
At Liv Hospital, we make complex medical terms clear. Acute Coronary Syndrome (ACS) includes heart issues where blood flow to the heart muscle suddenly drops.Understand acute coronary syndrome means, its medical definition, and clinical importance.
This drop in blood flow usually happens because of a blockage or narrowing in the coronary arteries. These arteries carry blood to the heart. Knowing what ACS means is key for quick medical help and effective treatment.
We focus on giving our patients clear and caring care. We make sure they get the best and most ethical treatment for ACS-related conditions.
Key Takeaways
- ACS refers to a group of conditions involving sudden reduced blood flow to the heart.
- The condition is often caused by a blockage or narrowing of the coronary arteries.
- Understanding ACS is key for quick medical help.
- Liv Hospital is dedicated to providing top-notch and ethical care for ACS patients.
- Our approach emphasizes clear and caring care for our patients.
What Acute Coronary Syndrome Means in Medical Terminology – 300 words
It’s important to know what acute coronary syndrome (ACS) means in medical terms. This is true for both doctors and patients. ACS refers to a group of heart problems caused by sudden reduced blood flow to the heart. Knowing this helps in clear communication and making smart choices.
Origin and Etymology of the Term
The term “acute coronary syndrome” comes from describing sudden heart events. “Acute” means it happens quickly, “coronary” points to the heart’s arteries, and “syndrome” means a set of symptoms. Doctors use a special code for chest pain, a key sign of ACS, to spot it fast.
ACS as an Umbrella Term
ACS is a broad term that covers many heart issues. These include unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). This helps doctors diagnose and treat patients better.
How ACS Differs from Other Cardiac Conditions
ACS is different from other heart problems like stable angina. Stable angina is more predictable and happens when you exert yourself. But ACS can happen suddenly, even when you’re resting. Below is a table that shows how ACS is different from other heart issues.
