
Endovascular thrombectomy (EVT) is a new way to treat acute ischemic stroke. This happens when a blood clot blocks a big brain vessel. AtLiv Hospital, we use EVT to remove these clots. This minimally invasive procedure has changed how we treat strokes, giving patients and their families new hope.
Pete Wilkins’ story shows how well EVT medical treatment works. He got treated with EVT and recovered quickly. Stories like his highlight the need for quick action in treating strokes. EVT is a key treatment that can greatly help patients if done fast.
Key Takeaways
- EVT is a minimally invasive procedure used to treat acute ischemic stroke.
- The procedure involves mechanically removing blood clots from large brain vessels.
- Timely intervention with EVT can significantly improve patient outcomes.
- EVT has revolutionized stroke care, giving patients new hope.
- Liv Hospital is at the forefront of using EVT for stroke treatment.
Understanding Stroke and the Need for Rapid Treatment
Stroke is a serious medical emergency that needs quick action. Knowing about its types and how it affects the brain is key to treating it well. When a stroke happens, the brain doesn’t get the oxygen and nutrients it needs. This can lead to cell death and serious long-term problems.
There are three main types of stroke. Ischemic stroke is the most common, making up about 87% of all strokes. It happens when a blood clot blocks an artery to the brain. Hemorrhagic stroke occurs when a blood vessel in the brain bursts, causing bleeding. Transient ischemic attack (TIA), or “mini-stroke,” is a temporary blockage that doesn’t cause lasting harm.
Types of Stroke and Their Impact
Stroke can have a big impact, affecting not just the person but also their family and community. The severity depends on the stroke type, the brain area affected, and how quickly and well treatment is given. For example, ischemic strokes can cause significant disability if not treated quickly.
Dr. Marsha Eustace stresses the importance of calling 911 right away if stroke symptoms are seen. She says “time is brain,” showing how urgent it is to act fast to prevent brain damage.
The Critical Time Window for Intervention
The time to treat a stroke is short. For ischemic stroke, endovascular thrombectomy (EVT) can be done up to 24 hours after the stroke starts in some patients. The sooner EVT is done, the better the chances of a good outcome. So, knowing the time window for treatment is important for both doctors and the public.
Quick treatment not only saves lives but also improves the quality of life for those who survive. By understanding the urgency of stroke treatment, we can all help reduce its impact on people and communities.
What Is EVT Medical: Defining Endovascular Thrombectomy
Endovascular Thrombectomy, or EVT, is a new way to treat strokes. It’s a minimally invasive method that helps restore blood flow to the brain. This has changed how we treat acute ischemic strokes.
The Meaning Behind EVT Medical Abbreviation
The EVT medical term means Endovascular Thrombectomy. Endovascular means it’s done inside the blood vessels. Thrombectomy is about removing clots. So, EVT is a procedure that removes blood clots from the blood vessels, mainly for stroke treatment.
Historical Development of Thrombectomy Procedures
Thrombectomy has been around for decades, but its use in treating strokes has grown a lot. Early attempts were made, but it wasn’t until better endovascular tools came along that EVT became a real option.
The history of EVT includes important steps:
| Year | Milestone | Description |
| Early 2000s | Introduction of First-Generation Thrombectomy Devices | First devices were big and not very good, but they started the journey to better treatments. |
| 2010s | Advancements in Stent Retrievers | Stent retrievers were a big leap forward, making it easier to get rid of clots. |
| 2015 | Publication of Landmark Clinical Trials | Trials like MR CLEAN showed how well EVT works, making it a standard treatment. |
Thanks to these improvements, EVT is now a key treatment for strokes. It has greatly improved patient outcomes.
