Athletes often do a lot of hard training. This can affect their heart health. It makes people wonder if abnormal ECG findings are normal for them.
Studies show that hard training can change the heart’s shape and how it works. This can lead to ecg abnormalities that non-athletes don’t usually get.
We’ll look at how exercise affects heart health and EKG readings. We’ll see how different workouts can change ecg findings.
Key Takeaways
- Athletes may show different EKG patterns because of their intense training.
- Certain abnormal heart rhythms are more common in athletes.
- It’s important to understand the context of EKG readings to interpret them correctly.
- Not all ecg abnormalities in athletes mean there’s a health problem.
- Heart health and the type of athletic training are key to what’s normal.
Understanding the Basics of Electrocardiograms (ECGs/EKGs)

The electrocardiogram (ECG) is a key test for checking the heart’s electrical activity. It gives important details about the heart’s rhythm, rate, and function.
What is an ECG and how does it work?

An ECG records the heart’s electrical signals as it beats. Electrodes on the skin, like on the chest, arms, and legs, detect these signals. The ECG machine then shows these signals on a graph, giving a visual of the heart’s electrical activity.
To do this, electrodes are placed on the skin to pick up the heart’s electrical signals. These signals are then shown on a screen or paper, showing the heartbeat’s phases.
Normal ECG patterns and measurements
A normal ECG tracing has a steady heart rate and rhythm. It includes the P wave, QRS complex, and T wave. Each part tells us something about the heart’s electrical activity.
Normal ECG measurements are:
- Heart rate: 60-100 beats per minute
- PR interval: 120-200 milliseconds
- QRS duration: Less than 120 milliseconds
- QT interval: Varies with heart rate, but generally less than 440 milliseconds
|
ECG Component |
Normal Measurement |
Clinical Significance |
|---|---|---|
|
P Wave |
<120 ms |
Atrial depolarization |
|
QRS Complex |
<120 ms |
Ventricular depolarization |
|
T Wave |
Variable |
Ventricular repolarization |
The purpose of ECG testing in clinical settings
ECG testing is a key tool in many clinical settings. It helps spot arrhythmias, detect heart problems, and see how medicines affect the heart. It’s also used in exercise tests to check for heart disease.
In medical practice, ECGs are key for watching over patients with heart issues. They’re also used to screen people at risk of heart problems. The info from an ECG helps doctors make treatment plans and catch heart issues early.
The Athlete’s Heart: Physiological Adaptations
Athletic training changes the heart, known as cardiac remodeling. This change is key for athletes. It lets their hearts handle more physical activity.
Cardiac remodeling happens when the heart works hard during exercise. It makes the heart pump blood better. We’ll see how different sports affect these changes.
Cardiac Remodeling in Response to Exercise
Exercise makes the heart grow and work better. It gets bigger, thicker, and pumps more blood. These changes are good and show the heart is strong.
Differences Between Endurance and Strength Athletes
Endurance athletes, like runners and cyclists, have different heart changes than strength athletes, like weightlifters. Endurance training makes the heart bigger, improving how it pumps blood. Strength training makes the heart walls thicker.
How Athletic Training Affects Heart Structure and Function
Exercise changes the heart’s structure and function. It makes the heart pump better, relaxes blood vessels, and works more efficiently. Knowing these changes helps doctors understand athlete’s hearts.
Doctors can tell athletes’ hearts apart by looking at their ECGs. This helps them give the right care to athletes.
Common ECG Changes in Athletes
Athletes’ hearts change in ways that show up on an ECG. These changes include heart rate and rhythm shifts. They happen because of regular exercise and can sometimes look like sickness.
Sinus Bradycardia and Arrhythmia
Sinus bradycardia is common in athletes. It means their heart beats slower than 60 times a minute. This is because their heart gets better at handling exercise.
Arrhythmias, or irregular heartbeats, also show up in athletes. These can be simple or complex. It’s important to tell the difference between harmless and serious heart issues.
Early Repolarization Patterns
Early repolarization is seen in athletes’ ECGs. It looks like a bump at the start of the ST segment. This is usually okay and comes from the heart’s response to exercise. But, it’s key to tell it apart from serious problems like Brugada syndrome.
