Last Updated on November 20, 2025 by Ugurkan Demir
Diagnosing Acute Lymphoblastic Leukaemia (ALL) requires several detailed tests to identify abnormal lymphoblasts in the blood and bone marrow. The acute lymphoblastic leukaemia diagnosis process begins with blood work and a bone marrow biopsy, which help confirm the presence of leukemia cells.
The acute lymphoblastic leukaemia diagnosis often includes multiple steps, such as bone marrow aspiration, cytogenetic studies, and imaging tests like CT scans to determine how far the disease has spread. These tests provide doctors with the information needed to plan the most effective treatment.
At Liv Hospital, we combine advanced technology with compassionate care to deliver fast and accurate leukemia diagnoses. Our expert teams follow the latest medical standards to ensure that every patient receives precise results and a personalized treatment plan — helping them face this aggressive blood cancer with clarity and confidence.
Key Takeaways
- Diagnosing ALL involves a combination of blood tests, bone marrow biopsy, and genetic analysis.
- Blood tests and bone marrow aspiration are key for finding abnormal lymphoblasts.
- Imaging tests like CT scans may be used to check the disease’s spread.
- A diagnosis of ALL is confirmed when over 20 percent of bone marrow cells are lymphoblasts.
- Our expert teams use the latest medical protocols to provide clarity and confidence for patients facing ALL.
Understanding Acute Lymphoblastic Leukemia (ALL)
To understand Acute Lymphoblastic Leukemia, we need to know its definition, types, and how it affects children and adults. ALL is a cancer that affects the blood and bone marrow. It’s caused by the fast growth of immature white blood cells.
Acute Lymphoblastic Leukemia Definition
ALL is a cancer where lymphoblasts, or immature lymphocytes, don’t mature right. This leads to too many of these cells in the bone marrow and blood. The disease messes up normal blood cell making, causing health problems.
B-cell vs. T-cell ALL Classification
ALL is split into B-cell ALL and T-cell ALL based on the lymphocytes involved. B-cell ALL is more common, mainly in kids, making up about 85% of cases. T-cell ALL is more aggressive and often hits older kids and adults.
Childhood vs. Adult ALL
ALL shows up differently in kids and adults. Young kids, 2 to 5 years old, get ALL more often and usually do well with treatment. Adults, and older ones in particular, face a tougher time because of other health issues and less responsive disease.
| Characteristics | B-cell ALL | T-cell ALL | Childhood ALL | Adult ALL |
| Prevalence | More common (85%) | Less common (15%) | Higher incidence | Lower incidence |
| Age Group | Children and adults | Older children and adults | 2-5 years | Adults, specially older adults |
| Prognosis | Generally better in children | Poorer | Better response to treatment | Poorer due to comorbidities |
Knowing about Acute Lymphoblastic Leukemia, its types, and how it affects different ages is key for treatment. The differences between B-cell and T-cell ALL, and how it shows up in kids versus adults, help doctors plan better treatments.
Pathophysiology of Acute Lymphocytic Leukemia
To understand Acute Lymphocytic Leukemia (ALL), we need to look at its genetic and cellular roots. ALL happens when lymphoid cells grow out of control. This is mainly because of genetic changes in these cells.
Cellular Abnormalities in ALL
ALL starts with changes in lymphoid cells. These changes make the cells turn into cancer. This leads to too many immature cells in the bone marrow.
This buildup stops normal blood cells from being made. This causes problems like anemia and low white blood cell counts.
Key cellular abnormalities include:
- Dysregulation of cell cycle control mechanisms
- Impaired apoptosis (programmed cell death)
- Enhanced proliferative capacity of lymphoid cells
Genetic Mutations in Lymphoid Progenitor Cells
Genetic changes are key in ALL. These changes affect how cells grow, change, and live. Common changes include swapping genetic material, altering cell signaling, and changing the amount of genetic material.
| Genetic Mutation | Description | Impact on ALL |
| Chromosomal Translocations | Abnormal exchange of genetic material between chromosomes | Creates fusion genes that drive leukemogenesis |
| Mutations in Cell Signaling Genes | Alterations in genes involved in cell signaling pathways | Promotes proliferation and survival of leukemic cells |
| Deletions/Amplifications | Loss or gain of genetic material | Disrupts normal cellular regulation, contributing to leukemia |
Impact on Normal Blood Cell Development
ALL affects how blood cells are made. The bad cells in the bone marrow stop normal cells from being made. This leads to anemia, low white blood cells, and low platelets.
