Many people with back pain find that traditional treatments don’t last. But new medical tech like radiofrequency ablation (RFA) is making a big difference. It’s changing how we manage pain.
At Liv Hospital, we use RFA (Radiofrequency Ablation) and other advanced methods to help patients. This technique is non-invasive and uses electrical currents to stop pain signals from the spine. Ablation for back pain offers significant relief for those struggling with chronic discomfort, providing a safe and effective alternative to surgery.
Key Takeaways
- RFA is a minimally invasive procedure that targets nerves transmitting pain signals.
- It uses high-frequency electrical currents to disable these nerves.
- RFA offers a promising solution for individuals seeking lasting back pain relief.
- The procedure is part of the advanced treatments available at Liv Hospital.
- Our approach combines expertise with a patient-centered care philosophy.
Understanding Ablation for Back Pain
Ablation for back pain stops pain signals. It’s an option for those who want relief beyond usual treatments. It involves destroying nerve tissues that send pain signals to the brain.
Definition and Purpose of Nerve Ablation
Nerve ablation is a medical procedure to help with chronic pain. It aims to stop pain signals from reaching the brain. This is for people with back pain that hasn’t gotten better with usual treatments.
The method uses different ways to harm or kill the nerves that carry pain. This goal is to lessen or stop the pain a person feels.
Types of Ablation Techniques for Spinal Pain
There are many ablation techniques for spinal pain, including:
- Radiofrequency Ablation (RFA): This common method uses electrical currents to heat up nerves. This heats them up, stopping pain signals.
- Chemical Ablation: It uses chemicals to damage or destroy nerves.
- Cryoablation: This uses cold to freeze nerves, stopping their function.
Each method has its own use and benefits. The choice depends on the patient’s condition and the doctor’s skills.
History and Development of Ablation Procedures
Ablation procedures started in the early 20th century for pain treatment. Over time, they’ve improved a lot. This is thanks to new technology and understanding pain better.
The 1960s saw a big step with radiofrequency ablation. It made treating pain more precise and safe. Ever after, more research and tech advancements have made these procedures even better and safer for patients.
The Science Behind Radiofrequency Ablation
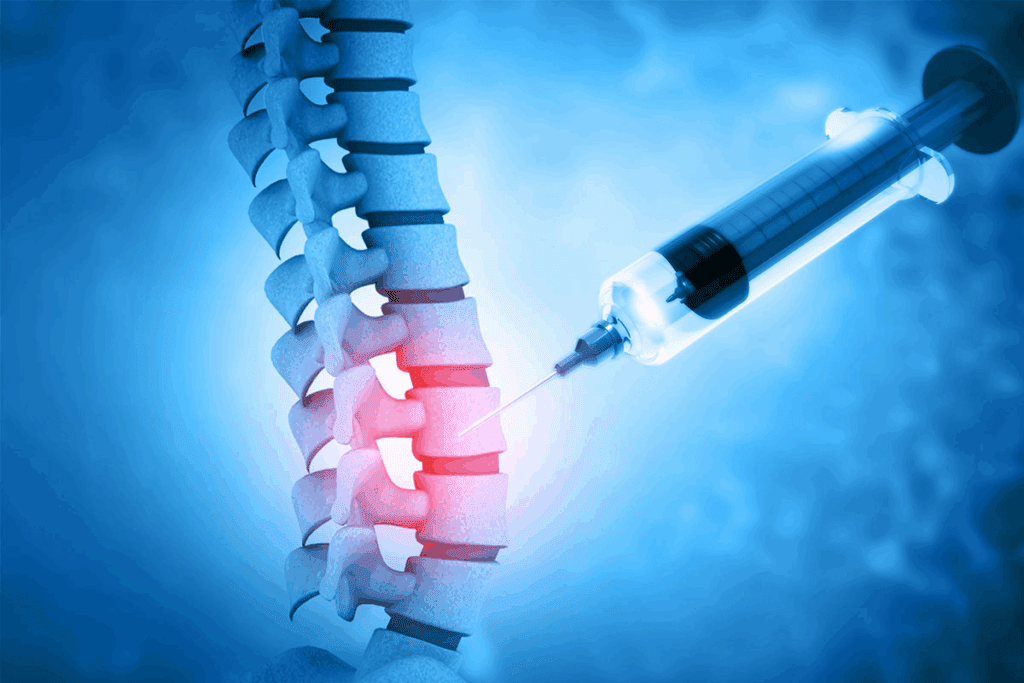
Radiofrequency ablation works by targeting nerves that carry pain signals. This method is a big change in treating chronic pain. It helps those who haven’t found relief with other treatments.
