For those dealing with liver or bile duct issues, the thought of liver stent surgery can be scary. But, thanks to recent advancements, this procedure now offers a safer and more effective way to find relief.
At Liv Hospital, we’re at the forefront in treating patients who need a bile duct stent. Our skilled team is here to support and guide you every step of the way.
We’ll dive into why liver stent surgery is key in treating blockages in the bile duct. We’ll also look at the main reasons doctors might suggest a bile duct stent.
Key Takeaways
- Understanding the role of liver stent surgery in treating bile duct blockages
- Recognizing the benefits of bile duct stent placement
- Identifying conditions that require liver stent surgery
- Learning about the expertise offered by Liv Hospital
- Discovering the extensive support provided to patients
The Critical Role of Bile Flow in Digestive Health
Bile flow is key for digesting and absorbing nutrients. The biliary system, including the liver, gallbladder, and bile ducts, is vital for our digestive health.
How the Biliary System Functions
The biliary system makes, stores, and moves bile. Bile, made by the liver, is essential for digesting fats and absorbing fat-soluble vitamins.
- The liver produces about one liter of bile daily.
- Bile is stored in the gallbladder.
- When food enters the small intestine, bile is released to emulsify fats, making them easier to digest.
What Happens When Bile Flow Is Obstructed
When bile flow is blocked, it can cause health issues like jaundice, itchy skin, and digestive problems. Blockages can be due to gallstones, tumors, or inflammation.
The consequences of obstructed bile flow can be severe. If not treated, it can lead to serious conditions like cholangitis, an infection of the bile duct, or secondary biliary cirrhosis, which can cause liver failure.
Restoring bile flow is essential. One effective way is through the placement of a bile duct stent. This procedure ensures bile flows freely, easing symptoms and preventing further issues.
“The placement of a bile duct stent is a highly effective procedure for restoring bile flow and improving the quality of life for patients with bile duct obstruction.”
Understanding Liver Stent Surgery and Bile Duct Stenting

For those dealing with bile duct problems, knowing about liver stent surgery is key. This surgery puts a stent in the bile duct to clear blockages and keep bile flowing right. We’ll look into the details of this procedure, including the stents used and when they’re temporary or permanent.
Definition and Purpose of Biliary Stents
Biliary stents are devices that keep the bile duct open, ensuring bile flows as it should. They’re mainly used to remove blockages from tumors, scar tissue, or stones. By keeping bile flowing, stents prevent jaundice, infection, and liver damage. For more on caring for your stent, check out MyHealth.Alberta.ca.
Types of Stents Used in Bile Duct Procedures
There are two main stent types: plastic and metal. Plastic stents are cheaper and work well for short-term use. But, they can clog easily and need replacing often. Metal stents, being more durable and less likely to clog, are better for longer use.
| Stent Type | Material | Duration of Use |
| Plastic Stents | Polyethylene or other plastics | Temporary (weeks to months) |
| Metal Stents | Stainless steel or alloys | Permanent or long-term (months to years) |
Temporary vs. Permanent Stent Placement
Choosing between a temporary or permanent stent depends on the cause of the blockage. Temporary stents are used when the blockage is likely to clear, like after surgery. Permanent stents are for chronic issues or when the blockage won’t go away. We’ll dive deeper into stent placement and care in the next sections.
Reason 1: Treating Malignant Bile Duct Obstruction
Liver stent surgery is key in managing malignant bile duct obstruction. This condition happens when a tumor blocks the bile duct. It stops bile from flowing into the intestine.
This blockage can cause severe jaundice, intense itching, and serious infections. These symptoms can be very dangerous.
Pancreatic Cancer and Bile Duct Blockage
Pancreatic cancer is a common cause of this blockage. As the tumor grows, it can press on or invade the bile duct. Liver stent surgery helps relieve this blockage.
It places a stent in the bile duct to keep it open. This allows bile to drain freely. It improves the patient’s quality of life and prepares them for other treatments.
Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinoma, or bile duct cancer, also causes bile duct obstruction. This cancer starts in the bile duct and can block bile flow. Stenting is a key treatment to manage symptoms and improve outcomes.
