Last Updated on October 21, 2025 by mcelik

At Liv Hospital, we know how urgent acute thrombosis is. It’s when a blood clot forms quickly, which can be very dangerous. A blood clot, or thrombus, blocks blood flow to important organs like the heart, lungs, and brain.
Clots in veins or arteries can cause big health problems. This includes acute embolism and thrombosis or acute deep vein thrombosis (DVT). Quick action and expert care are key to managing this condition well. We aim to give full care and support to those with acute thrombus and similar issues.
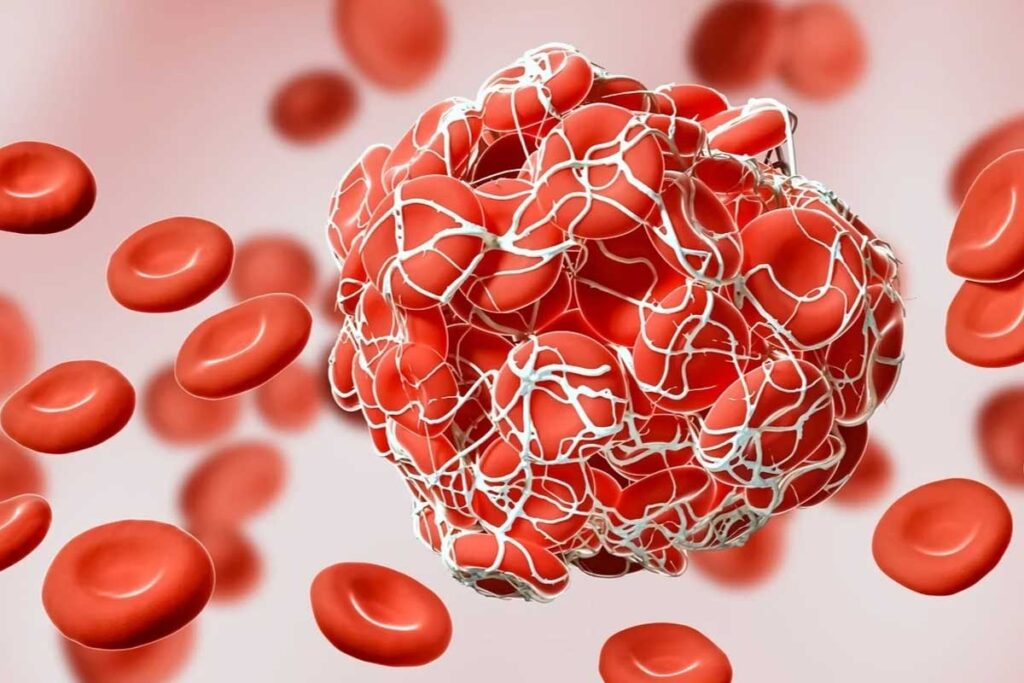
A blood clot in a vessel, known as acute thrombosis, is serious. It can harm health if not treated quickly. We will look into what it is and why it matters.
Acute thrombosis happens when a blood vessel gets damaged. The body tries to heal by forming a clot. But if the clot doesn’t dissolve or forms without reason, it’s bad. Studies show acute thrombosis can cause serious problems, like acute venous thromboembolism (VTE), if not treated quickly.
A fresh blood clot forms recently, usually in a short time. These clots can change, but they’re often easier to treat than older ones. We know acute thrombosis is more treatable than chronic clots, so acting fast is key.
The 14-day timeframe is key for acute thrombosis. It’s when the clot is most likely to respond to treatment. Research shows acting within this time can greatly help patients. We stress how vital this period is to stop things from getting worse.
Knowing the 14-day timeframe and what a fresh clot looks like is critical for doctors. By spotting acute thrombosis signs early, we can help patients better.
It’s important to know how acute blood clots form to prevent and treat them. These clots, or thrombi, happen when the body’s clotting gets out of balance. This imbalance is often caused by different risk factors.
The process of acute thrombus development is complex. It involves blood vessels, platelets, and clotting factors. When a blood vessel gets hurt, the body tries to stop bleeding by forming a clot.
But sometimes, this clotting can go wrong. This leads to an acute thrombus. Conditions like valvulitis or inflammation of a valve, aneurysm, leukemia, and factor V mutation can raise the risk of this happening.