| Condition | Presentation | Severity |
| ACS | Acute, often unexpected | High |
| Stable Angina | Predictable, with exertion | Moderate |
| Heart Failure | Gradual, with symptoms like shortness of breath | Varies |
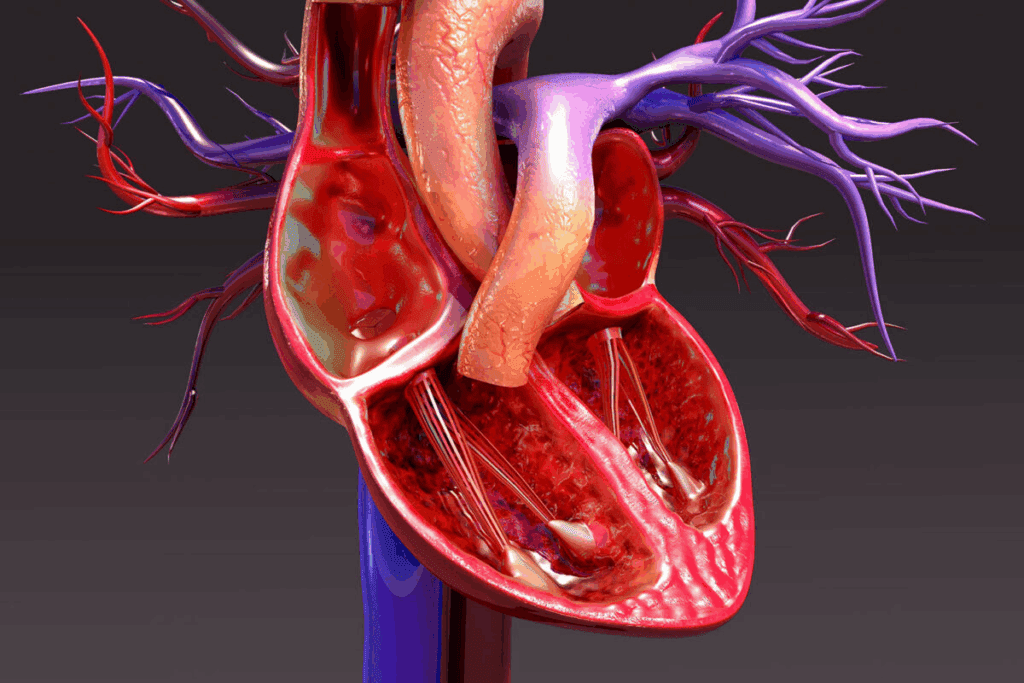
The Pathophysiology Behind Acute Coronary Syndrome – 250 words
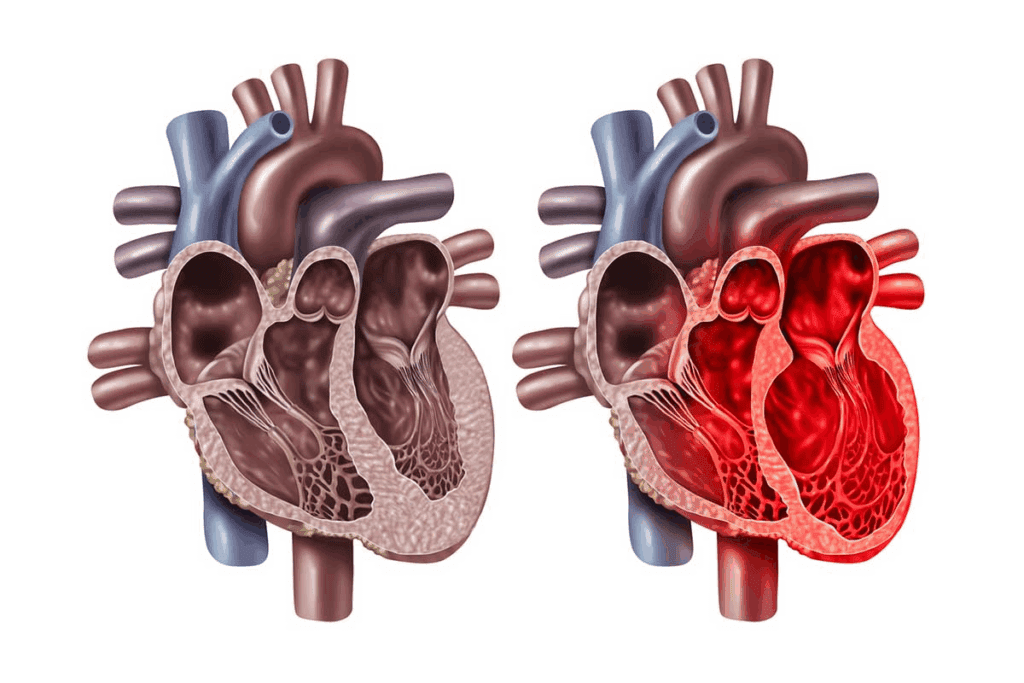
Understanding ACS is key to knowing how it happens and why quick medical help is needed. ACS often comes from fatty deposits in the coronary arteries, called plaque. This plaque can narrow the arteries and block blood flow. If the plaque bursts, a blood clot might form, which could cause a heart attack.
Coronary Artery Disease and Atherosclerosis
Coronary artery disease (CAD) plays a big role in ACS. CAD is marked by atherosclerosis, where plaque builds up in the artery walls. This causes inflammation and damage, narrowing the arteries and reducing blood flow to the heart.
As atherosclerosis gets worse, plaques can become unstable. This makes them more likely to rupture.
The Process of Plaque Rupture and Thrombosis
Plaque rupture is a key event in ACS. When a plaque bursts, it exposes material to the blood that triggers a blood clot. This clot can block the artery, leading to heart muscle damage or even a heart attack.
The clotting process is complex. It involves platelets getting activated and sticking together, and the coagulation cascade. This results in the symptoms of ACS.
The Spectrum of Acute Coronary Syndrome Conditions – 300 words
It’s important to know the different heart conditions under the ACS umbrella. Acute Coronary Syndrome (ACS) includes unstable angina, Non-ST-Segment Elevation Myocardial Infarction (NSTEMI), and ST-Segment Elevation Myocardial Infarction (STEMI). These conditions affect the heart’s blood supply.
Unstable Angina
Unstable angina happens when blood flow to the heart drops but doesn’t cause permanent damage. It shows as chest pain or discomfort. Prompt medical evaluation is essential to stop it from getting worse.
