Last Updated on November 25, 2025 by Ugurkan Demir

Understanding Acute Decompensated Heart Failure (ADHF) is key for quick medical help. At Liv Hospital, we know how important fast action is for ADHF. This is a sudden bad turn in heart failure symptoms.
The Medical organization says heart failure happens when the heart can’t pump blood well. ADHF is when this gets worse suddenly, needing urgent care or hospital stay.
We aim to give top-notch care for ADHF patients. We follow the newest medical rules and ways. Our focus is on you, making sure you get the best care fast.
Key Takeaways
- ADHF is a sudden worsening of heart failure symptoms needing urgent care.
- Quick action is vital for managing ADHF well.
- Liv Hospital is dedicated to giving the best care for ADHF patients.
- We put you first, making sure you get fast and good care.
- We use the latest medical rules and ways in treating ADHF.
Understanding Acute Decompensated Heart Failure
It’s key for doctors to know about acute decompensated heart failure (ADHF) to treat it well. ADHF happens when the heart can’t fill or pump blood right, as the NCBI Bookshelf says.
Definition and Pathophysiology
ADHF comes on fast in people with or without heart problems. It’s caused by heart issues and changes in the body. These changes upset the heart’s balance, causing ADHF symptoms.
The body’s stress response and heart changes play a big role in ADHF. The heart’s workload goes up, leading to less blood flow and higher pressure in the veins.
Difference Between Chronic Heart Failure and ADHF
Chronic heart failure and ADHF are different but related. Chronic heart failure is a long-term issue where the heart can’t pump enough blood. ADHF is a sudden worsening of symptoms that needs quick action.
Chronic heart failure is treated over time, but ADHF needs urgent care. This care helps prevent things from getting worse.
ADHF Medical Abbreviation and Terminology
The term “ADHF” is used a lot in medicine for acute decompensated heart failure. Knowing this helps doctors talk clearly. Terms like “decompensated cardiac failure” mean the same thing as ADHF.
Knowing these terms helps doctors diagnose and treat patients right. It also makes sharing patient info easier, leading to better care.
Common Precipitating Factors of ADHF
It’s key for doctors to know what causes acute decompensated heart failure. This knowledge helps them create better treatment plans. Many things can lead to ADHF, and knowing them is vital for managing the condition.
Cardiac Triggers: Arrhythmias and Ischemia
Heart problems are a big part of why ADHF happens. Arrhythmias, or irregular heartbeats, make it hard for the heart to pump. Ischemia, or less blood to the heart, is another big factor.
- Arrhythmias, like atrial fibrillation, raise the risk of ADHF.
- Ischemia from coronary artery disease can cause sudden decompensation.
Non-Cardiac Triggers: Infections and Medication Non-Adherence
Other things also play a big role in ADHF. Infections, like pneumonia and sepsis, put extra stress on the heart. Medication non-adherence is also a big issue, as not taking heart meds can make symptoms worse.
- Infections make the body need more oxygen, stressing the heart.
- Not taking meds as directed can lead to uncontrolled symptoms and ADHF.
Lifestyle Factors Contributing to Decompensation
How we live can also lead to ADHF. Dietary indiscretion and excessive alcohol consumption are big culprits. Eating too much salt can cause fluid buildup, making heart failure symptoms worse. Drinking too much alcohol can also harm the heart and cause arrhythmias.
- A diet high in sodium can lead to fluid overload and worsen heart failure.
- Drinking too much alcohol can directly harm heart function.
Knowing what causes ADHF is key to preventing and managing it. By tackling these triggers, doctors can create better treatment plans. This helps improve patient outcomes.
4 Primary Symptoms of Acute Decompensated Heart Failure
Knowing the main symptoms of ADHF is key for quick diagnosis and treatment. ADHF happens when the heart can’t pump enough blood. This leads to fluid buildup in the lungs and body. Spotting symptoms early can greatly help patients.