Left Ventricular Hypertrophy
Strength training athletes might have left ventricular hypertrophy (LVH) on their ECG. LVH means the left ventricle gets thicker. In athletes, this is usually okay. But, in others, it can be a sign of heart disease.
|
ECG Change |
Description |
Clinical Significance |
|---|---|---|
|
Sinus Bradycardia |
Resting heart rate |
Generally benign, related to increased vagal tone |
|
Early Repolarization |
J-point elevation, ST segment elevation |
Benign, but must be distinguished from Brugada syndrome |
|
Left Ventricular Hypertrophy |
Thickening of left ventricle walls |
Often a benign adaptation in athletes, but requires evaluation |
Knowing about these ECG changes in athletes is important. It helps athletes and doctors tell the difference between normal changes and serious problems. This way, they can avoid unnecessary worry or treatment.
Abnormal ECG Examples in Athletes
ECG abnormalities in athletes can cause worry. They need a detailed check to see if they’re serious. It’s hard to tell if they’re just normal changes or something more serious.
Benign vs. Pathological Findings
When looking at ECG results for athletes, it’s key to know the difference. Some changes are normal because of exercise. But others might mean there’s a problem that needs more looking into.
- Benign findings often include sinus bradycardia, early repolarization, and increased QRS voltage.
- Pathological findings may involve T-wave inversion, ST-segment depression, and certain arrhythmias.
Visual Examples of Athlete-Specific ECG Patterns
Looking closely at ECG tracings helps spot patterns unique to athletes. For example, the early repolarization pattern is common in athletes. It’s usually not a cause for worry.
Interpretation Challenges for Medical Professionals
Doctors have a tough time figuring out ECGs for athletes. It’s hard to tell the difference between normal changes and real problems. They need to know the athlete’s ECG patterns well and be able to spot serious issues.
- Careful analysis of the ECG tracing to identify subtle abnormalities.
- Consideration of the athlete’s medical history and clinical context.
- Use of additional diagnostic tests when necessary to clarify the significance of ECG findings.
Distinguishing Normal Athletic Adaptations from Pathology
Understanding ECG results in athletes is complex. It involves knowing both normal heart changes and signs of disease. The heart changes in many ways when someone exercises regularly. Some of these changes might look bad on an ECG.
The Gray Zone Between Adaptation and Disease
One big challenge is finding ECG results that are hard to read. These results can be in a gray area between normal and possibly serious. This makes it hard for doctors to know what to do.
Key factors help tell normal changes from disease. These include the athlete’s health, the ECG patterns, and any symptoms or family history.
Key Differentiating Factors
Several things help tell normal heart changes from disease on an ECG:
- Symptom history and physical examination findings
- Family history of cardiac conditions
- The specific nature of the ECG abnormalities
- Results from additional diagnostic tests when necessary
When to Be Concerned About an Athlete’s ECG
Some ECG findings need more checking. Look out for big T-wave inversion or ST-segment depression. These signs mean you should act fast.
By looking at these factors and keeping up with new guidelines, we can better tell normal heart changes from disease on ECGs.
International Criteria for ECG Interpretation in Athletes
Interpreting electrocardiograms (ECGs) in athletes is key to heart health checks. It needs clear, worldwide rules. These rules help spot real heart problems from normal changes from exercise.
Evolution of Athlete-Specific ECG Criteria
Athletes often show ECG patterns not seen in regular people. Early rules were too wide, causing many false alarms. Thanks to new research, these rules have gotten better.
Research found that some ECG signs once thought bad are actually common in athletes. For example, slow heart rates and early repolarization are seen in many endurance athletes. So, the rules have changed to better tell the difference between safe and unsafe signs.
The Seattle Criteria and Its Updates
The Seattle Criteria, from 2013, was a big step in ECG reading for athletes. It divided ECG signs into “common and training-related” and “uncommon and training-unrelated.” Later updates have made these rules even better.
International Consensus Guidelines
Leading cardiology groups have come together to make global ECG reading rules. These rules help doctors understand ECGs the same way everywhere. They also consider things like age, gender, and race.
|
Guideline |
Key Features |
Application |
|---|---|---|
|
Seattle Criteria |
Nuanced classification of ECG findings |
Athlete screening programs |
|
International Consensus Guidelines |
Standardized interpretation across demographics |
Global application in sports cardiology |
Using these global rules helps doctors get better at reading ECGs in athletes. This means fewer false alarms and better care for athletes with real heart issues.
Sport-Specific ECG Findings
Athletes in different sports show unique ECG patterns. This is because their sports have special demands. These demands shape their heart health, which shows up in their ECGs.
