, and acute kidney injury from uric acid. Lab tests show high levels of uric acid, potassium, phosphate, and low calcium.
- Hyperuricemia
- Hyperkalemia
- Hyperphosphatemia
- Hypocalcemia
Preventive Measures
Preventing tumor lysis syndrome is very important. We use aggressive hydration, rasburicase or allopurinol to lower uric acid, and closely watch electrolytes and kidney function. For those at high risk, these steps can greatly lower the chance of getting tumor lysis syndrome.
Management of Established Tumor Lysis Syndrome
When tumor lysis syndrome happens, we focus on careful monitoring and supportive care. This might include dialysis to fix severe electrolyte imbalances and kidney replacement therapy if kidney failure happens. Our goal is to keep the patient stable until the leukemia is controlled.
By knowing the risks and taking steps to prevent it, we can lessen the impact of tumor lysis syndrome in ALL patients. This helps improve their chances of recovery.
Complication #6: Organ Infiltration and Dysfunction
Leukemic cells can invade organs, causing serious problems in Acute Lymphocytic Leukemia (ALL) patients. This can lead to organ failure, affecting patients’ quality of life. We will look at the organs involved, symptoms of dysfunction, and how to manage these issues.
Hepatosplenomegaly and Liver Complications
Hepatosplenomegaly, or liver and spleen enlargement, is common in ALL. It happens when leukemic cells invade these organs. Liver dysfunction can cause liver failure in severe cases.
To manage liver problems, we:
- Regularly check liver function tests
- Adjust chemotherapy doses to reduce liver harm
- Use supportive care to manage symptoms
Renal Involvement and Acute Kidney Injury
ALL can cause kidney problems, like acute kidney injury (AKI). AKI happens when leukemic cells invade the kidneys or due to tumor lysis syndrome. It can lead to waste buildup, electrolyte imbalances, and fluid overload.
To handle kidney issues, we:
- Keep patients hydrated to prevent tumor lysis syndrome
- Watch kidney function closely
- Adjust medications to avoid kidney damage
- Use renal replacement therapy when needed
Cardiac and Pulmonary Manifestations
Leukemic cells can also affect the heart and lungs. Heart problems can lead to heart failure. Lung issues can range from infections to pulmonary leukemic infiltration.
| Organ | Complication | Management |
| Liver | Hepatosplenomegaly, Liver Dysfunction | Monitoring, Chemotherapy adjustment, Supportive care |
| Kidneys | Acute Kidney Injury | Hydration, Renal function monitoring, Medication adjustment, Renal replacement therapy |
| Heart and Lungs | Cardiac dysfunction, Pulmonary complications | Cardiac monitoring, Pulmonary support, Infection management |
Management Approaches for Organ Dysfunction
Managing organ dysfunction in ALL requires a team effort. This includes treating the leukemia, supportive care, and specific treatments for each organ. A multidisciplinary team is key in managing these complex cases.
Understanding organ infiltration and dysfunction helps healthcare providers create better treatment plans. This can improve patient outcomes.
Complication #7: Treatment-Related Toxicities
Acute Lymphocytic Leukemia (ALL) treatment includes chemotherapy, radiation, and stem cell transplants. These can cause serious side effects. It’s important to know about these to care for patients well.
Acute Chemotherapy Complications
Chemotherapy is key in fighting ALL. But, it can lead to problems like myelosuppression, mucositis, and hair loss. Myelosuppression makes it harder for the body to fight off infections and can cause anemia and bleeding.
Radiation Therapy Side Effects
Radiation is used in some ALL cases, mainly for brain involvement. It can cause tiredness, skin issues, and long-term risks like cancer and organ damage.
Stem Cell Transplantation Complications
Stem cell transplants can cure high-risk or relapsed ALL. But, they come with big risks like graft-versus-host disease, infections, and damage to organs.
To grasp the range of side effects from treatment, let’s look at a summary:
| Treatment Modality | Common Complications | Management Strategies |
| Chemotherapy | Myelosuppression, mucositis, alopecia | Supportive care, growth factor support, dose adjustments |
| Radiation Therapy | Fatigue, skin reactions, secondary malignancies | Symptom management, radiation planning to minimize exposure |
| Stem Cell Transplantation | GVHD, infections, organ toxicity | Immunosuppressive therapy, antimicrobial prophylaxis, close monitoring |
Handling side effects from ALL treatment needs a team effort. This includes teaching patients, giving supportive care, and watching them closely. Knowing about these complications helps us deal with the challenges of ALL treatment.
Complication #8: Long-Term and Late Effects
Medical progress has led to better survival rates for B-ALL patients. Now, we focus on managing long-term effects. Survivors of B Acute Lymphocytic Leukemia face various late effects. So, it’s key to have thorough follow-up care.
Secondary Malignancies: Risks and Surveillance
Survivors of B-ALL are at high risk for secondary malignancies. Surveillance strategies are essential for early detection and management. It’s important to have regular check-ups with a healthcare provider to watch for signs of secondary cancers.
- Annual skin exams to check for skin cancers
- Regular mammograms starting at age 25 or 8 years after radiation exposure, whichever is later
- Colonoscopy screening as recommended based on radiation exposure and family history
Cardiovascular Late Effects
Cardiovascular disease is a big concern for B-ALL survivors, mainly those who got anthracycline chemotherapy or chest radiation. Cardiac monitoring is key, and making lifestyle changes can help reduce risk.
