Acute coronary syndrome (ACS) is a serious condition where the heart’s blood flow is suddenly blocked. At Liv Hospital, we are committed to providing expert care and guidance to help you understand the risks and symptoms associated with ACS. Discover acute coronary artery disease risk factors and essential symptoms for early detection.
It’s important to know the risk factors and symptoms of ACS to get early treatment. We will look at the top ten risk factors for ACS and the key symptoms you should watch for.
By recognizing the signs and taking steps to prevent them, you can lower your risk of a heart attack. Our aim is to give you the knowledge and tools to keep your heart healthy.
It’s important to know about Acute Coronary Syndrome (ACS). It’s a group of heart problems, including heart attacks and unstable angina. ACS is a serious condition that needs quick treatment to protect the heart.
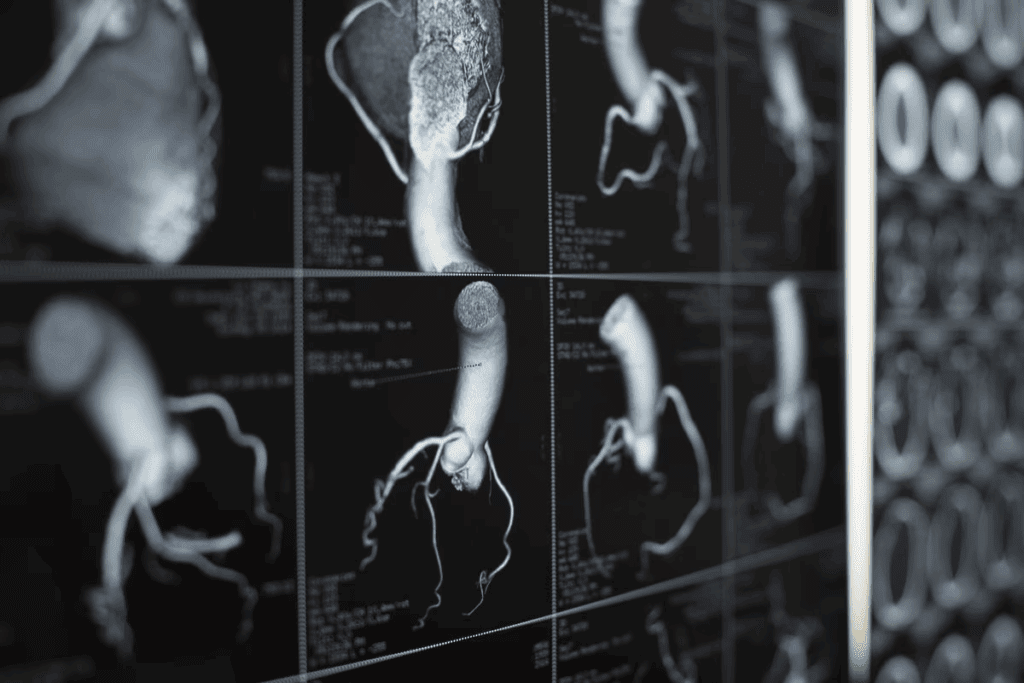
ACS happens when blood flow to the heart suddenly drops. This can cause heart attacks and unstable angina. The main reason is when a plaque in a heart artery bursts, causing a blood clot.
Symptoms of ACS include chest pain, shortness of breath, and feeling tired. Spotting these signs early is key to getting help fast.
Coronary artery disease (CAD) is the main cause of ACS. CAD makes heart arteries narrow or block. This happens when plaque, made of fat and cholesterol, builds up and ruptures.
Many things can make CAD worse, like high blood pressure, diabetes, and smoking. Controlling these risk factors helps prevent ACS.
| Risk Factor | Description | Impact on ACS |
| Hypertension | High blood pressure | Increases strain on coronary arteries |
| Diabetes Mellitus | High blood sugar levels | Damages coronary arteries and nerves |
| Hyperlipidemia | High levels of bad cholesterol | Contributes to plaque formation |
Spotting ACS early is critical. Quick treatment can greatly improve outcomes. The sooner help comes, the less damage to the heart.
ACS is a serious emergency that needs immediate care. If symptoms get worse, get help right away.