Understanding this helps us find better treatments. We can target the bad cells without harming the good ones.
By studying ALL’s cellular and genetic changes, we can find new ways to treat it. This is key to helping patients with ALL.
Etiology of Acute Lymphoblastic Leukemia
Acute Lymphoblastic Leukemia (ALL) is a complex disease. It involves genetics and environmental factors. Knowing these factors helps us prevent and treat it better.
Genetic Predisposition Factors
Genetics play a big role in ALL. Some people, like those with Down syndrome, are at higher risk. Syndromes like Li-Fraumeni and ataxia-telangiectasia also increase the risk.
Genetic changes, like in the IKZF1 gene, can lead to ALL. These changes affect lymphoid cells, which can cause leukemia.
Environmental Risk Factors
Environmental factors also raise the risk of ALL. Ionizing radiation is a known risk. People exposed to high levels of radiation, like those who had radiotherapy, are at higher risk.
Chemicals like benzene and pesticides are linked to ALL. Infections, including some in children, may also play a role.
Known Associations with Other Conditions
ALL is linked to other conditions. People who had chemotherapy or radiation for cancer are at higher risk. This is because ALL can develop as a secondary cancer.
Prenatal factors and exposures during pregnancy might also affect ALL risk in children. But, we need more research to understand these links.
By studying ALL’s causes, we can improve prevention, early detection, and treatment. This includes genetics and environmental factors.
Clinical Presentation and Symptoms
People with Acute Lymphoblastic Leukemia (ALL) often have symptoms like anemia, low platelets, and low white blood cells. The symptoms can differ a lot between children and adults. It’s important to know these differences to diagnose and treat correctly.
Common Signs and Symptoms
ALL symptoms include tiredness, easy bruising, and frequent infections. These happen because the leukemia cells stop normal blood cell production. Tiredness is often the first sign, caused by fewer red blood cells.
Easy bruising and bleeding happen because of low platelets. Frequent infections are due to low white blood cells, which fight off infections.
Differences in Presentation Between Children and Adults
Children with ALL might have symptoms like bone pain, fever, and feeling generally unwell. Adults, on the other hand, might have more severe symptoms like losing a lot of weight, night sweats, and more severe blood problems.
A leading hematologist said,
“The symptoms of ALL in adults are often more severe and aggressive than in children. Adults usually need more intense treatment right away.”
Emergency Presentations
Sometimes, ALL can be a medical emergency. This is when there’s a lot of leukemia cells, severe bleeding, or life-threatening infections. Quick action and treatment are key to avoid serious problems and improve health.
Emergency signs include severe shortness of breath, confusion, or signs of bleeding in the brain. Quick medical help is needed to stabilize the patient and start the right treatment.
Initial Assessment and Physical Examination
We start by doing a detailed check-up and looking at the patient’s health history. This helps us spot signs of Acute Lymphoblastic Leukemia (ALL).
This first step is key to finding out if someone has ALL. It helps us get the info we need for more tests. A careful check-up can show signs that point to the disease.
Key Physical Findings
We look for signs like pallor, bruising, and lymphadenopathy during the exam. These signs are often linked to ALL. They give us clues about the disease.
Medical History Evaluation
Looking at the patient’s health history is also important. We check their past health, treatments, and family history. This helps us find out if they might be at risk for ALL.
Initial Clinical Suspicion
After the exam and history check, we might suspect ALL. This suspicion is important. It tells us if we need to do more tests to confirm the diagnosis.
By using what we learn from the exam and history, we can decide what to do next. This helps us move forward in figuring out the diagnosis.
Acute Lymphoblastic Leukaemia Diagnosis: Laboratory Tests
Laboratory tests are key in diagnosing Acute Lymphoblastic Leukemia. They help identify the disease and its severity.
Complete Blood Count Analysis
A Complete Blood Count (CBC) is the first test for ALL. It checks red, white blood cells, and platelets. Abnormal counts suggest leukemia.