Non-ST-Segment Elevation Myocardial Infarction (NSTEMI)
NSTEMI is a heart attack with a partial blockage of a coronary artery. It’s diagnosed when heart muscle damage is shown, but the ECG doesn’t show ST-segment elevation. Treatment involves stabilizing the patient and addressing the underlying cause of the blockage.
ST-Segment Elevation Myocardial Infarction (STEMI)
STEMI is a severe heart attack with a complete blockage of a coronary artery. It leads to significant heart muscle damage. It’s identified by ST-segment elevation on an ECG. Immediate reperfusion therapy is critical to restore blood flow and minimize damage.
In summary, ACS includes unstable angina, NSTEMI, and STEMI, each with its own characteristics and clinical implications. Understanding these differences is vital for healthcare professionals to provide the right care.
Recognizing ACS Symptoms – 300 words
ACS symptoms can vary a lot, from classic chest pain to less common signs. It’s key to spot these signs early for better care and results.
Classic Chest Pain Presentation
Chest pain or discomfort is the top sign of ACS. People often say it feels like pressure or tightness. This pain can spread to the arms, back, neck, jaw, or stomach.
The term for chest pain in medical talk is often “CP” or “angina.” It’s important to know that how people feel pain can be different.
Atypical Symptoms
Not everyone with ACS has chest pain. Some might feel short of breath, nauseous, tired, dizzy, or have pain in their upper body or jaw. These signs are more common in women, older folks, and those with diabetes.
Spotting these atypical symptoms early is key to quick diagnosis and treatment.
Symptom Differences in Special Populations
ACS symptoms can change in different groups. Women often feel nausea and fatigue. Older adults might seem confused or weak. Diabetics might not feel pain as much because of nerve damage.
Knowing these differences helps doctors make quick and right diagnoses.
| Population | Common ACS Symptoms |
| General Population | Chest pain, discomfort |
| Women | Nausea, fatigue, shortness of breath |
| Older Adults | Confusion, generalized weakness |
| Diabetic Patients | Painless or atypical presentations |
By knowing how ACS symptoms can show up differently, we can do better in diagnosing and treating. This leads to better health outcomes for patients.
Risk Factors Contributing to Acute Coronary Syndrome – 250 words
Acute Coronary Syndrome (ACS) is caused by many risk factors. These can be changed or not changed. Knowing these factors is key to preventing and managing ACS.
Modifiable Risk Factors
Several things can be changed to lower ACS risk. These include smoking, high blood pressure, high cholesterol, and diabetes. Making lifestyle changes and getting medical help can greatly reduce ACS risk.
Non-Modifiable Risk Factors
Some risk factors can’t be changed. These include older age and family history of heart disease. Even though we can’t change these, knowing them helps in planning how to prevent and manage ACS.
Diagnostic Approach to ACS – 350 words
Diagnosing Acute Coronary Syndrome (ACS) needs a detailed plan. This plan includes checking the patient’s health, looking at the heart’s electrical activity, and running lab tests. This way, doctors can spot and treat ACS correctly.
Initial Clinical Assessment
The first step in diagnosing ACS is very important. Doctors take a detailed medical history and do a physical exam. They look for signs like chest pain or discomfort. Spotting ACS symptoms early is key to acting fast.
Electrocardiogram (ECG) Findings
An electrocardiogram (ECG) is a key tool for ACS diagnosis. It checks the heart’s electrical signals. It can show if the heart is not getting enough blood, like ST-segment changes. ECG results help decide on urgent treatments.
Cardiac Biomarkers
Cardiac biomarkers are proteins that show up in the blood when the heart is damaged. These include troponin and creatine kinase. High levels mean the heart muscle is hurt. Tracking these biomarkers over time helps doctors figure out the extent of heart damage.
Advanced Imaging Techniques
For some patients, tests like echocardiography or coronary angiography are used. These tests give clear pictures of the heart. They help find out where the heart is not getting enough blood. These images help doctors make treatment plans and predict how well the patient will do.
By using a mix of clinical checks, ECGs, biomarkers, and imaging, doctors can accurately diagnose ACS. This lets them start the right treatment right away.
Emergency Management of Acute Coronary Syndrome – 300 words
When a patient has ACS, quick and right action is key. It can greatly affect their survival and recovery. The main goal is to quickly get blood flowing to the heart again, to lessen damage.