How High-Frequency Electrical Currents Target Nerves
Radiofrequency ablation uses high-frequency electrical currents to heat up nerves. This creates a lesion that stops pain signals. A special device sends radiofrequency energy to the pain-causing nerve.
The heat damages the nerve, cutting off pain signals to the brain. This is how RFA works.
RFA is precise because it uses imaging like fluoroscopy or ultrasound. This helps doctors place the device exactly where it’s needed. It reduces the chance of harming nearby tissues.
The Neurological Mechanism of Pain Signal Disruption
RFA’s success comes from stopping pain signals at their source. When a nerve is damaged, it can’t send pain signals anymore. This reduces or stops pain feeling.
The effects of RFA on pain pathways can last a long time. It gives patients a lot of relief from chronic pain. But, it’s not a cure for the pain’s cause. It’s a way to manage pain and improve life quality.
Difference Between Ablation and Other Pain Management Techniques
RFA is different from other pain treatments. It directly targets pain sources, unlike medicines that can have side effects. It’s also less invasive than surgery, with a shorter recovery time.
Key differences between RFA and other pain management techniques include:
- Minimally invasive: RFA uses small incisions, lowering complication risks.
- Targeted approach: RFA goes straight to the pain-carrying nerves.
- Long-lasting relief: RFA’s effects can last months to years, depending on the case.
Knowing how RFA works and how it compares to other treatments helps patients and doctors. They can better understand its benefits and limits.
Common Back Conditions Treated with Ablation
Many back conditions can be managed with ablation therapy. Radiofrequency ablation (RFA) is a key treatment for chronic back pain. We’ll look at the back conditions that benefit from this method.
Facet Joint Syndrome and Medial Branch Nerves
Facet joint syndrome causes chronic back pain. It happens when the facet joints in the spine degenerate or get injured. The medial branch nerves, which supply these joints, are often treated with RFA to ease pain.
Research shows RFA can greatly reduce pain and improve function in facet joint syndrome patients. By blocking pain signals from the medial branch nerves, ablation offers long-term pain relief.
Sacroiliac Joint Pain and Lateral Branch Nerves
Sacroiliac joint pain is another condition that blation can treat. The lateral branch nerves, which carry pain signals from the sacroiliac joint, are the main focus in RFA procedures.
Patients with sacroiliac joint dysfunction often feel pain in their lower back and buttocks. This pain can spread down the leg. Ablating the lateral branch nerves can significantly lessen or stop this pain, boosting the patient’s quality of life.
Degenerative Disc Disease and Neuropathic Pain
Degenerative disc disease can lead to chronic back pain and neuropathic symptoms. RFA doesn’t fix the disc degeneration itself. But it can target nerves that send pain signals from the affected area.
This approach can offer significant relief for those who haven’t found help with other treatments. It’s a less invasive option compared to surgery.
Spinal Arthritis and Chronic Back Pain
Spinal arthritis, like osteoarthritis and ankylosing spondylitis, can cause chronic back pain. Ablation can manage the pain from these conditions, mainly when other treatments haven’t worked.
By focusing on the nerves involved in pain transmission, RFA can lessen the pain and discomfort of spinal arthritis. This improves the patient’s function and overall quality of life.
The following table summarizes the common back conditions treated with ablation and their associated outcomes:
| Condition | Nerves Targeted | Typical Outcome |
| Facet Joint Syndrome | Medial Branch Nerves | Significant pain reduction |
| Sacroiliac Joint Pain | Lateral Branch Nerves | Improved function and reduced pain |
| Degenerative Disc Disease | Nerves associated with affected discs | Relief from neuropathic pain |
| Spinal Arthritis | Various nerves depending on the affected area | Reduced pain and improved quality of life |
The Ablation for Back Pain Procedure: What to Expect
Knowing what to expect during ablation for back pain can make you feel less anxious. We aim to guide you through every step. This way, you can feel more prepared and comfortable.
Pre-Procedure Diagnostic Testing and Evaluation
We do thorough tests before starting the procedure. This includes X-rays, CT scans, or an MRI to see the pain area. We also do diagnostic injections to confirm the pain source.
Diagnostic testing is key. It helps us tailor the treatment to your specific needs. This makes the treatment more effective.
Step-by-Step Breakdown of the RFA Procedure
The RFA procedure has several steps:
- Preparation: We make sure you’re comfortable on an X-ray table.
- Needle Placement: We use X-ray guidance to place a small needle near the nerve.
- Electrode Insertion: A special electrode is inserted through the needle to send radiofrequency energy.