Key findings from a CBC in ALL patients may include:
- Anemia (low red blood cell count)
- Thrombocytopenia (low platelet count)
- Leukocytosis (high white blood cell count) or leukopenia (low white blood cell count)
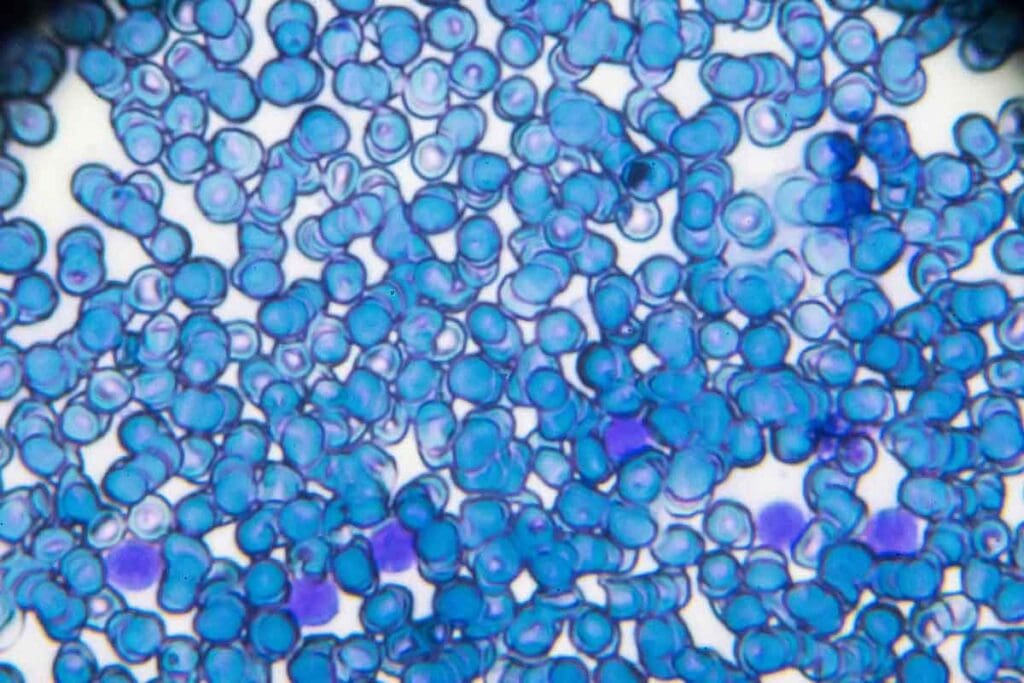
Peripheral Blood Smear Examination
A Peripheral Blood Smear examines blood under a microscope. It looks for blast cells, immature white blood cells seen in leukemia.
A medical expert notes, “Blast cells in the blood are a key sign of Acute Lymphoblastic Leukemia.”
“The diagnosis of ALL is often suggested by the presence of blast cells in the peripheral blood or bone marrow.”
Biochemical Markers
Biochemical markers, like lactate dehydrogenase (LDH), are high in ALL patients. They show how severe the disease is and its effects on the body.
Laboratory tests are vital for diagnosing ALL and planning treatment. By looking at blood counts, smears, and markers, doctors can create a treatment plan that fits the patient’s needs.
Bone Marrow Biopsy and Aspiration
Bone marrow biopsy and aspiration are key tools in diagnosing Acute Lymphoblastic Leukemia (ALL). They help us see if lymphoblasts are in the bone marrow and what they look like.
Procedure Overview
A bone marrow biopsy takes a small sample from the hipbone. Aspiration gets a liquid sample of bone marrow cells. These steps help us understand the bone marrow’s cells and find any problems.
First, we prepare the patient with local anesthesia to reduce pain. Then, we use a biopsy needle to take a sample. We also do aspiration to get a full view of the bone marrow.
Diagnostic Criteria for ALL
Diagnosing ALL mainly looks for lymphoblasts in the bone marrow. If more than 20% of the marrow is lymphoblasts, it’s ALL. We also check how these cells look to classify the disease.