Initial Stabilization Measures
First, oxygen, aspirin, and nitroglycerin are given to ease symptoms and boost heart oxygen. Keeping an eye on the patient’s vital signs and ECG is vital. It helps figure out how bad the situation is and what to do next.
Pharmacological Interventions
Medicines like heparin or bivalirudin and P2Y12 inhibitors are used. They stop more clots from forming and lower heart event risks.
Reperfusion Strategies
Reperfusion strategies are key in ACS management. They include PCI and thrombolysis to get blood flowing back to the heart. PCI is the best choice if it’s available quickly.
| Reperfusion Strategy | Description | Benefits |
| PCI | Percutaneous Coronary Intervention | Restores blood flow, reduces mortality |
| Thrombolysis | Dissolves clots obstructing coronary arteries | Effective when PCI is not readily available |
Timing Considerations in Treatment
Time is very important in ACS treatment. Waiting too long can make things worse. Fast decision-making is key for the best results.
A study in a top medical journal says, “Time is muscle” for ACS. It shows how urgent quick action is.
“The sooner the reperfusion therapy is initiated, the better the outcomes for patients with ACS.”
— Leading Medical Journal
Invasive Procedures for ACS Treatment – 250 words
Acute Coronary Syndrome (ACS) often needs invasive treatments to improve blood flow. These treatments are key to managing the condition and stopping further heart damage.
Percutaneous Coronary Intervention (PCI)
Percutaneous Coronary Intervention (PCI) is a non-surgical method to treat narrowed coronary arteries in ACS patients. A catheter is used to reach the blocked artery. Then, a balloon is inflated to clear the blockage, and a stent is placed to keep the artery open.
Benefits of PCI include:
- Minimally invasive, reducing recovery time
- Effective in restoring blood flow
- Can be performed under local anesthesia
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a surgical method. It bypasses blocked coronary arteries with grafts, usually from the patient’s leg or chest. This procedure is recommended for complex coronary artery disease or when PCI doesn’t work well.
| Procedure | Description | Benefits |
| PCI | Non-surgical, uses catheter and stent | Less invasive, quicker recovery |
| CABG | Surgical, bypasses blocked arteries | Effective for complex disease, long-term results |
Post-ACS Care and Secondary Prevention – 300 words
Managing post-ACS care is complex. It includes taking medication, going through rehabilitation, and making lifestyle changes. This approach is key to lowering the risk of heart problems and improving life quality.
Medication Regimens
Medicine is essential in post-ACS care. Antiplatelet agents, beta-blockers, and statins are used to keep the heart healthy. Antiplatelet agents stop blood clots, beta-blockers ease the heart’s work, and statins lower cholesterol. Taking these medicines as directed is vital to stop future heart issues.
Cardiac Rehabilitation Programs
Cardiac rehab programs focus on improving heart health. They combine exercise, education, and lifestyle advice. These programs help patients recover from heart attacks and lower future heart risks. By joining cardiac rehab, patients can boost their heart health and life quality.
Lifestyle Modifications
Making lifestyle changes is a big part of post-ACS care. Patients are advised to eat a heart-healthy diet, stay active, and stop smoking if they can. These steps can greatly lower the chance of heart problems and improve health. Stress management through meditation or yoga is also helpful.
Combining medication, cardiac rehab, and lifestyle changes helps patients manage post-ACS care well. This approach reduces the risk of future heart issues.
Complications and Prognosis Following ACS – 250 words
ACS can lead to serious complications, both right away and later on. It’s key to manage these issues well for a good recovery.
Immediate Complications
Right after ACS, some problems can be very serious and need quick help. These include arrhythmias and heart failure. Arrhythmias are when the heart beats irregularly because of damage. Heart failure is when the heart can’t pump enough blood.
| Complication | Description |
| Arrhythmias | Irregular heartbeats that can be too fast, too slow, or irregular |
| Heart Failure | The heart’s inability to pump enough blood for the body’s needs |
Long-term Complications
Long-term issues can really affect a person’s life. These include recurrent ACS and chronic heart failure. Recurrent ACS is when another heart attack happens. Chronic heart failure is when the heart gets worse at pumping blood over time.
“The risk of recurrent cardiovascular events remains high after an initial ACS event, stressing the need for ongoing care and prevention.”