- Relieves jaundice and associated symptoms
- Improves quality of life
- Facilitates further cancer treatment
Metastatic Liver Disease Affecting Biliary Drainage
Metastatic liver disease can also block bile ducts. When cancer spreads to the liver, it can affect biliary drainage. Bile duct stenting is effective in managing these obstructions.
It ensures proper bile flow and reduces complications. Understanding the causes and treatments for malignant bile duct obstruction helps patients and healthcare providers make better decisions.
The use of liver stent surgery has greatly improved care for these patients. It offers hope and better quality of life.
In conclusion, liver stent surgery is vital for treating malignant bile duct obstruction caused by cancer. It restores bile flow, relieves symptoms, improves outcomes, and enhances quality of life.
Reason 2: Managing Benign Biliary Strictures
Liver stent surgery is key for treating benign biliary strictures. It helps those with this serious condition. These strictures can come from surgery, chronic pancreatitis, or primary sclerosing cholangitis.
Post-Surgical Complications Leading to Strictures
After surgery, strictures can form in the bile duct. This is due to injury or scarring. Liver stent surgery is a gentle way to fix this, keeping bile flowing and preventing more problems.
Chronic Pancreatitis Effects on Bile Ducts
Chronic pancreatitis can cause inflammation and scarring in the bile duct. This leads to strictures. Stenting in bile duct helps by keeping the duct open, easing symptoms like jaundice and pain.
Primary Sclerosing Cholangitis Management
Primary sclerosing cholangitis (PSC) is a chronic liver disease. It causes inflammation and scarring in the bile ducts, leading to strictures. Using a bile duct stent can improve bile flow and lower the risk of complications.
Understanding and treating benign biliary strictures is important. Liver stent surgery is a safe and effective way to manage these issues. It helps improve patient outcomes significantly.
Reason 3: Addressing Common Bile Duct (CBD) Stones
Common Bile Duct (CBD) stones often block the bile duct. Liver stent surgery is key in treating this issue. These stones can lead to serious symptoms and problems, making quick and effective treatment vital.
When Stone Extraction Is Unsuccessful
At times, removing CBD stones through ERCP doesn’t work. This might be because the stones are too big, there are many of them, or they’re hard to reach. In such cases, stent placement is a critical backup to ensure bile flow and avoid complications.
Stenting keeps the bile duct open, allowing bile to flow into the intestine. This is very important for patients who can’t have surgery or when surgery is delayed.
Preventing Recurrent Stone Formation
Some people are more likely to get CBD stones again. In these cases, stent placement can be a long-term fix to stop stones from coming back. Stents keep the bile duct open, lowering the chance of new stones and problems.
Regular follow-up is key for patients with stents. It helps catch any problems like stent blockage or movement early. This proactive approach improves patient results.
Stenting After Failed ERCP Stone Removal
If ERCP can’t remove stones, stenting is a good backup. Stents keep the bile duct open, helping bile drain and lowering the risk of infections or other issues.
Deciding to put in a stent after ERCP failure depends on many things. These include the patient’s health, the size and location of the stones, and any other bile duct problems. Personalized treatment planning is key to the best results.
Reason 4: Relieving Jaundice and Associated Symptoms
Bile duct obstruction leads to jaundice, causing the skin and eyes to turn yellow. This can really affect a person’s life quality. Liver stent surgery can help fix this problem.
Mechanism of Jaundice in Bile Duct Obstruction
When the bile duct is blocked, bile and bilirubin can’t move into the intestine. This causes bilirubin to build up in the blood, leading to jaundice. The blockage might be caused by stones, tumors, or strictures.
Bilirubin Buildup: The liver breaks down bilirubin from old red blood cells. Normally, it’s moved into the bile and then the intestine. But with a blockage, bilirubin stays in the blood, causing jaundice.
Quality of Life Improvements After Stenting
Liver stent surgery can greatly improve life for those with jaundice. It helps bile flow, lowering bilirubin in the blood. This makes jaundice and related symptoms better.
Patients often notice:
- Less itching
- Better appetite
- Improved overall feeling
- Enhanced digestion
These changes are key for those with cancer or needing palliative care.