The criteria are:
- Presence of lymphoblasts
- Percentage of lymphoblasts in bone marrow
- Morphological assessment of lymphoblasts
| Diagnostic Feature | ALL Criteria |
| Lymphoblast Percentage | >20% |
| Morphological Characteristics | L1, L2, or L3 type lymphoblasts |
Morphological Assessment
Looking at lymphoblasts’ shape and size is key for ALL subtypes. We use Wright-Giemsa stain to see these details.
Classifying ALL into L1, L2, or L3 helps us understand how aggressive it is.
By combining biopsy, aspiration, and looking at cell shapes, we can accurately diagnose ALL. This helps us plan the right treatment.
Flow Cytometric Immunophenotyping
Flow cytometric immunophenotyping is a key tool for diagnosing Acute Lymphoblastic Leukemia (ALL). It helps identify the unique traits of leukemia cells.
Identifying Cell Surface Markers
We use flow cytometric immunophenotyping to find specific markers on leukemia cells. These markers are vital for diagnosing and classifying ALL. They tell us about the cell’s lineage and maturity.
This method analyzes the surface antigens of lymphocytes. It helps us tell apart different leukemia types.
Distinguishing ALL Subtypes
By looking at the immunophenotypic profile, we can tell B-cell from T-cell ALL. This is key for choosing the right treatment.
Flow cytometry spots the unique markers of B-cell or T-cell lineage. This helps us identify the ALL subtype.
Minimal Residual Disease Assessment
Flow cytometric immunophenotyping also checks for minimal residual disease (MRD) in ALL patients.
MRD testing is important for seeing how well treatment is working. It helps predict the chance of relapse. We find small leukemic cells left after treatment.
With flow cytometric immunophenotyping, we can accurately diagnose ALL. We can also classify it and track treatment response. This guides our clinical decisions.
Cytogenetic and Molecular Analysis
In the world of ALL diagnosis, cytogenetic and molecular analysis are key. They help find chromosomal and genetic changes.
Cytogenetic analysis looks at chromosomes in cells. It’s vital for spotting ALL-related abnormalities. Chromosomal translocations, deletions, and aneuploidy are common in ALL and have significant prognostic implications.
Chromosomal Abnormalities in ALL
Chromosomal changes are a big deal in ALL. They affect both diagnosis and how well the disease will do. The most common changes include the Philadelphia chromosome and having too many or too few chromosomes.
Genetic Mutations and Prognostic Significance
Genetic mutations are key in ALL’s development. They help decide the risk level. Molecular analysis finds these mutations, making treatment more personal.
- Mutations in genes such as IKZF1 and TP53 mean a worse outlook.
- Some genetic changes affect treatment choices.
Advanced Molecular Testing Methods
New testing methods like next-generation sequencing (NGS) and PCR have changed ALL diagnosis. They spot minimal residual disease (MRD) and reveal leukemia’s genetic makeup.
NGS checks many genes at once, making diagnosis faster and more accurate. This is key for finding rare mutations that could help in treatment.
Imaging Studies and Additional Diagnostic Procedures
In diagnosing Acute Lymphoblastic Leukemia, imaging studies are key. They help see how far the disease has spread. Imaging modalities are vital for planning treatment.
Role of CT, MRI, and PET Scans
CT, MRI, and PET scans are used to diagnose and stage ALL. CT scans show detailed images of the body. They help find lymph nodes and organs affected by the disease.
MRI gives clear images of soft tissues. It’s great for spotting disease in the brain and testes. PET scans show where the disease is most active, helping find leukemia.
“The use of PET/CT in the initial staging of ALL has been shown to provide additional information that can lead to changes in treatment plans.”
Assessing Extramedullary Involvement
Extramedullary involvement means leukemia has spread beyond the bone marrow. Imaging studies are key to finding this spread. It can happen in lymph nodes, spleen, liver, and the brain.
- Lymphadenopathy: Enlarged lymph nodes can be seen on CT or MRI.
- Organomegaly: Big spleen and liver can be checked with imaging.
- CNS involvement: MRI is best for finding disease in the brain.
Cardiac Evaluation
Before starting treatment for ALL, a heart check is needed. This is because some treatments can harm the heart. Echocardiography or MUGA scans are used to check the heart’s function.
As a study found,
“Cardiac assessment before and during treatment is key to avoid heart damage in ALL patients.”