Endurance Sports
Endurance sports like cycling, running, and swimming require long periods of aerobic exercise. This leads to heart changes, such as a bigger left ventricle and better vagal tone. As a result, endurance athletes often have:
- Sinus bradycardia: A slower heart rate at rest due to increased vagal tone.
- Early repolarization: A common finding that can sometimes be misinterpreted as a pathological condition.
- Voltage criteria for left ventricular hypertrophy: Reflecting the increased muscle mass of the heart.
Strength and Power Sports
Strength and power sports, like weightlifting and sprinting, have different heart adaptations. Their training makes the heart walls thicker but not the chambers. ECGs of these athletes may show:
- Left ventricular hypertrophy: Indicated by increased QRS voltages.
- Repolarization abnormalities: Sometimes seen in conjunction with hypertrophy.
Team and Mixed Discipline Sports
Team sports and mixed disciplines, like soccer, basketball, and rugby, mix endurance and strength. Their ECGs reflect this mix. Common findings include:
- Mixed ECG patterns: Combining elements seen in both endurance and strength athletes.
- Normal or mildly abnormal ECGs: As the cardiac adaptations may not be as pronounced as in single-discipline sports.
It’s key to understand these ECG patterns for athletes’ heart health. This helps tell real heart changes from possible problems. Knowing these patterns helps doctors give better care to athletes.
Demographic Factors Affecting Athletic ECG Patterns
When looking at ECG patterns in athletes, we must think about different factors. Things like age, gender, and ethnicity can really change what we see on an ECG.
Age-related Considerations
Age is very important when it comes to ECGs in athletes. As athletes get older, their hearts change in ways that show up on ECGs.
Young athletes often have a faster heart rate because of their nervous system. Older athletes might show signs of heart changes from years of hard training.
|
Age Group |
Common ECG Findings |
|---|---|
|
Young Athletes (<20 years) |
Sinus bradycardia, high vagal tone |
|
Adult Athletes (20-40 years) |
Left ventricular hypertrophy, early repolarization |
|
Older Athletes (>40 years) |
More pronounced cardiac remodeling, possible conduction issues |
Gender Differences
Gender also affects ECG patterns in athletes. Research shows that female athletes have different ECG readings than males.
For example, female athletes are less likely to show signs of heart thickening on their ECGs. It’s important to understand these differences to read ECGs correctly.
Ethnicity and Genetic Factors
Ethnicity and genetics also play a part in ECG patterns. Some ethnic groups might have more common ECG patterns due to their genes.
For instance, athletes from African backgrounds might have ECG patterns that are normal for them but could raise concerns in others.
By taking these factors into account, doctors can better understand ECGs in athletes. This helps avoid wrong diagnoses and ensures athletes get the right care.
Potentially Dangerous ECG Abnormalities in Athletes
ECG testing is key for spotting serious heart issues in athletes. Many athletes have normal or harmless ECG patterns. But, some patterns can show a higher risk of heart problems.
Abnormalities like T-wave inversion and ST-segment depression are concerning. They might point to heart diseases like coronary artery disease or cardiomyopathy. T-wave inversion is very worrying if it’s deep and even, often seen in hypertrophic cardiomyopathy.
T-wave Inversion and ST-Segment Depression
T-wave inversion and ST-segment depression are serious because they can mean heart ischemia or serious heart issues. ST-segment depression is linked to coronary artery disease, but can also show up in other conditions.
- T-wave inversion can be a sign of cardiomyopathy or other heart diseases.
- ST-segment depression may show ischemia or other heart problems.
Conduction Abnormalities and Heart Blocks
Conduction problems, like different heart blocks, are also a worry in athletes. These issues affect the heart’s electrical system, leading to arrhythmias or worse heart problems.
Some important points to remember:
- First-degree heart block is usually okay, but higher degrees need more checking.
- Bundle branch blocks might mean there’s a structural heart disease.
Ventricular Pre-excitation and Long QT Syndrome
Ventricular pre-excitation, like in Wolff-Parkinson-White (WPW) syndrome, and long QT syndrome raise the risk of dangerous arrhythmias in athletes.
“The presence of WPW syndrome or long QT syndrome on an ECG can have significant implications for an athlete’s participation in sports and their overall risk of sudden cardiac death.” –
A leading cardiologist
Athletes with these conditions need a cardiologist’s check-up. This is to figure out the right steps and talk about any activity limits.