Timeline for Symptom Resolution Post-Stenting
How fast symptoms get better after stenting varies. Most people see improvements in a few days to a week.
| Timeline | Expected Improvements |
| 1-3 days | Initial reduction in bilirubin levels |
| 3-7 days | Noticeable decrease in jaundice |
| 1-2 weeks | Significant improvement in symptoms and quality of life |
Understanding jaundice and stenting’s benefits helps patients see the need for quick action. Liver stent surgery not only eases jaundice but also boosts patient outcomes.
Reason 5: Preventing and Treating Cholangitis
Liver stent surgery is key in stopping and treating cholangitis. This is a dangerous infection that can happen when the bile duct gets blocked. It’s caused by bacteria and can get very serious if not treated fast.
Acute Cholangitis as a Medical Emergency
Acute cholangitis is a serious issue that needs quick action. It shows up with fever, jaundice, and belly pain. If not treated right away, it can turn into sepsis, which is very dangerous.
Key symptoms of acute cholangitis:
- Fever and chills
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain, mainly in the upper right side
Role of Stents in Preventing Recurrent Infection
Bile duct stents are very important in stopping cholangitis from coming back. They keep the bile duct open, which helps bile flow. This is very helpful for people with frequent blockages.
| Benefits of Stenting | Description |
| Restores Bile Flow | Ensures bile flows freely into the intestine, lowering infection risk. |
| Reduces Risk of Recurrent Cholangitis | Stents keep the bile duct open, lowering bacterial infection chance. |
| Improves Patient Outcomes | Good stenting can greatly improve life quality for those with bile duct blockages. |
Managing Recurrent Cholestasis with Stenting
Stenting is a good way to handle recurrent cholestasis. This is when bile flow slows down or stops. Stents keep the bile duct open, preventing cholestasis from coming back.
Stents in managing cholestasis improve patient results and cut down on the need for more treatments.
Reason 6: Serving as a Bridge to Surgery in Complex Cases
In complex surgical cases, liver stent surgery is key. It acts as a bridge to more definitive treatments. Patients often need to be stabilized before major surgeries. Liver stent surgery helps by improving their condition before surgery.
Preoperative Biliary Drainage Benefits
Preoperative biliary drainage is a big plus of liver stent surgery. It helps by relieving biliary obstruction. This reduces the risk of complications after surgery.
Studies show that preoperative drainage can lead to fewer infections. It also improves overall surgical outcomes.
“Preoperative biliary drainage has been shown to significantly reduce the incidence of postoperative complications in patients undergoing surgery for biliary obstruction.”
Nature Reviews Gastroenterology & Hepatology
Improving Surgical Outcomes Through Stenting
Stenting makes surgery better by ensuring the biliary system works well before surgery. This makes the surgery simpler and improves recovery chances.
| Surgical Outcome | With Stenting | Without Stenting |
| Postoperative Complications | Reduced | Increased |
| Surgical Complexity | Lower | Higher |
| Recovery Time | Faster | Slower |
Timing Considerations for Stent Placement Before Surgery
The timing of stent placement is very important. We aim to balance the benefits of preoperative drainage with the risks of stent placement. Usually, stenting happens a few weeks before surgery to ensure good biliary drainage.
By planning stent placement carefully, we can make liver stent surgery more effective. It helps prepare patients for more complex surgeries.
Reason 7: Providing Palliative Care in Advanced Disease
Advanced disease often requires new approaches to care, like liver stent placement. The main goal changes from curing to improving life quality. Palliative care is key in managing symptoms and complications of terminal illnesses.
Improving Quality of Life in Terminal Illness
For those with terminal bile duct obstruction, liver stent surgery can greatly improve life quality. It helps restore bile flow, easing jaundice and pruritus. Our aim is to provide relief and comfort, helping patients maintain dignity and spend time with loved ones.
This procedure is very helpful for those with advanced pancreatic cancer or cholangiocarcinoma. It improves bile drainage, reducing the risk of cholangitis and other complications. This enhances the patient’s overall well-being.
Managing Symptoms in Inoperable Cases
Inoperable cases are challenging, but liver stent placement offers a solution. We’ve seen big improvements in symptom management, mainly in patients with malignant biliary obstruction. Stenting:
- Relieves jaundice and related symptoms
- Reduces the risk of cholangitis
- Improves nutritional status by restoring bile flow
- Enhances overall quality of life
By tackling these critical areas, we significantly improve patient comfort and quality of life.