- Ablation: The energy heats the nerve, stopping it from sending pain signals.
This precise method helps avoid damage to other tissues. This means you can recover faster.
Technology and Equipment Used During Ablation
We use the latest technology and equipment for the RFA procedure. This includes:
- Fluoroscopy: Gives us real-time X-ray images for needle placement.
- Radiofrequency Generator: Sends the right amount of energy for the treatment.
- Specialized Electrodes: Designed for the best energy delivery and less tissue damage.
Advanced technology makes the RFA procedure more precise and effective. This leads to better results for patients.
Typical Duration and Setting of the Procedure
The RFA procedure usually lasts 30 to 60 minutes. It’s often done on an outpatient basis. This means you can go home the same day. We watch over you for a bit after to make sure you’re okay.
Knowing about the ablation for back pain procedure can help ease your worries. Our team is here to provide full care and support every step of the way.
Duration of Pain Relief After Ablation
Knowing how long RFA pain relief lasts is key. Radiofrequency ablation is a big help for chronic back pain. It brings relief to many.
Average Timeframes for Pain Relief Benefits
Pain relief from RFA can last 6 to 12 months, sometimes more. The time varies based on the condition and the patient’s health.
For example, those with facet joint syndrome might feel better for 9 to 12 months. Those with sacroiliac joint pain might see relief for a bit less time.
Factors Affecting How Long RFA Results Last
Many things can change how long RFA relief lasts. These include:
- The condition being treated
- The success of the RFA procedure
- The patient’s health and lifestyle
- Other chronic pain conditions
For instance, degenerative disc disease might lead to shorter relief times. This is because the condition gets worse over time.
Clinical Studies on Long-Term Effectiveness
Many studies have looked at RFA’s long-term effects. A study in the Journal of Pain Research found relief for up to 12 months in chronic lower back pain patients.
| Study | Sample Size | Average Relief Duration |
| Journal of Pain Research | 100 | 12 months |
| Pain Medicine | 150 | 9 months |
| European Spine Journal | 80 | 11 months |
When and Why Relief Eventually Diminishes
RFA pain relief isn’t permanent. It can fade over time. This might happen because nerves grow back or the condition gets worse. Sometimes, patients need more RFA to keep feeling better.
Managing chronic back pain is a long-term effort. Knowing what affects RFA’s success and how long it lasts helps patients choose the best treatments.
Recovery and Post-Procedure Care
After Radiofrequency Ablation, it’s key to stick to a care plan. This ensures the best results. The recovery time is as important as the procedure itself.
Immediate Post-Procedure Experience
Right after RFA, you might feel some soreness. This is usually mild and short-lived. Rest for the day and avoid hard activities.
- Watch your temperature and tell your doctor if it’s high.
- Look out for signs of infection, like redness or swelling at the site.
- Follow your doctor’s advice on wound care.
Timeline for Return to Normal Activities
You can usually get back to normal in a few days. But listen to your doctor’s advice. Everyone recovers at their own pace.
Typical Recovery Timeline:
- First 24 hours: Rest and avoid heavy lifting, bending, or strenuous activities.
- 2-3 days: Start doing normal things again as you feel comfortable.
- 1-2 weeks: Most people are fully recovered and can do everything they want.
Pain Management During Recovery
It’s important to manage pain during recovery. We might suggest pain relievers or other meds to help.
Always take your meds as your doctor tells you to.
Follow-Up Care and Monitoring
Follow-up care is vital. We check on you to see how you’re doing and adjust your treatment if needed.
Key aspects of follow-up care include:
- Checking if the RFA worked.
- Handling any side effects or problems.
- Helping with long-term pain management.
Potential Risks, Side Effects, and Complications
When we talk about RFA for back pain, we must also discuss the risks and side effects. RFA is generally safe, but knowing the possible side effects is key. This knowledge helps patients make informed choices about their treatment.
Common Temporary Side Effects
After RFA, many people feel some temporary side effects. These can include:
- Temporary discomfort or pain at the procedure site
- Bruising or swelling around the treated area
- Numbness or altered sensation in the affected region
These effects are usually mild and go away within a few days to a week.
Rare but Serious Complications
Though rare, serious complications can happen with RFA. These include:
- Infection at the procedure site
- Nerve damage resulting in persistent numbness or weakness
- Allergic reactions to the materials used during the procedure
It’s important for patients to know about these risks. They should talk to their healthcare provider about any worries.