Severe Shortness of Breath (Dyspnea)
Severe shortness of breath, or dyspnea, is a major sign of ADHF. Fluid in the lungs makes it hard to breathe. This can happen suddenly, even when resting or at night.
Fatigue and Weakness
Patients with ADHF often feel very tired and weak. The heart’s poor pumping means less blood to muscles and tissues. This makes it hard to do everyday tasks.
Orthopnea: Difficulty Breathing When Lying Flat
Orthopnea means trouble breathing when lying down. It’s because lying flat increases blood flow to the heart, making breathing harder. Patients often use pillows or sleep in a recliner to feel better.
Paroxysmal Nocturnal Dyspnea
Paroxysmal nocturnal dyspnea (PND) is sudden, severe night breathing trouble. It starts a few hours into sleep. PND is a serious sign of heart failure and needs quick medical help.
| Symptom | Description | Clinical Implication |
| Severe Shortness of Breath (Dyspnea) | Fluid accumulation in the lungs | Indicates pulmonary congestion |
| Fatigue and Weakness | Inadequate blood flow to muscles and tissues | Signifies reduced cardiac output |
| Orthopnea | Difficulty breathing when lying flat | Exacerbated by increased venous return |
| Paroxysmal Nocturnal Dyspnea | Sudden, severe shortness of breath at night | Sign of severe heart failure |
It’s vital for doctors to know these ADHF symptoms well. Quick diagnosis and treatment can greatly improve patient care. This can also lower the chance of serious problems.
3 Critical Physical Signs of ADHF Heart
Acute decompensated heart failure (ADHF) shows through key physical signs. Doctors must spot these signs fast. They show how bad heart failure is and help decide treatment.
We’ll look at the importance of swelling in legs, fluid in lungs, and bulging neck veins in ADHF.
Peripheral Edema and Leg Swelling
Swelling in legs, ankles, and feet is a big sign of ADHF. It happens when the heart can’t pump well, causing fluid to leak into tissues. Peripheral edema shows how serious heart failure is. Doctors check how bad the swelling is to see if treatment is working.
Pulmonary Congestion and Rales
Pulmonary congestion and rales are key signs of ADHF. Fluid builds up in lungs because the heart can’t circulate well. Pulmonary congestion and rales mean the patient might get worse respiratory problems. It’s important to treat these signs quickly to avoid more problems.
Jugular Venous Distension
Jugular venous distension (JVD) is a big sign in ADHF. It means the veins in the neck are too full. JVD shows the heart’s right side is under too much pressure. Seeing JVD means the patient needs help right away, as it could mean serious heart issues.
In short, spotting signs like swelling, fluid in lungs, and neck vein bulging is key for doctors. These signs help diagnose and manage ADHF. By acting fast on these signs, we can help patients with ADHF get better care.
Clinical Assessment and Diagnosis of Decompensated Cardiac Failure
Diagnosing ADHF is a detailed process. It includes clinical assessment and diagnostic testing. We will explain the key steps to help our readers understand how to evaluate patients with suspected ADHF.
Initial Patient Evaluation in Emergency Settings
When patients with suspected ADHF arrive in emergency settings, a quick evaluation is key. Rapid assessment helps make immediate decisions. We start with a detailed medical history and physical exam.
We look for symptoms like dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. A physical exam may show signs like peripheral edema, jugular venous distension, and pulmonary congestion. These signs help us understand the severity of the condition and guide further testing.
Diagnostic Tests and Laboratory Markers
Diagnostic tests are vital in confirming ADHF diagnosis. We use laboratory markers like natriuretic peptides (BNP or NT-proBNP) to support the diagnosis. High levels of these biomarkers are linked to heart failure.
| Diagnostic Test | Purpose |
| Electrocardiogram (ECG) | Assesses cardiac rhythm and detects ischemia or infarction |
| Chest X-ray | Evaluates pulmonary congestion and cardiac size |
| Echocardiogram | Assesses cardiac function and structure |
Other tests, like electrocardiogram (ECG), chest X-ray, and echocardiogram, give important information on cardiac function and possible causes of decompensation.