Knowing and spotting these dangerous ECG patterns helps doctors protect athletes’ health and safety.
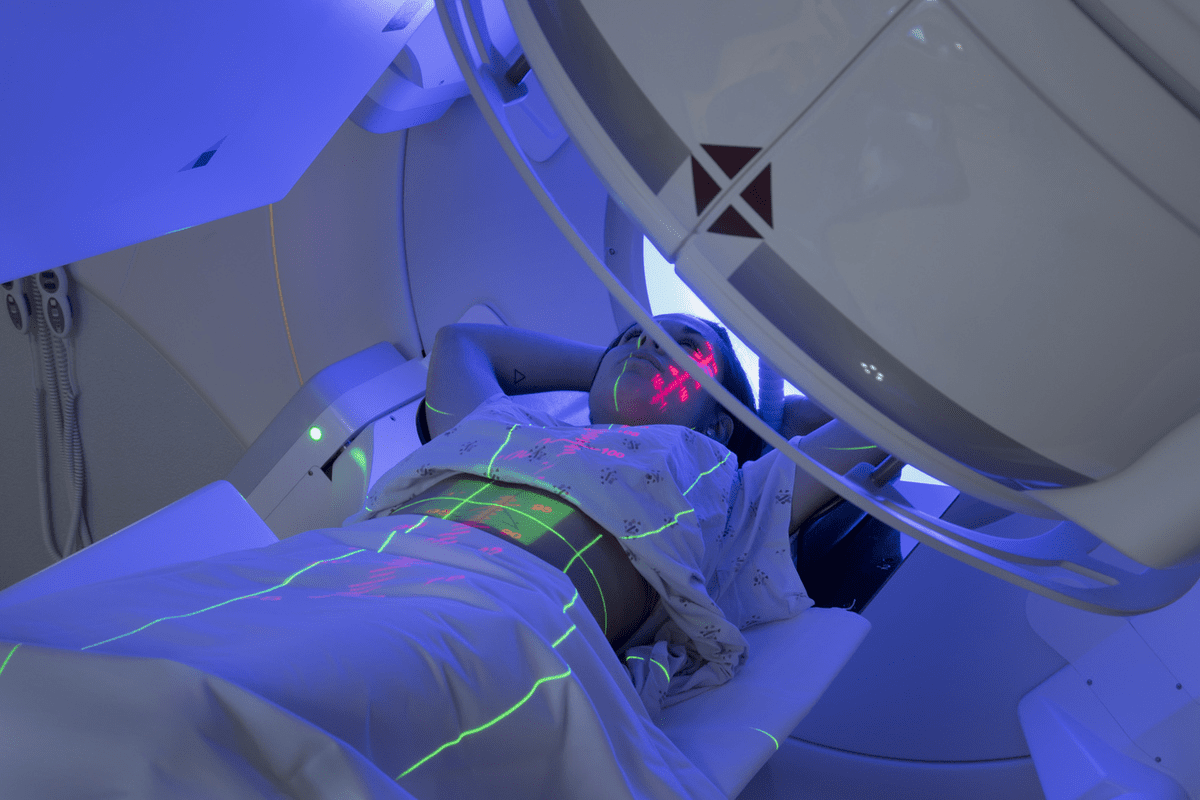
Advanced Cardiac Imaging in Athletes
Athletes need special heart checks, which advanced imaging is key for. The heart changes a lot with intense training. Sometimes, these changes look bad on a regular heart test. But, advanced imaging can tell the difference.
When is a Cardiac CT Scan Indicated?
A cardiac CT scan gives detailed heart pictures. It’s great for athletes to check for heart disease and see the heart’s shape.
Here’s when we suggest a cardiac CT scan:
- When an athlete’s symptoms hint at heart disease.
- To see how much calcium is in the heart’s arteries.
- When other tests don’t give clear answers.
|
Scenario |
Cardiac CT Scan Utility |
|---|---|
|
Symptoms of coronary artery disease |
High |
|
Evaluation of cardiac calcification |
High |
|
Inconclusive other imaging results |
Moderate to High |
Cardiac MRI in Athletic Heart Evaluation
Cardiac MRI (CMR) is a safe way to see the heart’s shape and how it works. It’s great for checking the athlete’s heart, telling real changes from bad ones.
A top cardiology journal says, “CMR is the best for checking the heart’s function and shape. It’s very important for athletes.”