Risk Factors That May Increase Complications
Some factors can make complications from RFA more likely. These include:
| Risk Factor | Potential Complication |
| Diabetes | Increased risk of infection |
| Previous history of allergic reactions | Allergic reaction to materials used in RFA |
| Poor overall health | Slower recovery and increased risk of complications |
How Physicians Minimize Procedure Risks
Healthcare providers take steps to reduce RFA risks. They:
- Do a thorough check before the procedure to spot risk factors
- Use clean techniques to lower infection risk
- Use precise imaging to place the RFA device correctly
- Watch closely during and after the procedure to catch any issues fast
By understanding the risks and how to lessen them, patients can make better choices. This helps them get the most from RFA for back pain relief.
Patient Experiences and Success Rates
Many studies show that Radiofrequency Ablation (RFA) is a top choice for chronic back pain. It helps a lot of people feel better. Let’s look at what makes RFA work well for patients.
Statistical Overview of Patient Satisfaction
About 80% of patients see big improvements in pain after RFA. A study in the Journal of Pain Research showed RFA boosts pain scores and function in chronic low back pain patients. This success rate makes RFA a strong option for chronic back pain.
Real-World Radiofrequency Ablation for Back Pain Reviews
Real stories and reviews back up RFA’s success. People say they feel less pain and live better lives. For example, a Pain Management Association survey found 75% of patients moved better and felt less pain after RFA.
- Improved pain management
- Enhanced quality of life
- Increased mobility
Predictors of Successful Outcomes
While RFA works well, some things can make it even better. These include:
- Accurate diagnosis of the pain source
- Proper patient selection
- Technical skill of the practitioner
Healthcare providers can make RFA more likely to succeed by focusing on these areas.
Managing Expectations About Results
It’s key for patients to know what to expect from RFA. While many feel a lot of relief, results can differ. Things like the pain’s cause, health, and past treatments affect RFA’s success. Talking with a doctor about what to expect helps set realistic hopes.
Knowing about RFA’s success helps people choose their treatments wisely. Always talk to a doctor to find the best treatment for you.
Conclusion: Is Ablation Right for Your Back Pain?
Radiofrequency ablation (RFA) is a good option for many with chronic back pain. The choice to get RFA depends on your pain level, past treatments, and health.
Thinking about RFA for back pain? It’s key to know the good and bad sides. RFA can help a lot with certain back problems, like facet joint syndrome or sacroiliac joint pain.
Wondering if RFA is for you? Look at your back pain treatment options and talk to a doctor. They can guide you based on your specific needs and health history.
Whether RFA is right for you depends on many things. This includes the cause of your back pain and your health. Knowing about RFA and its effects can help you decide if it’s the best choice for your back pain treatment.
FAQ
What is radiofrequency ablation (RFA) for back pain?
Radiofrequency ablation (RFA) is a procedure that uses heat to treat back pain. It targets nerves that send pain signals to the brain. This helps relieve chronic back pain.
How long does radiofrequency ablation last for back pain?
RFA can offer pain relief for 6 to 12 months. Some people may feel relief for up to 2 years or more.
What are the common back conditions treated with RFA?
RFA treats many back conditions. These include facet joint syndrome, sacroiliac joint pain, and degenerative disc disease. It also helps with spinal arthritis and other chronic back pain.
How is RFA different from other pain management techniques?
RFA is unique because it directly targets pain nerves. This provides longer-lasting relief compared to other methods like steroid injections or medication.
What can I expect during the RFA procedure?
During RFA, you’ll undergo tests and get local anesthesia. A special needle is inserted near the nerves. Then, radiofrequency energy heats and disrupts the nerves.
Are there any potential risks or side effects associated with RFA?
Yes, RFA can have risks and side effects. These include temporary pain, swelling, or bruising. Rare but serious complications like infection or nerve damage can also occur.
How long does it take to recover from RFA?
Recovery from RFA is usually quick. Most people can go back to normal activities within a few days to a week. It’s important to follow the post-procedure care instructions.
Will I need follow-up care after RFA?
Yes, follow-up care is essential after RFA. It helps monitor the procedure’s success, manage side effects, and decide if more treatments are needed.
Can RFA be repeated if pain returns?
Yes, RFA can be repeated if pain comes back. The nerves can grow back, and the procedure can be safely done again.
How effective is RFA in managing chronic back pain?
RFA is effective in managing chronic back pain. Many patients experience significant pain relief. But results can vary from person to person.
References
- Abd-Elsayed, A. (2020). The Long-Term Efficacy of Radiofrequency Ablation With Image-Guided Lesioning for Chronic Low Back Pain: A Review. Pain Medicine, 21(7), 1295–1301. https://pmc.ncbi.nlm.nih.gov/articles/PMC7901125/