How the EVT Procedure Works in Detail
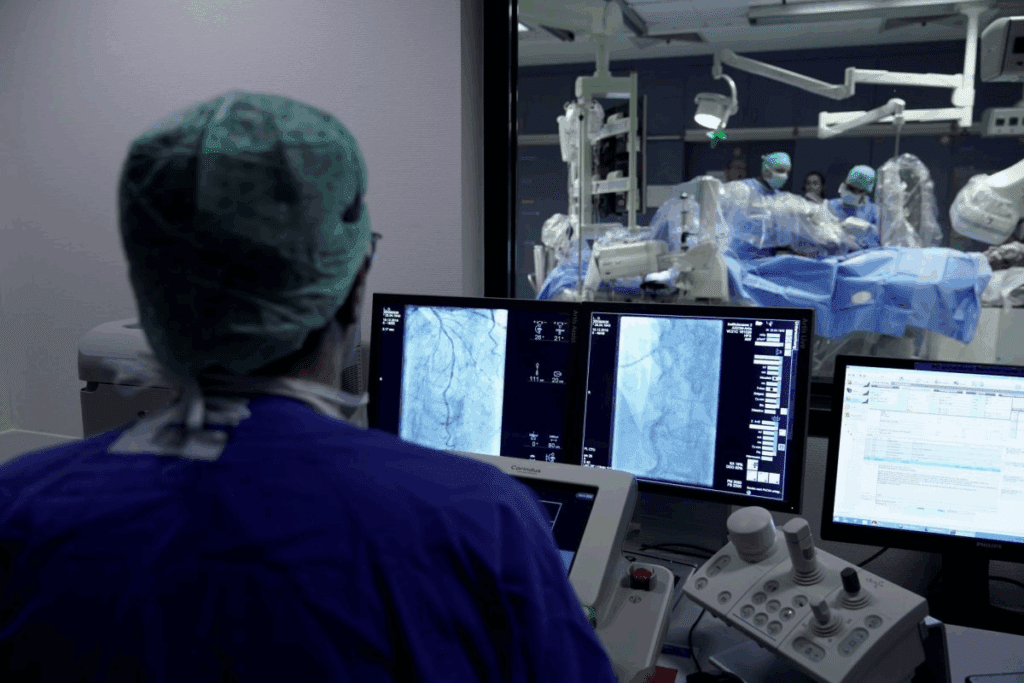
Endovascular thrombectomy (EVT) is a lifesaving procedure for acute ischemic stroke patients. It requires a skilled team and several key steps.
Patient Preparation and Anesthesia Considerations
Before starting the EVT procedure, patient preparation is key. We check the patient’s medical history and current condition. We also decide if they need general anesthesia or conscious sedation.
This ensures the patient is comfortable and doesn’t move during the procedure. It’s based on the patient’s health and the procedure’s complexity.
Catheter Insertion and Navigation to the Clot
The EVT procedure starts with a catheter in the femoral artery. It’s then guided through the vascular system to the brain clot. Advanced imaging techniques help find the clot.
This step is precise to avoid damaging blood vessels. It’s important to reach the clot effectively.
Clot Retrieval Techniques and Devices
When the catheter reaches the clot, clot retrieval devices are used. These devices, like stent retrievers, grab the clot and pull it out. The choice of device depends on the clot’s type and location.
We use the best technology to remove the clot successfully. The whole procedure, from start to finish, usually takes 1-2 hours. The quicker it is, the better the patient’s chances of recovery.
The Timeline for EVT Stroke Treatment
Knowing the timeline for EVT stroke treatment is key to better patient care. The success of endovascular thrombectomy (EVT) in treating stroke depends a lot on time.
We will look at the standard and extended treatment windows for EVT. We’ll talk about why quick action and choosing the right patients are so important.
Standard 6-8 Hour Treatment Window
The usual time for EVT in treating stroke is 6 to 8 hours after symptoms start. Early treatment in this time frame leads to better results and more successful treatments.
Research shows that those treated early have a better chance of getting back to normal.
Extended Treatment Windows up to 24 Hours
New imaging and clinical criteria have opened up a 24-hour window for EVT for some patients. This longer window is for those with brain tissue that can be saved, seen through advanced scans.
Guidelines say patients with a big gap between their symptoms and brain damage can get EVT up to 24 hours after symptoms start.More on choosing patients can be found in clinical guidelines.
The table below shows the main differences between the standard and extended treatment windows for EVT:
| Criteria | Standard Window (6-8 hours) | Extended Window (up to 24 hours) |
| Time from Symptom Onset | 6-8 hours | Up to 24 hours |
| Patient Selection | Based on time and clinical assessment | Based on advanced imaging and clinical criteria |
| Imaging Requirements | Basic imaging (e.g., CT scan) | Advanced imaging (e.g., CT perfusion or MRI) |
By following these guidelines, healthcare teams can improve stroke treatment with EVT. This leads to better results for patients, no matter the treatment window.
Patient Selection Criteria for Cerebral Thrombectomy
To get the most from EVT, doctors must carefully pick who to treat. They look at many things to see if a patient is right for cerebral thrombectomy.