Hypertension is a big risk for Acute Coronary Syndrome (ACS). High blood pressure can lead to heart diseases, including ACS. It’s important to understand how it affects heart health to prevent and manage it.
Hypertension puts too much pressure on coronary arteries. This can damage them over time. The damage can cause the arteries to narrow and harden, a condition known as atherosclerosis.
This can stop the heart muscle from getting the oxygen and nutrients it needs. This can lead to ACS.
The mechanisms through which hypertension damages coronary arteries include:
Managing blood pressure is key to reducing ACS risk. Guidelines suggest keeping blood pressure below 130/80 mmHg for most adults. This can greatly lower the risk of heart events.
| Blood Pressure Category | Systolic BP (mmHg) | Diastolic BP (mmHg) |
| Normal | ||
| Elevated | 120-129 | |
| Hypertension Stage 1 | 130-139 | 80-89 |
| Hypertension Stage 2 | ≥ 140 | ≥ 90 |
Managing hypertension requires lifestyle changes and sometimes medicine. Lifestyle changes include eating healthy, exercising regularly, staying at a healthy weight, drinking less alcohol, and quitting smoking.
Medicine might include:
It’s important to check blood pressure regularly and follow up with doctors. This helps adjust treatment plans as needed to reach blood pressure targets.
It’s important to know how diabetes mellitus affects heart health to avoid Acute Coronary Syndrome (ACS). Diabetes can harm blood vessels and affect the heart, raising the risk of heart disease.
High blood sugar from diabetes can damage blood vessel linings. This makes them more likely to block. This damage is a big reason for coronary artery disease, which can cause ACS.
People with diabetes are more likely to get ACS. This is because of insulin resistance, inflammation, and bad cholesterol levels. These issues speed up atherosclerosis, making heart attacks more likely.
Keeping blood sugar in check is key for diabetics to avoid heart problems. This can be done through diet, exercise, or medication.
The table below shows how to control blood sugar and its benefits:
| Strategy | Benefits |
| Dietary Changes | Reduces blood sugar spikes, improves insulin sensitivity |
| Regular Exercise | Enhances insulin sensitivity, improves cardiovascular health |
| Medication Adherence | Maintains blood sugar within target range, prevents complications |
Understanding diabetes’ effect on heart health and managing blood sugar can lower ACS risk.
Hyperlipidemia is a condition where cholesterol and triglycerides are not at normal levels. It’s a big factor in Acute Coronary Syndrome (ACS). It happens when there’s too much of certain lipids in the blood.
Cholesterol moves through the blood with the help of lipoproteins, like LDL and HDL. LDL cholesterol, or “bad” cholesterol, can build up in arteries. This can cause atherosclerosis. On the other hand, HDL cholesterol, or “good” cholesterol, helps clear out extra cholesterol.
It’s important to know how LDL and HDL levels affect heart health. Too much LDL and not enough HDL can raise the risk of ACS.
High LDL cholesterol can lead to atherosclerotic plaques in coronary arteries. These plaques can rupture, causing a blood clot. This can block the artery and lead to ACS.
The buildup of lipids in arteries makes them more likely to rupture. So, managing lipid levels is key to preventing ACS.
The goal of managing lipids is to lower the risk of ACS. This means reducing LDL cholesterol and sometimes increasing HDL cholesterol.
| Lipid Parameter | Desirable Level | Therapeutic Action |
| LDL Cholesterol | <100 mg/dL (or <70 mg/dL for high-risk patients) | Statins, Ezetimibe, PCSK9 inhibitors |
| HDL Cholesterol | >60 mg/dL | Lifestyle modifications, Niacin (in selected cases) |
| Triglycerides | <150 mg/dL | Fibrates, Omega-3 fatty acids, Lifestyle modifications |
Understanding hyperlipidemia and its effects on heart health is key. We can prevent ACS by managing lipid levels. This is done through lifestyle changes and, if needed, medication.
Tobacco use is a big risk for Acute Coronary Syndrome (ACS). It’s something we can change. Smoking harms the heart in many ways, raising the risk of heart disease.
Smoking harms coronary arteries in several ways. It increases inflammation and oxidative stress. This can cause plaque buildup in arteries.