— American Heart Association
Factors Affecting Prognosis
Many things can change how well someone does after ACS. These include how bad the first event was, any other health problems, and how well they follow their treatment plan. A good care plan that fits each person’s needs is very important.
Special Considerations in ACS Management – 300 words
Managing Acute Coronary Syndrome (ACS) needs careful thought about different patient groups and health issues. Each patient’s treatment plan must be made to fit their specific needs. This includes looking at factors that can change how a patient is diagnosed and treated.
ACS in Women
Women with ACS often show symptoms differently than men. They might not have typical chest pain and could have symptoms like nausea and fatigue. It’s important to recognize these differences to provide timely and right care.
ACS in Elderly Patients
Elderly patients with ACS usually have more health problems and a higher risk of serious issues. Their symptoms might not be typical, like confusion or shortness of breath instead of chest pain. They need careful evaluation and treatment plans made just for them.
ACS in Diabetic Patients
Diabetic patients face a higher risk of ACS and often have a worse outcome. Diabetes can make managing ACS harder because of silent ischemia and the need to control blood sugar. It’s important to closely watch and adjust treatment to improve results.
ACS with Comorbidities
Patients with many health issues face a big challenge in managing ACS. Conditions like kidney failure, COPD, and others can affect treatment choices and outcomes. A detailed approach that looks at all health issues is key for managing ACS well.
In conclusion, managing ACS well needs a deep understanding of the factors that can affect patient results. By focusing on the unique needs of different patient groups, healthcare providers can offer more tailored and effective care.
Conclusion – 250 words
Understanding Acute Coronary Syndrome (ACS) is key for quick and effective care. ACS includes unstable angina, NSTEMI, and STEMI. Recognizing symptoms early and treating them right can greatly help patients.
Managing ACS well means using a complete approach. This includes checking patients first, doing tests, and using medicines and ways to get blood flow back. Knowing the signs and risks of ACS helps doctors give better care.
In short, managing ACS needs a plan that includes fast diagnosis, right treatment, and steps to prevent it from happening again. By knowing how to handle ACS and using proven methods, we can improve care and fight heart disease better.
FAQ
What does Acute Coronary Syndrome (ACS) mean in medical terms?
Acute Coronary Syndrome (ACS) is a term for sudden heart problems. It includes heart attacks and unstable angina.
What is the meaning of ACS in medical terminology?
ACS is a broad term in medicine. It covers many heart issues caused by sudden blood flow problems. This includes unstable angina, NSTEMI, and STEMI.
What are the different conditions classified under ACS?
ACS includes unstable angina, NSTEMI, and STEMI. Each has its own symptoms and treatment needs.
What are the symptoms associated with ACS?
ACS symptoms can be chest pain or other signs. They can be different for women, older people, and diabetics. It’s important to recognize them quickly.
What are the risk factors that contribute to the development of ACS?
Risk factors for ACS are lifestyle choices and genetics. Some things you can change, and some you can’t.
How is ACS diagnosed?
Doctors use several methods to diagnose ACS. This includes checking the heart with an ECG and blood tests. They also use imaging to get a clear picture.
What is the emergency management of ACS?
Treating ACS quickly is key. Doctors use medicines and procedures to open blocked arteries. This helps the heart get blood again.
What invasive procedures are used in the treatment of ACS?
Doctors use PCI and CABG to treat ACS. These procedures help restore blood flow to the heart.
What care is required after an ACS event?
After ACS, patients need ongoing care. This includes medicines, cardiac rehab, and lifestyle changes. These steps help prevent future heart problems.
What are the possible complications after an ACS event?
ACS can lead to immediate or long-term problems. These depend on the severity of the event and how well it’s treated.
Are there special considerations in the management of ACS?
Yes, managing ACS requires special care for certain groups. This includes women, older adults, diabetics, and those with other health issues. Each needs a tailored approach.
What is the meaning of ACS medical abbreviation?
ACS stands for Acute Coronary Syndrome. It’s a serious heart condition.
What does ACS mean in medical terms?
ACS is a serious heart condition. It involves sudden heart problems and includes various cardiac conditions.
References:
National Center for Biotechnology Information. (2025). What Does Acute Coronary Syndrome ACS Mean in. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459157/