Clinical Assessment Factors
Choosing patients for EVT starts with a detailed look at their health. Doctors check the patient’s medical history, how bad their stroke symptoms are, and how long ago the symptoms started. They often use the National Institutes of Health Stroke Scale (NIHSS) to measure stroke severity.
By doing a deep dive into a patient’s health, doctors can find out who will likely do well with EVT. For example, someone with very bad stroke symptoms and a high NIHSS score might be a good candidate if other things check out.
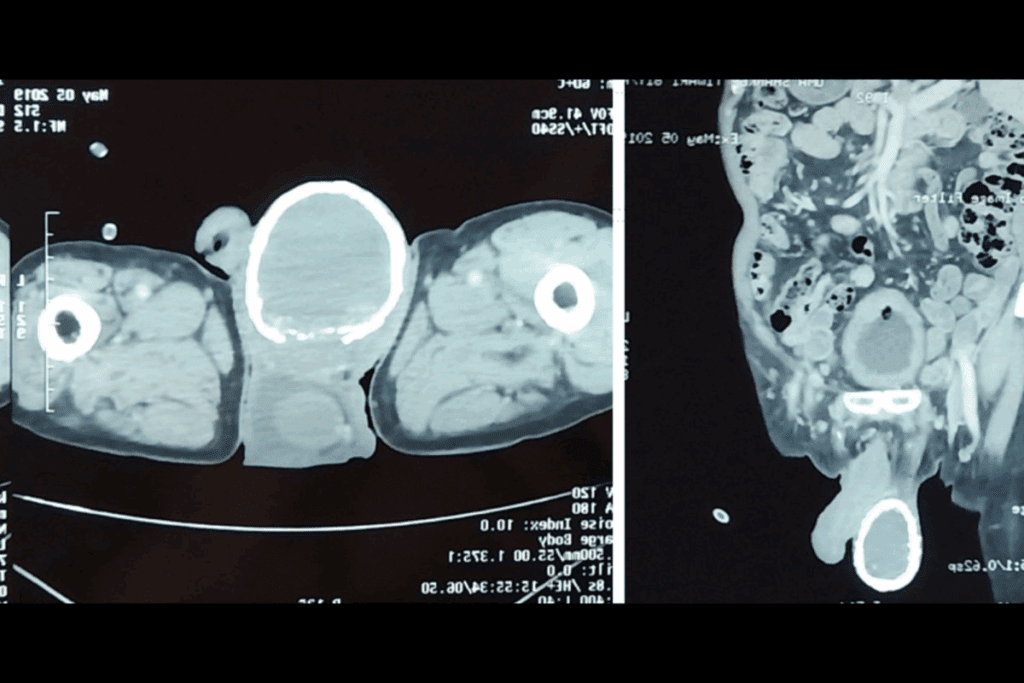
Imaging Requirements for EVT Candidacy
Imaging is key in deciding if someone can have EVT. Doctors use CT angiography (CTA) and MR angiography (MRA) to see the blocked blood vessel and how much brain tissue is at risk.
| Imaging Modality | Purpose |
| CT | Assess early ischemic changes |
| CTA | Identify occlusion site and collateral circulation |
| MRI | Evaluate infarct core and penumbra |
A recent study found that new imaging methods have changed how doctors pick patients for EVT. Now, they can spot who will really benefit from the treatment more accurately.
“The use of CTA and MRA has significantly improved our ability to select appropriate candidates for EVT, hereby improving patient outcomes.”
Contraindications and Exclusion Criteria
Not every patient is right for EVT. Doctors have to think about things that might make the treatment too risky. This includes serious health problems, bleeding risks, and severe brain damage. By carefully looking at these, doctors can make sure the treatment is safe and effective.
For instance, people with severe allergies to imaging contrast might not be good candidates. Also, those with bleeding disorders or who have had major surgery recently might not be considered.
In summary, picking patients for cerebral thrombectomy is a detailed process. It involves looking at the patient’s health, using imaging, and considering what might make the treatment too risky. By following these steps, doctors can make sure EVT is done safely and effectively.
Clinical Evidence Supporting EVT Effectiveness
Endovascular Thrombectomy (EVT) has been proven effective in treating acute ischemic stroke. Many landmark trials have shown its safety and success. They also found better patient outcomes than standard medical therapy alone.