Long-term Stent Management in Palliative Settings
Managing liver stents long-term is vital in palliative care. Regular follow-ups are needed to check stent patency and address any issues quickly. We work closely with patients and caregivers to ensure they know the signs of stent problems, allowing for timely action.
| Aspect | Description | Benefits |
| Symptom Management | Effective relief of jaundice, pruritus, and other symptoms | Improved quality of life |
| Stent Patency | Regular monitoring to prevent occlusion | Reduced risk of complications |
| Patient Education | Empowering patients and caregivers with knowledge | Timely intervention in case of complications |
By focusing on these areas, we offer complete palliative care for patients with advanced disease.
The Liver Stent Surgery Procedure Explained
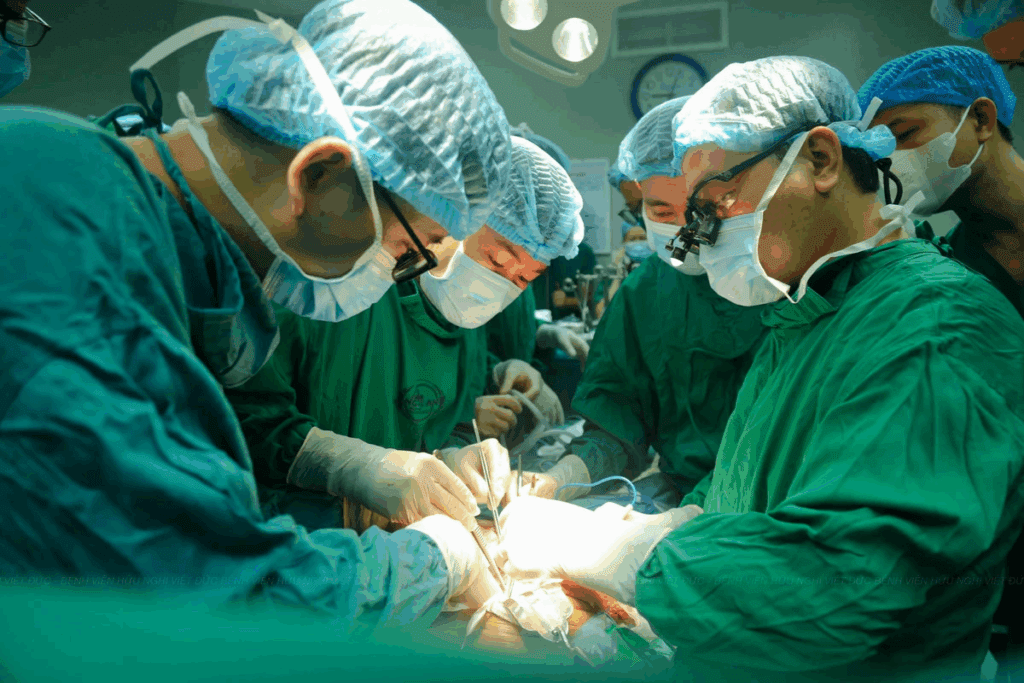
We will explain the liver stent surgery process. This includes the techniques and what you can expect. Liver stent surgery is a complex procedure. It involves placing a stent in the bile duct to restore normal bile flow.
This procedure is key for patients with bile duct obstruction. It can be caused by various reasons.