Smoking also damages the endothelium, the blood vessel lining. This makes it hard for blood vessels to open up and flow properly.
The chemicals in tobacco smoke promote platelet aggregation. This means blood clots are more likely to form. These clots can block arteries, causing ACS. Smoking also reduces oxygen delivery to the heart, making it work harder.
Quitting smoking greatly lowers ACS risk. Smoking cessation improves heart health right away. Within a year, heart disease risk drops a lot.
There are many ways to quit smoking. Nicotine Replacement Therapy (NRT) and prescription medications like bupropion and varenicline help with cravings.
Counseling and support groups are also key. The National Cancer Institute’s Smoking Quitline offers free help to quit smoking.
Genetic and environmental factors both play a role in the risk of ACS. Family history is a key indicator. People with a family history of heart disease face a higher risk of ACS.
Coronary artery disease, a major cause of ACS, has a strong genetic link. Studies show that genetics can impact its development and progression. Specific genetic mutations can affect lipid metabolism, blood pressure regulation, and other factors that contribute to coronary artery disease.
Familial hypercholesterolemia is a genetic condition with very high LDL cholesterol levels. It greatly increases the risk of early coronary artery disease. Knowing these hereditary factors is key to identifying those at higher risk.
For those with a family history of coronary artery disease or ACS, early and regular screening is recommended. This includes checking lipid profiles, blood pressure, and glucose levels. Early detection of risk factors allows for timely intervention, potentially reducing the risk of ACS.
Genetic testing can offer valuable insights for those with a strong family history of coronary artery disease. But, it’s important to consider it carefully. Counseling is needed to understand the implications of test results.
Genetic testing is not routine for everyone. It may be recommended for those with a significant family history or other specific risk factors. The decision to undergo genetic testing should be made with a healthcare provider.
Understanding Acute Coronary Syndrome (ACS) is complex. Obesity and metabolic syndrome play big roles in heart health. Obesity is growing worldwide, raising ACS risk.
Body Mass Index (BMI) helps sort people into weight groups. A higher BMI means a higher heart disease risk, including ACS. Studies show a 29% increase in heart disease risk for every 5-unit BMI increase in men and 26% in women.
BMI affects heart health in many ways. It’s linked to inflammation, insulin resistance, and bad cholesterol levels. These issues are common in those with higher BMIs.
Excess belly fat is a big worry. It’s linked to metabolic syndrome and heart disease risk. Visceral fat releases harmful substances that cause heart blockages.
Measuring your waist is a simple way to check for belly fat. Men should aim for a waist under 40 inches, and women under 35. This helps lower heart disease risk.
Managing weight is key for those with obesity and metabolic syndrome. A good plan includes eating better, moving more, and changing habits. Focus on whole foods like veggies, fruits, grains, lean meats, and healthy fats.
For some, medical help or bariatric surgery might be needed if diet and exercise don’t work. But, always talk to a doctor first.
Regular physical activity is key for heart health and lowering ACS risk. A sedentary lifestyle, with too much sitting, leads to heart diseases.
Adults need at least 150 minutes of moderate activity or 75 minutes of vigorous activity weekly. Adding muscle-strengthening activities two or more times a week boosts heart health.
Exercise is vital for preventing ACS by improving heart function and lowering blood pressure. A good exercise plan should include:
The American Heart Association says, “Regular physical activity can prevent heart disease. It improves circulation, strengthens the heart, and lowers risk factors like high blood pressure and high cholesterol.”
For those new to exercise or returning after a break, start slow and increase gradually. Always talk to a healthcare provider before starting any new exercise, even more so if you have health issues.
“The key to a successful exercise program is sustainability. Finding activities you enjoy and incorporating them into your daily routine can make physical activity a lifelong habit.”
American Council on Exercise
By knowing the dangers of a sedentary lifestyle and staying active, you can lower your risk of ACS and keep your heart healthy.
It’s important to know how age and gender affect the risk of Acute Coronary Syndrome (ACS). Both play big roles in who might get ACS. This knowledge helps in preventing and treating the condition.
Older people face a higher risk of ACS. This is because aging brings plaque buildup in arteries, higher blood pressure, and less physical activity. The risk goes up after 45 for men and 55 for women. It shows why keeping an eye on heart health is key as we get older.