“Cardiac MRI is key in sports cardiology. It gives deep insights into the heart’s shape and how it works.”
Journal of Cardiovascular Magnetic Resonance
Echocardiography as a Follow-up Tool
Echocardiography is a safe and common test for the heart. It’s often the first choice for checking the heart in athletes. It helps see how the heart changes over time.
We use echocardiography for follow-ups because it’s safe and gives a lot of info on heart health.
The Role of Computed Tomography in Cardiac Assessment
CT imaging is key for checking the heart. We use cardiac CT scans to see the heart’s details. This helps us find and treat heart problems.
What Does a Cardiac CT Scan Show?
A cardiac CT scan shows the heart’s parts, like chambers and valves. It spots calcium in arteries and checks how well the heart works. It also finds tumors or heart defects.
These detailed images help doctors see the heart’s structure and function clearly. This is important for diagnosing heart diseases, masses, and other issues.
CT Scan Procedure and Preparation
Before a cardiac CT scan, patients avoid caffeine and some medicines. They lie on a table in the CT scanner. The scanner moves around to get detailed heart images.
Preparation Steps:
- Remove any metal objects or jewelry
- Wear comfortable, loose-fitting clothing
- May be required to hold breath for short periods during the scan
The scan itself is quick, taking just a few minutes. But getting ready and recovering can take longer.
Benefits and Limitations of CT Imaging
Cardiac CT scans have many advantages. They are non-invasive and provide clear images. They can spot many heart problems. But, there are downsides like radiation exposure and the need for contrast agents.
Benefits:
- Non-invasive and relatively quick procedure
- High-resolution images of the heart and its structures
- Effective in detecting calcium deposits and assessing cardiac function
Limitations:
- Exposure to radiation
- Potential need for contrast agents
- May not be suitable for patients with certain medical conditions or implants
In summary, cardiac CT scans are vital for heart checks. They give detailed insights into the heart. While there are pros and cons, the info from CT scans is very helpful in diagnosing and treating heart issues.
Case Studies: Athletes with Abnormal ECGs
Athletes often have ECG abnormalities that doctors must carefully look at. They need to know if these are just from training or if they could be serious. It’s all about understanding the body’s changes from sports and any possible health issues.
Professional Athletes with Benign ECG Abnormalities
Many professional athletes have ECG changes that are not serious. For example, a 25-year-old elite cyclist had a slow heart rate and early repolarization. But no heart problems were found, so they could keep training.
A 30-year-old football player had an ECG showing left ventricular hypertrophy. An echocardiogram showed it was from sports, not a disease.
Cases Where Abnormal ECGs Revealed Serious Conditions
But sometimes, ECGs show serious heart issues in athletes. A 20-year-old basketball player had T-wave inversion on their ECG. A cardiac MRI found arrhythmogenic right ventricular cardiomyopathy, a dangerous heart condition.
A 28-year-old marathon runner had conduction abnormalities on their ECG. Tests showed a high-degree atrioventricular block, needing a pacemaker.
Follow-up and Outcomes
The outcomes for athletes with abnormal ECGs depend on the cause. For minor issues, regular checks and ECGs are needed. But serious problems might mean no sports, medicine, or surgery.
In summary, studying athletes with abnormal ECGs shows how critical careful checks are. Knowing the reasons and possible outcomes helps doctors give better care to athletes.
Pre-participation Screening Controversies
The use of electrocardiogram (ECG) screening in pre-participation evaluations has sparked intense debate. Ensuring athlete safety is complex, and the controversy over ECG screening is significant.
Mandatory ECG Screening Debate
The debate on mandatory ECG screening for athletes is complex. Supporters say it can spot life-threatening conditions like hypertrophic cardiomyopathy. Opponents worry about the cost, false positives, and the stress it causes.
A sports cardiology expert, believes ECG screening can detect cardiac issues. Yet, others think the costs and challenges outweigh the benefits.
Cost-Effectiveness Considerations
Cost is a major concern with mandatory ECG screening. The financial cost of such programs is high, and there’s debate on whether it’s worth it. A study in the Journal of the American College of Cardiology showed the cost per athlete is significant.
False positives also complicate the issue. Many athletes get abnormal ECG results that are later found to be okay. This can cause unnecessary stress, more tests, and higher healthcare costs.
International Approaches to Athlete Screening
Screening methods vary worldwide. Italy requires ECG screening for athletes, which has lowered sudden cardiac deaths. The U.S. has guidelines but doesn’t make it mandatory for all athletes.