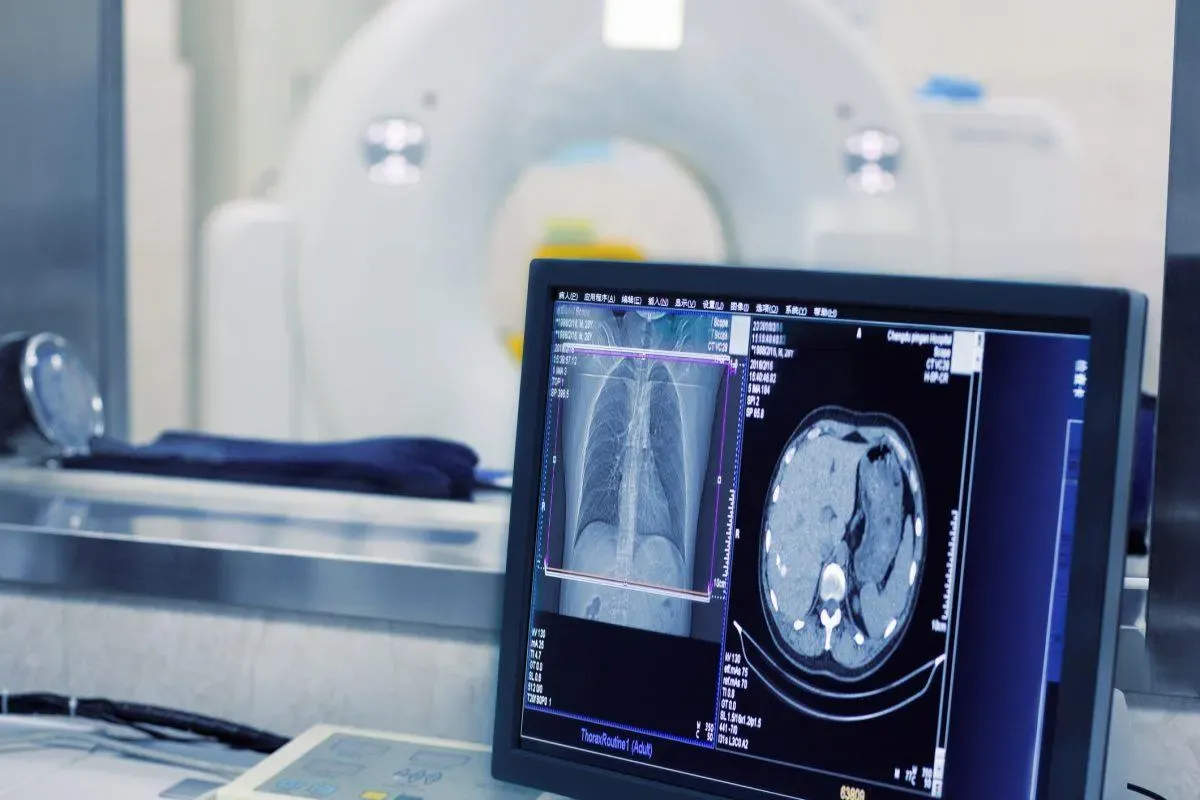
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a common technique for liver stent placement. It uses a flexible tube with a camera and instruments. This allows us to see the bile duct and place the stent.
We use ERCP to access the bile duct through the mouth. This avoids external incisions. The procedure is done under sedation to reduce discomfort.
During ERCP, we first find the blockage in the bile duct. We use contrast dye and X-ray imaging for this. Once found, we place the stent to open up the blocked area. This allows bile to flow freely into the intestine.
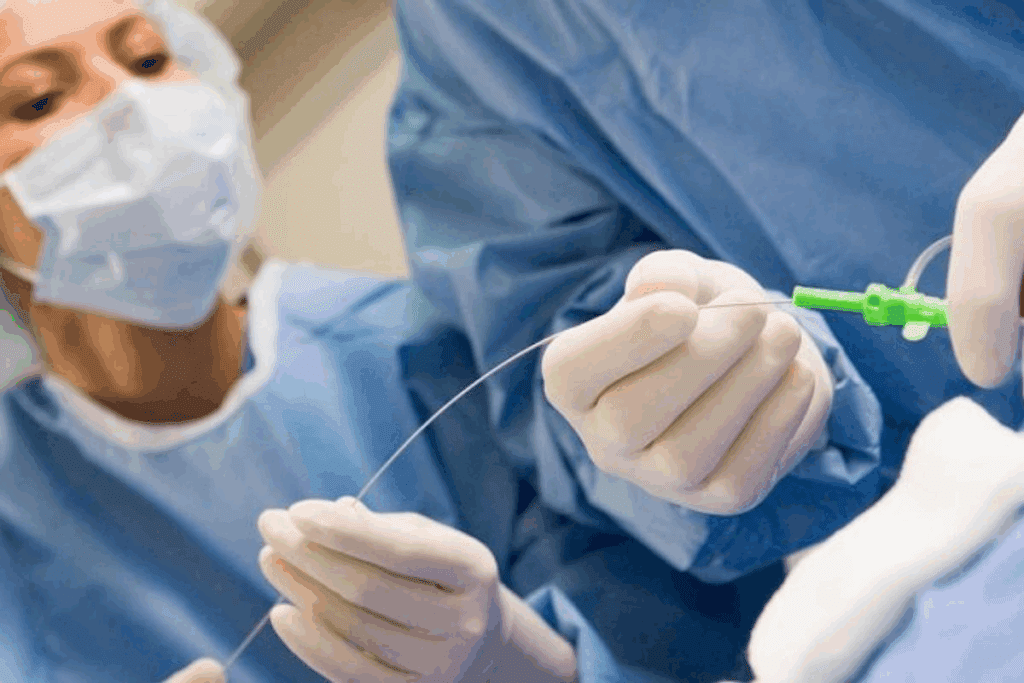
Percutaneous Transhepatic Cholangiography (PTC)
In some cases, PTC is used as an alternative or in conjunction with ERCP. PTC accesses the bile duct through the skin and liver tissue. It uses a needle and guidewire.