“The use of biomarkers, such as natriuretic peptides, has become an integral part of the diagnostic algorithm for heart failure.”
Source: NCBI Bookshelf
Imaging Studies for ADHF Confirmation
Imaging studies are key in confirming ADHF diagnosis and assessing cardiac structure and function. Echocardiography helps evaluate left ventricular function and detect causes of heart failure, like valvular disease or cardiomyopathy.
In some cases, cardiac MRI is used to further assess cardiac structure and function. The choice of imaging study depends on the patient’s clinical presentation and suspected cause of ADHF.
Emergency Management of Acute Decompensated Heart Failure
Managing acute decompensated heart failure in emergencies needs a detailed plan. This plan includes steps to stabilize patients and improve their health. It covers everything from the first steps to advanced monitoring of the heart’s function.
Initial Stabilization Measures
When patients with ADHF come in, they need quick help. This includes making sure they get enough oxygen, managing their symptoms, and improving their heart’s function. These first steps are key to stop things from getting worse.
We start with oxygen therapy to help increase oxygen levels and ease the heart’s work. For more serious cases, we might use non-invasive or mechanical ventilation to help with breathing.
Oxygen Therapy and Respiratory Support
Oxygen therapy is very important for ADHF patients, mainly those with low oxygen levels. Our goal is to keep oxygen levels high enough while avoiding too much carbon dioxide.
For those with very bad breathing problems, we might use NIPPV or mechanical ventilation. The choice depends on how bad their breathing is and how they react to oxygen therapy.
Hemodynamic Monitoring
Monitoring the heart’s function is critical in managing ADHF. It helps doctors see how well the heart is working, guide treatments, and check if things are getting better. We use different methods, both invasive and non-invasive.
Advanced monitoring helps tailor treatments to each patient. It helps manage fluids and improve blood flow to the heart.
Risk Stratification in the Emergency Department
It’s important to figure out the risk level of patients in the emergency room. This helps identify those at high risk of serious problems. We look at clinical signs, biomarkers, and other factors to understand how severe ADHF is.
Knowing the risk level helps us focus on the most important treatments. It also helps us use resources better and improve patient care.
| Risk Factors | Description | Implications for Management |
| Elevated Troponin Levels | Indicates myocardial injury | More aggressive management may be required |
| Hypotension | Signifies decreased cardiac output | Inotropic support or vasopressors may be needed |
| Severe Dyspnea | Reflects significant respiratory distress | Immediate oxygen therapy and possible ventilatory support |
Pharmacological Treatment Approaches for Acute Exacerbation of Heart Failure
Managing acute heart failure needs the right medicines. The choice of treatment depends on how severe the heart failure is. We’ll look at treatments like diuretics, vasodilators, beta blockers, and inotropic agents.
Intravenous Diuretics: Dosing and Administration
Intravenous diuretics are key for managing heart failure, mainly for those with too much fluid. Loop diuretics, like furosemide, are often used. The right dose and how to give it depends on the patient’s health and how much fluid they have.
- The first dose is based on what the patient has taken before.
- It’s important to check how well the diuretic is working to adjust the dose.
- Some patients might need a continuous infusion if bolus doses don’t work well.
Vasodilators in ADHF Management
Vasodilators are also important in treating heart failure, mainly for high blood pressure or when diuretics alone don’t work. Nitroglycerin and nitroprusside are examples of vasodilators used in heart failure. They help by reducing the heart’s workload and improving blood flow.
- Nitroglycerin is often the first choice because it starts working quickly and can be easily adjusted.
- Nitroprusside is used for those needing stronger vasodilation.
- It’s vital to watch the patient’s blood pressure and how they’re feeling while using vasodilators.
Beta Blocker Therapy in Acute Heart Failure
Beta blockers are important for long-term heart failure but are used with caution in the acute phase. For patients already on beta blockers, whether to continue or stop depends on the situation. Starting beta blockers in the acute phase is usually not recommended unless the patient is stable.