- Regular echocardiograms to assess cardiac function
- Blood pressure management
- Lipid profile monitoring
Endocrine Dysfunction and Growth Impairment
Endocrine dysfunction and growth issues can happen due to radiation therapy, more so in children. Hormonal replacement therapy might be needed, and tracking growth is vital for kids.
Survivors should watch for thyroid, gonadal, and growth problems. Early treatment can greatly improve their outcomes.
Neurocognitive and Psychological Sequelae
Neurocognitive and psychological late effects can really affect B-ALL survivors’ quality of life. Cognitive rehabilitation and psychological support are key parts of care.
Survivors might find help in:
- Cognitive training programs
- Psychological counseling
- Support groups
Monitoring and Prevention Strategies for ALL Complications
Managing ALL complications requires a proactive approach. This includes advanced monitoring and preventive measures. It’s important to have a plan for managing Acute Lymphocytic Leukemia (ALL) complications. This plan should include risk-adapted monitoring, preventive measures, educating patients, and a coordinated care approach.
Risk-Adapted Monitoring Protocols
Risk-adapted monitoring protocols are key for early detection and management of complications in ALL patients. These protocols involve regular checks on the patient’s risk factors, disease status, and treatment response.
Key components of risk-adapted monitoring include:
- Regular blood counts and bone marrow assessments
- Imaging studies to detect organ involvement or damage
- Lumbar punctures to assess CNS involvement
- Cardiac monitoring for patients receiving anthracyclines
| Monitoring Parameter | Frequency | Purpose |
| Blood Counts | Weekly or biweekly | Detect cytopenias and infection risk |
| Bone Marrow Assessment | At diagnosis, after induction, and as needed | Assess disease response and detect relapse |
| Imaging Studies | As clinically indicated | Detect organ involvement or damage |
Preventive Interventions
Preventive interventions are vital in reducing the risk of complications in ALL patients. These interventions include:
- Prophylactic antibiotics and antifungals
- Tumor lysis syndrome prevention with hydration and allopurinol
- CNS prophylaxis with intrathecal chemotherapy
- Growth factor support to reduce neutropenia
“The use of preventive interventions has significantly improved outcomes in ALL patients by reducing the incidence of life-threatening complications.”
— Medical Expert, Hematologist
Patient Education and Self-Monitoring
Educating patients about their condition, treatment, and possible complications is essential. Patients should be able to recognize signs of complications and report them quickly.
Key areas for patient education include:
- Recognizing signs of infection or bleeding
- Understanding the importance of adherence to treatment
- Monitoring for symptoms of CNS involvement
- Maintaining a healthy lifestyle to mitigate treatment side effects
Multidisciplinary Approach to Complication Management
A multidisciplinary approach is key for managing ALL complications effectively. This involves teamwork between hematologists, oncologists, nurses, and other healthcare professionals.
The benefits of a multidisciplinary approach include:
- Comprehensive care coordination
- Improved communication between healthcare providers
- Enhanced patient support and education
- Better management of complex complications
Conclusion: Navigating the Complex Landscape of ALL Complications
Understanding and managing ALL complications is key to better patient outcomes. We’ve talked about the many issues that can arise, like severe anemia and tumor lysis syndrome. These are just a few examples.
Managing these problems well means being aware of the risks and watching patients closely. It also means using the right strategies to tackle these issues. A team effort is essential, focusing on the patient’s needs.
By tackling ALL complications head-on, we can make life better for patients. This includes improving their survival chances. It takes teamwork from doctors, patients, and families to manage these challenges effectively.
FAQ
What is Acute Lymphocytic Leukemia (ALL)?
Acute Lymphocytic Leukemia (ALL) is a blood cancer. It happens when too many immature white blood cells are made. It’s common in kids but can also affect adults.
What are the complications of Acute Lymphocytic Leukemia?
ALL can lead to serious problems. These include anemia, low platelets, and low white blood cells. It can also affect the brain, cause kidney problems, and lead to long-term health issues.
How does ALL affect different age groups?
ALL mostly hits kids under 5. But it can also affect adults. The disease is more aggressive in older adults.
What are the risk factors for developing ALL?
Some people are more likely to get ALL. This includes those with certain genes, exposure to harmful chemicals, and past radiation. Down syndrome also raises the risk.
What is tumor lysis syndrome, and how is it managed?
Tumor lysis syndrome is a serious side effect of ALL treatment. It happens when cancer cells burst in the blood. To manage it, doctors use lots of fluids, watch blood tests closely, and give medicines to lower uric acid.
How is CNS involvement in ALL diagnosed and treated?
Doctors check for CNS involvement with a spinal tap and scans. Treatment includes special chemotherapy and sometimes radiation for the brain and spinal cord.
What are the long-term effects of ALL treatment?
ALL treatment can cause lasting problems. These include new cancers, heart issues, hormone problems, and brain and mental health issues. Survivors need ongoing care to manage these effects.
How can complications of ALL be prevented or managed?
Managing ALL complications needs a team effort. This includes careful monitoring, preventive steps, teaching patients, and encouraging them to watch their health.
What is the role of stem cell transplantation in ALL treatment?
Stem cell transplantation is an option for some ALL patients. It’s for those with high-risk disease or who have relapsed. It replaces the bone marrow with healthy stem cells.
How does B cell Acute Lymphocytic Leukemia differ from other types of ALL?
B cell ALL has B cell markers on the leukemia cells. It often has a worse outlook than other ALL types.
References
1. Hunger, S. P., & Mullighan, C. G. (2015). Acute lymphoblastic leukemia in children. The New England Journal of Medicine, 373(16), 1541–1552. https://pubmed.ncbi.nlm.nih.gov/26465987/