Landmark Clinical Trials and Their Findings
Several key trials have looked into EVT’s effectiveness. Some notable ones include:
- MR CLEAN Trial: It was one of the first to show EVT’s benefits over standard care.
- EXTEND-IA Trial: Found EVT greatly improved outcomes for patients with large vessel occlusions.
- DAWN Trial: Showed EVT’s benefits even for late-presenting patients, with certain criteria.
These trials and others have shown EVT’s positive effects. They found better function, less disability, and more successful reperfusion.
Functional Outcome Improvements After EVT
EVT’s impact on function has been a major focus. Studies show EVT-treated patients are more likely to be functionally independent than those on standard care.
| Trial | Functional Independence Rate (EVT vs. Standard Care) |
| MR CLEAN | 32.6% vs. 19.1% |
| EXTEND-IA | 71% vs. 40% |
| DAWN | 49% vs. 13% |
Dr. Raul Nogueira said, “The DAWN trial showed EVT’s effectiveness even beyond traditional time windows. This is for carefully selected patients.”
“The evidence from these landmark trials has revolutionized acute ischemic stroke treatment. EVT plays a critical role in better patient outcomes.”
The evidence for EVT’s effectiveness is strong. It shows significant improvements in function for treated patients. As the field grows, we expect better patient selection and treatment methods.
Potential Risks and Complications of Thrombectomy for Stroke
EVT (Endovascular Thrombectomy) is a key treatment for stroke. Yet, it comes with risks. We must manage these complications to ensure the best care for our patients.
Procedural Complications
During EVT, several complications can happen. These include:
- Vascular complications, such as arterial dissection or perforation.
- Emboli to new territories, potentially causing further ischemic damage.
- Bleeding, either at the puncture site or intracranially.
Knowing these risks helps us prevent and prepare for them.
Post-Procedure Risks
After EVT, patients face several risks. These include:
- Re-occlusion of the treated artery.
- Hemorrhagic transformation of the infarct.
- Medical complications such as pneumonia or deep vein thrombosis.
Monitoring patients closely after the procedure is key to managing these risks.
Strategies to Minimize Complications
To lower EVT risks, we use several strategies:
- Careful patient selection based on clinical and imaging criteria.
- Advanced imaging techniques to guide the procedure and assess the clot.
- Post-procedure care in a specialized neuro-intensive care unit.
These strategies help reduce complications and improve patient outcomes.
In summary, while EVT is a vital stroke treatment, it carries risks. Understanding these risks and using strategies to minimize them ensures the best care for our patients.
EVT Medical Centers and Specialized Stroke Care
EVT medical centers are key in giving timely and effective stroke treatment. The success of EVT procedures depends on the center’s setup and the team’s skills.
We know that having a good stroke center is important. These centers have the latest technology and a team of experts ready to help.
Comprehensive Stroke Center Requirements
For stroke patients, certain requirements must be met by stroke centers. These include:
- Advanced imaging like CT and MRI
- A dedicated stroke team ready 24/7
- The ability to do EVT with precision
- Access to neuro-intensive care units for monitoring
Being able to work together across different areas is key. This teamwork is vital for the best patient results.
| Requirement | Description | Importance |
| Advanced Imaging | CT and MRI for accurate diagnosis | High |
| Dedicated Stroke Team | Available 24/7 for timely intervention | High |
| EVT Capability | Precision in performing EVT procedures | High |
| Neuro-ICU | Post-procedure monitoring and care | High |
The Stroke Team: Specialists Involved in EVT
The stroke team is a group of experts working together. They include:
- Interventional neuroradiologists
- Stroke neurologists
- Neurosurgeons
- Nurses and technicians specialized in stroke care
The role of each specialist is critical in the care of stroke patients. Their combined knowledge ensures patients get the best care.
Understanding the needs of EVT centers and the team involved shows the complexity of stroke care. The role of skilled teams in stroke centers is essential for better patient outcomes.
Recovery and Rehabilitation After EVT
The journey to recovery after EVT is complex. It involves immediate care and long-term rehabilitation. Knowing this process helps patients and their families navigate the post-stroke path.
Immediate Post-Procedure Monitoring
Patients are watched closely in a stroke unit or intensive care after EVT. This early care is key to spotting and handling any issues quickly. Close monitoring includes checking the brain, managing blood pressure, and watching for bleeding or other problems.