PTC is useful when ERCP is not feasible. This is due to certain anatomical issues or when the blockage is high up in the bile ducts. We carefully plan the approach for the safest and most effective outcome.
Recovery and Aftercare Following Stent Placement
After stent placement, recovery and aftercare are key for a successful outcome. Patients are monitored for a few hours post-procedure. We check for any immediate complications.
We provide specific instructions on diet, activity level, and follow-up appointments. This ensures the stent functions properly and addresses any concerns.
It’s important for patients to report any symptoms like fever, severe abdominal pain, or jaundice. These could indicate complications. With proper care and follow-up, most patients can return to their normal activities within a few days.
We understand that liver stent surgery can be daunting. But with our experienced team and state-of-the-art facilities, we are committed to providing the best care and support throughout your treatment journey.
Potential Complications of Bile Duct Stents
Bile duct stents are key for treating many biliary issues. Yet, they can lead to several complications. It’s important for doctors and patients to know about these risks to get the best care.
Stent Migration and Occlusion
Two major issues with bile duct stents are stent migration and occlusion. Stent migration means the stent moves from where it was placed. This can block the bile duct and cause pain and jaundice. Stent occlusion happens when the stent gets blocked, often by sludge or tumors. This can lead to jaundice and cholangitis, a serious infection.
- Stent migration can cause abdominal pain and jaundice.
- Occlusion may result in cholangitis, a potentially life-threatening infection.
- Regular monitoring is key to catch these problems early.
Managing a Blocked Bile Duct Stent
When a bile duct stent gets blocked, there are steps to take. First, doctors use imaging like ultrasound or CT scans to confirm the blockage. Then, they might:
- Clear the stent with an endoscope.
- Replace the stent with a new one.
- Put in more stents to keep the bile duct open.
These actions help get bile flowing again and ease symptoms.
Infection and Bleeding Risks
Bile duct stenting also carries risks of infection and bleeding. Cholangitis, an infection of the bile duct, can happen if the stent gets blocked or if bacteria grow. Bleeding might occur from the procedure or damage to the bile duct wall.
To lower these risks, doctors often give antibiotics before the procedure. Patients should watch for signs of infection or bleeding, like fever, pain, or jaundice.
When to Seek Medical Attention
It’s important for patients to know when to get help. Look for these signs that need immediate doctor’s care:
- Severe abdominal pain.
- Fever or chills.
- Jaundice or dark urine.
- Signs of bleeding, such as black stools or vomiting blood.
Quick action to address these issues can greatly improve health outcomes.
Advances in Bile Duct Stent Technology
The field of bile duct stenting has seen big changes in recent years. These changes have made stent placement safer and more effective. This has improved how well patients do after treatment.
Evolution from Plastic to Metal Stents
At first, bile duct stents were made of plastic. But they had problems like getting blocked often and needing to be replaced a lot. Moving to metal stents has helped fix these issues.
Metal stents have better success rates and need less fixing. They work best for people with cancer blocking their bile ducts.