Comparing international methods shows we need a balanced approach. It’s important to develop guidelines that work for different places and people.
Management of Athletes with Abnormal ECGs
Managing athletes with abnormal ECGs is a complex task. It’s about finding a balance between caution and letting athletes keep training and competing. Clinical guidelines help, but each case might need a special approach.
Clinical Decision-Making Process
The process for handling athletes with abnormal ECGs starts with figuring out if the ECG is just a normal response to exercise or if it’s a sign of a bigger issue. This means looking at the athlete’s medical history and doing a physical check-up.
More tests, like echocardiography or cardiac MRI, might be needed to understand the ECG better. These tests help decide if the athlete can keep playing sports.
|
Diagnostic Test |
Purpose |
Implications for Athlete |
|---|---|---|
|
Echocardiography |
Assess cardiac structure and function |
Helps determine if ECG abnormality is related to structural heart disease |
|
Cardiac MRI |
Detailed assessment of cardiac anatomy and function |
Useful in identifying conditions such as cardiomyopathy |
Return-to-Play Considerations
Deciding if an athlete can go back to playing after an abnormal ECG is tricky. It depends on the type of ECG abnormality, any symptoms the athlete has, and what extra tests show.
For some conditions, like long QT syndrome, athletes need special care before they can play sports again.
Long-term Monitoring Strategies
Athletes with abnormal ECGs need ongoing checks to make sure their condition doesn’t get worse. This might mean regular ECGs, echocardiograms, or other tests based on their condition.
Good long-term monitoring also means teaching the athlete about their condition. They need to know how to report new symptoms and manage their condition while training and competing.
Conclusion
Understanding ECGs in athletes is complex. It involves knowing normal changes and possible heart problems. Some ECG changes in athletes are harmless, but others can be serious.
It’s vital to correctly read ECGs to spot the difference between normal athlete’s heart and dangerous conditions. Healthcare experts use international guidelines and consider the athlete’s background and sport. This helps them make the right decisions about athlete heart health.
Our main aim is to keep athletes safe by carefully checking and managing any unusual ECG findings. This way, we can avoid sudden heart problems and let athletes compete safely.
FAQ
What is an ECG, and how does it work?
An electrocardiogram (ECG) is a test that checks the heart’s electrical activity. It detects the heart’s electrical signals and records them on a graph.
What are normal ECG patterns, and what do they indicate?
Normal ECG patterns vary but show a healthy heart. They include specific heart rates and waveforms. These signs show the heart is working well.
How does athletic training affect the heart, and what are the implications for ECG readings?
Athletic training changes the heart, known as cardiac remodeling. These changes can affect ECG readings. They might be normal or show a problem.
What is cardiac remodeling, and how does it relate to athletic training?
Cardiac remodeling is when the heart changes due to exercise. It makes the heart more efficient but can also show up as abnormal ECG findings.
What are some common ECG changes observed in athletes?
Athletes often see changes like sinus bradycardia and early repolarization patterns. These can be normal or might show a problem.
How do you differentiate between normal athletic adaptations and potentially dangerous heart disease on an ECG?
To tell the difference, you need to look closely at the ECG. Consider the athlete’s health, symptoms, and other tests.
What is the role of computed tomography (CT) in cardiac assessment?
CT scans help check the heart’s structure and function. They give detailed images of the heart and its blood vessels.
What does a cardiac CT scan show, and how is it used in athlete evaluation?
A cardiac CT scan shows detailed heart images, including the coronary arteries. It helps check athletes for heart conditions.
What are the benefits and limitations of using CT imaging in cardiac assessment?
CT imaging gives detailed heart images but involves radiation. It’s not right for all athletes.
How are abnormal ECGs managed in athletes, and what are the return-to-play considerations?
Managing abnormal ECGs involves looking at the athlete’s health and other tests. This helps decide when they can safely play again.
What are the controversies surrounding pre-participation screening for athletes?
There’s debate on whether athletes should have mandatory ECG screening. Some worry about cost and false positives.
How do demographic factors such as age, gender, and ethnicity affect ECG patterns in athletes?
Demographic factors can change ECG patterns in athletes. These factors are important when reading ECG results.
What are potentially dangerous ECG abnormalities in athletes, and how are they managed?
Dangerous ECG abnormalities include T-wave inversion and long QT syndrome. They need careful management and more tests.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4646899/