ACS shows up differently in men and women. Women often have symptoms that are not typical like men. They might feel short of breath, nauseous, or tired instead of chest pain.
It’s vital for doctors to know these differences. This helps them diagnose and treat quickly and correctly.
Preventing ACS needs a plan that fits the person’s age and risk. For older adults, this might mean more heart health checks, changing lifestyle, and using medicines for high blood pressure and cholesterol.
After a first heart attack, patients face a big chance of having another. This makes stopping future heart attacks very important. A heart event can change a person’s life, and the fear of another event is big for patients and their families.
Secondary prevention helps lower the chance of more heart attacks in those who have already had one. It includes changing how you live, taking your medicine, and joining cardiac rehab programs.
Key components of secondary prevention include:
Sticking to your medicine is key after a heart attack. Taking your medicine as told can lower the risk of another heart attack and help you feel better. We stress how important it is to know why you’re taking each medicine and what happens if you don’t.
Common challenges to medication adherence include:
Cardiac rehab is a program that helps you get better after a heart event. It includes exercise, learning, and support. We see how it helps lower the risk of another heart attack and makes life better.
The benefits of cardiac rehabilitation include:
By focusing on stopping future heart attacks, we can help patients a lot. This includes sticking to their medicine and joining cardiac rehab. This way, we can make sure patients don’t have to go through another heart attack.
It’s vital to know the signs of Acute Coronary Syndrome (ACS) to get help fast. ACS shows itself in different ways, with symptoms that can change in how bad they are and how they feel.
Chest pain, or CP, is a key sign of ACS. This pain feels like pressure or tightness in the chest. It might spread to the arms, back, neck, jaw, or stomach.
The pain can stay the same or change, and its strength can vary. Knowing what chest pain feels like is key. ACS pain is often a squeezing or heavy feeling, not a sharp pain.
People with ACS might also have other symptoms. These include shortness of breath, nausea or vomiting, feeling lightheaded or dizzy, and feeling very tired. These signs can show up with or without chest pain and are important signs of ACS.
It’s important to remember that some people, like women, might not show ACS symptoms in the usual way. They might have less typical or more subtle signs. This is why it’s important to know all the symptoms of ACS.
Studies have found that men and women can show ACS symptoms differently. Women are more likely to have symptoms like back or neck pain, indigestion, or extreme tiredness. These differences can sometimes cause delays in getting a diagnosis and treatment.
Knowing these differences can help doctors and patients spot ACS symptoms better. This ensures that people get the care they need quickly and correctly.
The American Heart Association (AHA) sets clear guidelines for ACS management. They stress the need for quick action. These guidelines help doctors give the best care to ACS patients.
The AHA ACS guidelines focus on early detection and treatment. They suggest a detailed plan that includes:
ACLS protocols are key in managing ACS. They cover:
ACLS ensures patients get quick and effective care in heart emergencies.