Inotropic Agents for Severe Cases
Inotropic agents like dobutamine and milrinone are for severe heart failure cases. They help the heart pump better and improve blood flow. But, they can also cause problems like irregular heartbeats and higher heart oxygen use.
Managing heart failure with medicines needs a careful and personalized approach. It’s important to consider the patient’s health, other conditions, and how they react to treatment. By knowing how to use diuretics, vasodilators, beta blockers, and inotropic agents, doctors can improve patient care.
Clinical Guidelines and Advanced Management Strategies
Managing acute decompensated heart failure (ADHF) needs a detailed plan. This plan includes the latest clinical guidelines and new treatments. Keeping up with these updates is key to giving our patients the best care.
Current Acute Decompensated Heart Failure Guidelines
The American College of Cardiology and the American Heart Association have set guidelines for ADHF. They suggest a team effort for diagnosis, risk assessment, and treatment. Each patient’s needs are considered carefully.
First steps in treatment include oxygen and breathing support. Doctors also use medicines like diuretics and vasodilators. These choices depend on the patient’s condition and how their heart is doing.
| Guideline Recommendation | Clinical Application |
| Early risk stratification | Identify high-risk patients for intensive monitoring |
| Intravenous diuretics | Relieve congestion and improve symptoms |
| Vasodilators | Reduce afterload and improve cardiac output |
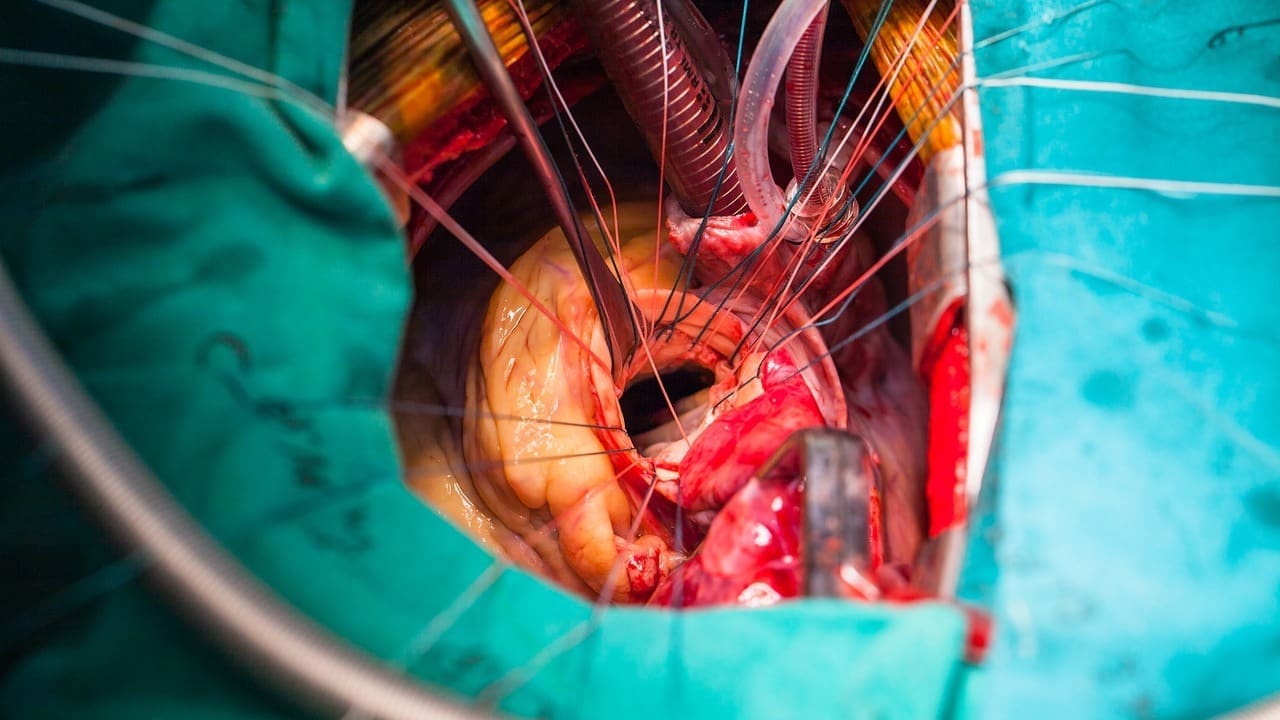
Mechanical Circulatory Support Options
For severe ADHF that doesn’t respond to first treatments, mechanical support is considered. Devices like intra-aortic balloon pumps (IABP) and left ventricular assist devices (LVAD) help the heart work better.