Now, metal stents are the preferred choice because they last longer and work better. Their main advantages are:
- They stay open longer
- They block less often
- They need less fixing
Drug-Eluting and Biodegradable Stents
New stents can release medicine to stop blockages and dissolve over time. Drug-eluting stents release medicine to keep the stent open. Biodegradable stents dissolve, so you don’t need to remove them.
These new stents are promising for treating biliary problems. For example, drug-eluting stents can stop blockages. Biodegradable stents can avoid long-term problems.
Improved Patency Rates with Modern Stent Designs
New stent designs aim to keep them open longer. They have features like covers and special coatings to prevent problems.
These design changes have greatly helped patients. Modern stents have important features like:
- Covers to stop tumors from growing
- Special coatings to keep them in place
- Medicine to keep them open
Future Directions in Stent Development
Technology will keep getting better, leading to new stent designs. We might see stents that release more medicine, dissolve faster, and fit each patient’s needs better.
These new stents will be key in the future of bile duct stenting. Knowing about these changes helps doctors give the best care to patients with bile duct stents.
Conclusion: The Life-Changing Impact of Appropriate Bile Duct Stenting
Liver stent surgery and bile duct stenting are key for managing bile duct blockages. They greatly improve how patients feel and do. Knowing the good and bad sides of these treatments helps patients choose the best care for themselves.
Getting the right bile duct stenting can really change a person’s life. It helps get rid of jaundice and stops infections. New stent technologies, like metal and drug-eluting ones, make these treatments even better.
It’s clear that quick and right stenting is key for dealing with bile duct blockages. We’ve covered the main points to show how important bile duct stenting is. As medical tech gets better, we’ll see even more improvements in liver stent surgery and bile duct stenting. This means better care for people all over the world.
FAQ
What is liver stent surgery and how does it help in treating bile duct obstruction?
Liver stent surgery is a procedure where a stent is placed in the bile duct. This helps to relieve blockages and supports normal bile flow. It can help reduce symptoms like jaundice and itchy skin.
What are the different types of stents used in bile duct procedures?
There are plastic and metal stents used in bile duct procedures. The choice depends on the condition and whether the stent is temporary or permanent.
What are the reasons for bile duct stent placement?
Stents are placed for several reasons. These include treating malignant bile duct blockages, benign strictures, and common bile duct stones. They also help relieve jaundice and prevent cholangitis.
How does liver stent surgery help in managing malignant bile duct obstruction?
Liver stent surgery helps manage malignant blockages by restoring bile flow. This is important for patients with cancers like pancreatic cancer and cholangiocarcinoma.
What is the role of stenting in preventing and treating cholangitis?
Stenting is key in preventing and treating cholangitis. It ensures bile flows normally, reducing infection risk and complications.
How does liver stent surgery serve as a bridge to surgery in complex cases?
Liver stent surgery can improve outcomes by providing preoperative drainage. It enhances surgical success and optimizes stent placement timing.
What are the benefits of liver stent surgery in providing palliative care in advanced disease?
Liver stent surgery improves quality of life and manages symptoms in advanced disease. It provides long-term management in palliative care settings.
What are the possible complications of bile duct stents?
Complications include stent migration, occlusion, infection, and bleeding. It’s important to seek medical help if these issues arise.
What advances have been made in bile duct stent technology?
Advances include the shift from plastic to metal stents. There are also drug-eluting and biodegradable stents. Modern designs have improved patency rates.
What is the difference between ERCP and PTC in liver stent surgery?
ERCP and PTC are techniques used in liver stent surgery. ERCP is more common for stent placement. PTC is used when ERCP is not possible.
What is the recovery process like after liver stent surgery?
Recovery involves monitoring for complications and managing symptoms. The process varies based on individual needs.
How does stenting help in managing benign biliary strictures?
Stenting improves bile flow and reduces symptoms in benign strictures. It aims to prevent future strictures.
Can liver stent surgery be used to manage common bile duct stones?
Yes, liver stent surgery can manage common bile duct stones. It’s used when extraction is unsuccessful or to prevent future stones.
References
- Baron, T. H., & Kozarek, R. A. (2023). Endoscopic management of biliary strictures and stones: Current perspectives and future directions. Gastroenterology Clinics of North America, 52(2), 275-290. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7452929/