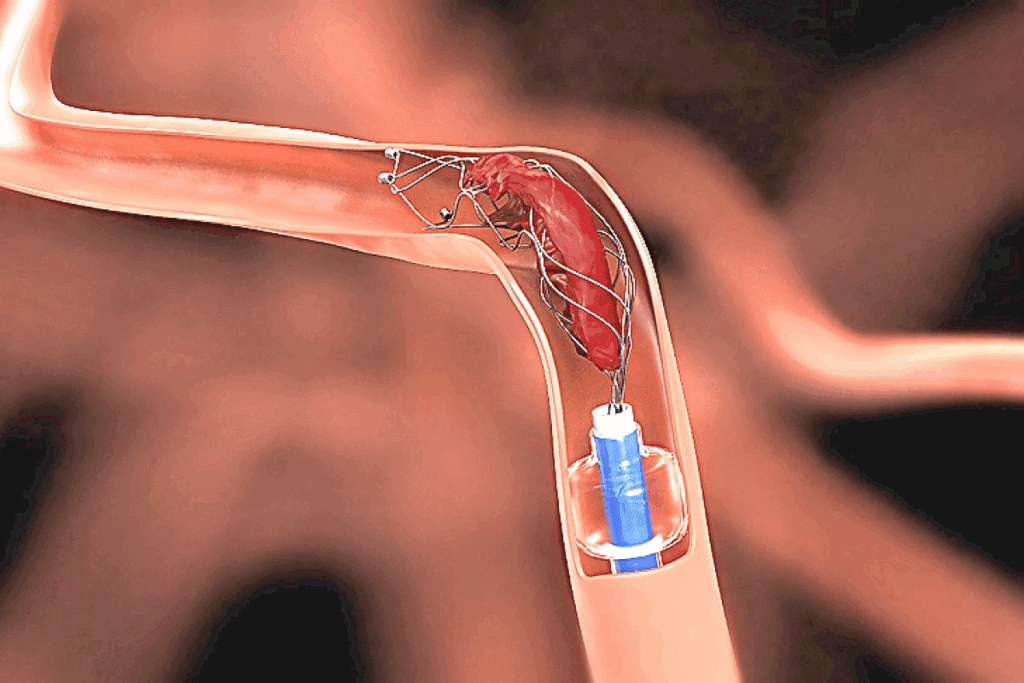
Dual antiplatelet therapy (DAPT) is vital in ACS management. It includes:
Statins are also recommended to lower the risk of more heart problems. The guidelines suggest using high-intensity statins for most patients.
Reperfusion strategies are key, mainly for STEMI patients. The guidelines suggest:
Quick reperfusion is essential, aiming to restore blood flow as fast as possible.
By sticking to current guidelines and treatment plans, healthcare providers can better help ACS patients.
Knowing the risk factors and symptoms of Acute Coronary Syndrome (ACS) is key. We’ve looked at many factors that can lead to ACS. These include high blood pressure, diabetes, high cholesterol, smoking, family history, being overweight, and not being active.
By managing these risk factors, you can protect your heart. Keep your blood pressure and blood sugar in check. Also, control your cholesterol, quit smoking, and stay at a healthy weight. Regular exercise is also important.
Being aware of ACS symptoms can help you get help fast. Look out for chest pain and other signs. Take care of your heart by living a healthy lifestyle and seeing a doctor if you have concerns. This way, you can lower your risk of ACS and keep your heart healthy.
Acute Coronary Syndrome (ACS) is a serious heart condition. It happens when blood flow to the heart suddenly stops. This includes heart attacks and unstable angina. It’s a medical emergency because quick action is needed to avoid serious harm or death.
Several factors increase the risk of ACS. These include high blood pressure, diabetes, high cholesterol, smoking, family history, obesity, metabolic syndrome, and a sedentary lifestyle. Knowing these risks helps in early detection and prevention.
High blood pressure can damage heart arteries. This is because it increases the pressure on the heart. Lowering blood pressure through lifestyle changes and medication can help prevent ACS.
Diabetes can harm blood vessels and nerves that control the heart. This increases the risk of heart disease and ACS. Keeping blood sugar levels under control is key to preventing heart problems in diabetics.
Quitting smoking greatly lowers the risk of ACS. Tobacco damages heart arteries. There are resources like counseling and medication to help quit smoking.
Family history can raise the risk of ACS. Genetic factors can affect heart disease. Genetic testing may be suggested for those with a family history of heart disease.
Obesity and metabolic syndrome increase heart disease risk. They cause insulin resistance, inflammation, and high cholesterol. Losing weight through diet and exercise can reduce this risk.
ACS symptoms include chest pain or discomfort. It can feel like pressure or tightness. Women may have different symptoms, like shortness of breath or nausea.
The American Heart Association (AHA) has guidelines for ACS management. These include using dual antiplatelet therapy, statins, and reperfusion strategies. Following these guidelines is important for the best patient outcomes.
After an ACS event, secondary prevention is key. This includes taking medication as directed and participating in cardiac rehabilitation. These steps help manage risk factors and improve heart health.
Regular exercise is vital for heart health and ACS prevention. Aim for at least 150 minutes of moderate-intensity aerobic activity each week.
Cardiac rehabilitation offers a full recovery plan. It includes exercise, heart-healthy education, and counseling. These programs can greatly improve outcomes and lower the risk of future heart problems.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us