This initial phase is vital. It lays the groundwork for recovery. Good monitoring can greatly improve outcomes by catching and treating problems early.
Rehabilitation Process and Timeline
Rehab after EVT is customized for each patient. It starts 24 to 48 hours after the procedure, when the patient is stable. A team of therapists creates a plan tailored to the patient’s needs.
This plan includes various therapies to help regain lost abilities, improve mobility, and enhance life quality. The length of rehabilitation can range from weeks to months, based on the stroke’s severity and the patient’s response to therapy.
Long-Term Outcomes and Quality of Life
Long-term results after EVT are often positive, with many patients seeing big improvements. The level of recovery varies, but EVT often leads to better outcomes than standard treatments alone.
For example, Pete Wilkins’ story shows how much improvement is possible with minimal lasting effects. The speed of EVT treatment, the stroke’s initial severity, and the patient’s health all play roles in long-term outcomes.
With a focus on thorough rehabilitation and support, we can improve the lives of stroke survivors. This helps them regain independence and return to their daily routines.
Conclusion: The Evolving Role of EVT in Modern Stroke Care
The introduction of EVT in stroke care has changed how we treat strokes. EVT has become a key treatment for many patients. As it keeps getting better, we see even more positive results for patients.
In places like Newfoundland and Labrador, more EVT services are being added. This shows how important EVT is becoming in treating strokes. It’s a big step towards better stroke care and results.
Looking ahead, making EVT even better is key. We expect EVT to play an even bigger role in stroke care. This will lead to better lives for those affected by strokes.
FAQ
What does EVT stand for in medical terms?
EVT stands for Endovascular Thrombectomy. It’s a procedure to treat acute ischemic stroke. It removes blood clots from the brain.
What is EVT medical abbreviation used for?
The EVT medical abbreviation stands for Endovascular Thrombectomy. It’s a key treatment for acute ischemic stroke. It uses a catheter to remove blood clots.
How does the EVT procedure work?
The EVT procedure starts with a catheter in the affected artery. It’s guided to the clot. Then, devices remove the clot, improving blood flow to the brain.
What is the typical timeline for EVT stroke treatment?
EVT is usually done within 6-8 hours after a stroke. But, it can go up to 24 hours for some patients.
What are the criteria for patient selection for EVT?
Choosing patients for EVT involves clinical checks and imaging. It makes sure patients will likely benefit from the treatment.
What are the risks and complications of thrombectomy for stroke?
Risks of EVT include complications like vessel damage. Post-procedure, there’s a chance of clot return or bleeding. These risks are lower with careful patient choice and skilled doctors.
What is the role of stroke centers in EVT?
Stroke centers are key for EVT. They have the right setup, team, and skills. This ensures the procedure and care after it are successful.
What is the recovery and rehabilitation process like after EVT?
After EVT, patients are closely watched. Then, a personalized rehab plan is made. It aims to improve function and quality of life.
How has EVT evolved as a treatment for stroke?
EVT has grown as a top stroke treatment. Studies show it improves outcomes. It keeps getting better with new tech and methods.
What are the benefits of EVT in stroke care?
EVT can greatly improve stroke outcomes. It reduces disability and boosts quality of life for stroke patients.
How long does a thrombectomy procedure take?
EVT procedures last from 30 minutes to a few hours. It depends on the case’s complexity and the team’s skill.
What is cerebral thrombectomy?
Cerebral thrombectomy is removing a brain artery clot. It’s a key part of EVT for treating acute ischemic stroke.
What is thrombectomy for stroke?
Thrombectomy for stroke, or EVT, is a treatment to remove a clot in acute ischemic stroke. It aims to restore blood flow to the brain.
References
- Saver, J. L., Goyal, M., van der Lugt, A., Menon, B. K., Majoie, C. B., Dippel, D. W., Campbell, B. C., Nogueira, R. G., Demchuk, A. M., Tomasello, A., Cardona, P., Devlin, T. G., Frei, D. F., du Mesnil de Rochemont, R., Berkhemer, O. A., Jovin, T. G., Siddiqui, A. H., van Zwam, W. H., Davis, S. M., … HERMES Collaborators. (2016). Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA, *316*(12), 1279-1288. https://pubmed.ncbi.nlm.nih.gov/27673305/


