Mechanical Circulatory Support Devices:
- Intra-aortic balloon pump (IABP)
- Left ventricular assist device (LVAD)
- Extracorporeal membrane oxygenation (ECMO)
Specialized Care Units for ADHF Patients
Units like ICUs and heart failure units are vital for ADHF care. They offer the right setup for constant monitoring and advanced treatments. A team of experts works together to care for these patients.
“The management of acute decompensated heart failure requires a team-based approach, incorporating the expertise of cardiologists, intensivists, and other healthcare professionals.”
— American Heart Association
Liv Hospital’s Approach to ADHF Management
Liv Hospital follows the latest guidelines and uses advanced strategies for ADHF. Our team works together to give complete care, from the start to ongoing management.
We use mechanical support when needed and have specialized units for close care. Our goal is to offer top-notch healthcare and support to our international patients.
Conclusion: Improving Outcomes in Heart Failure Decompensation
Managing acute decompensated heart failure (ADHF) well is key to better patient results. We’ve talked about the main signs, symptoms, and treatment options for ADHF. It’s vital to act fast and give full care.
Liv Hospital is all in on top-notch care for ADHF patients. We use the latest clinical guidelines and treatments. Our goal is to make life better for those with heart failure through teamwork and advanced care.
Heart failure management means making lifestyle changes, taking medicines, and sometimes surgery. Health experts recommend these steps. We aim to boost ADHF outcomes with tailored care and the latest treatments, ensuring the best for our patients.
At Liv Hospital, we’re committed to leading in heart failure care. We use the newest medical science to help international patients get the best treatments.
FAQ
What is Acute Decompensated Heart Failure (ADHF)?
ADHF is when heart failure suddenly gets worse. It often needs emergency care or hospital stay.
What are the primary symptoms of ADHF?
Symptoms include severe shortness of breath, feeling very tired, and swelling in legs. These signs mean heart failure is getting worse and need quick doctor check-ups.
What are the critical physical signs of ADHF?
Signs include swelling in legs, breathing problems, and bulging neck veins. These show how serious heart failure is and help doctors decide what to do.
How is ADHF diagnosed?
Doctors first check patients in emergency rooms. Then, they use tests and scans to confirm ADHF.
What is the emergency management of ADHF?
First, doctors stabilize patients with oxygen and breathing help. They also watch heart function and decide how serious ADHF is.
What are the pharmacological treatment approaches for ADHF?
Treatment includes medicines like diuretics and beta blockers. Doctors choose based on how bad ADHF is.
What are the current guidelines for ADHF management?
Guidelines suggest a team approach. This includes using new treatments and special care units, like Liv Hospital, for better care.
What is the role of beta blockers in acute heart failure?
Beta blockers help manage acute heart failure. Doctors use them carefully, based on how severe ADHF is, to help patients get better.
What lifestyle factors contribute to ADHF decompensation?
Not taking medicine, bad diet, and not moving enough can make ADHF worse. Teaching patients about these helps prevent it.
What is the significance of risk stratification in ADHF management?
Knowing how bad ADHF is helps doctors decide the best treatment. This improves how well patients do
References
- Lung, K., & Lui, F. (2023). Anatomy, Abdomen and Pelvis: Arteries. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK525959/