Lumbar Puncture and CNS Evaluation
Diagnosing and treating Acute Lymphoblastic Leukemia (ALL) needs a detailed look at the central nervous system (CNS). A lumbar puncture, or spinal tap, is a key part of this process.
Detecting Central Nervous System Involvement
CNS involvement is a big worry in ALL. Leukemia cells can get into the cerebrospinal fluid (CSF). Finding out if this has happened is key for planning treatment.
We do a lumbar puncture to get CSF for testing. This helps us see if leukemia cells have reached the CNS.
Cerebrospinal Fluid Analysis
Looking at CSF is a big part of checking the CNS. We check for lymphoblasts, which are young cells seen in leukemia.
If we find lymphoblasts in the CSF, it means the CNS is involved. This changes how we plan treatment and what we expect for the future. We also check the CSF for protein and glucose levels to see how well the CNS is doing.
Prophylactic CNS Treatment Considerations
For patients with ALL, we often plan to prevent CNS relapse. This is very important for those at high risk of CNS involvement.
We make the treatment plan based on each patient’s risk and disease details. This might include intrathecal chemotherapy. This is when we put chemotherapy directly into the CSF through a lumbar puncture.
Conclusion: From Diagnosis to Treatment Planning
After getting a diagnosis of acute lymphoblastic leukemia (ALL), the next step is treatment planning. We work closely with patients to create a plan that fits their needs. This plan considers the diagnosis, how likely the patient is to recover, and what the patient needs.
Planning treatment for ALL is a team effort. It includes chemotherapy, targeted therapy, and other treatments as needed. Our aim is to find the best treatment for each patient’s leukemia.
We understand each patient’s diagnosis and how likely they are to recover. This helps us make a treatment plan that’s just right for them. Our team is dedicated to giving top-notch care to international patients with ALL.
Good treatment planning is key to helping patients with ALL do well. We’re committed to giving the best care, from the start of treatment to after it’s done. We make sure patients get the support they need every step of the way.
FAQ
What is Acute Lymphoblastic Leukemia (ALL)?
Acute Lymphoblastic Leukemia (ALL) is a cancer where abnormal lymphocytes grow too much. It’s divided into B-cell and T-cell types, with B-cell being more common.
What are the common symptoms of Acute Lymphoblastic Leukemia?
Symptoms of ALL include feeling very tired, bruising easily, and getting infections. Kids might not show clear signs, while adults often have more serious symptoms.
How is Acute Lymphoblastic Leukemia diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests to diagnose ALL. They confirm it when more than 20 percent of bone marrow cells are lymphoblasts.
What is the role of genetic mutations in Acute Lymphoblastic Leukemia?
Genetic changes in lymphoid cells cause them to grow uncontrollably. This disrupts normal blood cell production, leading to ALL.
What are the differences in Acute Lymphoblastic Leukemia between children and adults?
ALL impacts kids and adults differently. Kids usually have a better chance of recovery. Kids might not show clear symptoms, while adults often have more severe ones.
What is the significance of B-cell vs. T-cell classification in Acute Lymphoblastic Leukemia?
Knowing if it’s B-cell or T-cell ALL helps doctors understand the disease better. It also guides treatment plans. B-cell ALL is more common, which affects prognosis and treatment.
How is the diagnosis of Acute Lymphoblastic Leukemia confirmed?
Doctors confirm ALL through blood tests, bone marrow biopsies, and smears. These tests check for abnormal cells.
What is the role of imaging studies in Acute Lymphoblastic Leukemia diagnosis?
Imaging like CT, MRI, and PET scans help see if the disease has spread. They check for growth outside the bone marrow.
What is the importance of lumbar puncture in Acute Lymphoblastic Leukemia diagnosis?
Lumbar punctures check for cancer in the brain. They analyze cerebrospinal fluid for lymphoblasts. This helps prevent brain relapse.
How is treatment planning done for Acute Lymphoblastic Leukemia?
Treatment planning is a team effort. It considers the diagnosis, how likely the patient is to recover, and their needs. It includes chemotherapy, targeted therapy, and other treatments as needed.
References
- Roberts, K. G., & Mullighan, C. G. (2018). Genetics and prognosis of acute lymphoblastic leukemia in children vs. adults. Blood, 131(2), 197–204. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6245970/