Many things can cause acute clotting. These include genetic factors, lifestyle choices, and certain health conditions. Knowing these risk factors early helps us take steps to stop acute thrombosis.
Steps like anticoagulants and compression therapy can help. By understanding the risks and how they work, we can reduce the chance of acute blood clots.
Acute thrombosis can show different symptoms. Some are obvious, while others are not. It’s important to know these signs to get help quickly and avoid serious problems.
Pain, swelling, and redness are common signs of acute thrombosis. These happen because blood flow is blocked by a clot. Pain can feel dull or sharp and gets worse when you move. Swelling happens because of extra fluid, and redness is from inflammation. These symptoms can start suddenly or slowly.
For example, deep vein thrombosis (DVT) can make a leg swell, hurt, and feel warm. Watching for these signs is key, as they might mean a dangerous clot is present.
| Symptom | Description | Common Location |
| Pain | Dull ache to sharp pain | Leg, arm |
| Swelling | Fluid accumulation | Leg, arm |
| Redness | Inflammation | Leg, arm |
Not all acute thrombosis shows obvious symptoms. Some people might have silent symptoms or symptoms that are not typical. For instance, a pulmonary embolism might start with sudden chest pain or trouble breathing, without any leg symptoms first.
Other unusual symptoms can include stomach pain, nausea, or neurological issues if the clot is in different areas. Knowing about these different symptoms is important for catching the problem early.
In summary, while pain, swelling, and redness are clear signs of acute thrombosis, it’s also important to watch for silent or unusual symptoms. Quick action and medical help are key to managing acute thrombosis well.
A blood clot in the deep veins is known as acute DVT. It’s a serious condition that needs quick medical help. This clot forms suddenly in the deep veins, usually in the legs. If not treated fast, it can cause serious problems.
Acute DVT starts suddenly and has a clot in the deep veins. Symptoms include swelling, redness, tingling, tenderness, or warmth in the leg. These signs can be different for everyone and might not always show up.
Key characteristics of acute DVT include:
Acute DVT blocks blood flow due to a clot in the vein. This blockage can cause pain and swelling in the affected limb. A big clot can stop all blood flow, leading to serious tissue damage.
The blockage by acute DVT can lead to post-thrombotic syndrome. This is a condition with chronic pain, swelling, and skin color changes. Quick treatment is key to avoiding these issues and get blood flow back to normal.
Deep vein thrombosis can lead to a serious problem called acute embolism. A blood clot in the deep veins might break loose and travel through the blood. This can be very dangerous if the clot reaches important organs.
Not every blood clot turns into an embolism. But when it does, it’s a serious situation. The clot can go to different parts of the body, like the lungs, brain, or heart. This can cause a lot of damage or even death.
Turning from a stationary clot to a moving embolus is risky. When a clot breaks free, it can travel to smaller vessels. There, it might get stuck, causing an acute embolism.
This blockage can harm tissues or organs, depending on where it happens. For example, a clot in the lungs is a pulmonary embolism, which is a big emergency.
Things like not moving much, having a family history, or getting hurt can increase the risk of blood clots. Knowing these risks helps prevent and treat embolisms early.
A pulmonary embolism is a severe form of acute embolism. It happens when a clot blocks the arteries in the lungs. Symptoms include sudden shortness of breath, chest pain, and coughing up blood.
Other signs include a fast heart rate, feeling dizzy, and a sense of impending doom. If you or someone else has these symptoms, get help right away. Doctors use tests like CT scans to diagnose and treat pulmonary embolism.
When a blood clot blocks a vessel completely, it’s called occlusive thrombosis. This can lead to serious problems. We’ll look at what happens when a vessel is fully blocked and the risks to tissues.
Complete vessel occlusion happens when a clot blocks a blood vessel fully. This can cause a lot of damage because of the lack of blood flow. The damage’s severity depends on where and for how long the blockage lasts.
If a clot blocks an artery to the heart, it can cause a heart attack. A blockage in a brain artery can lead to a stroke. These are serious consequences that need quick medical help.
The damage from occlusive thrombosis can be very bad. It can cause tissue damage because of a lack of oxygen. This can lead to long-term disability or even death.
The risk and extent of tissue damage from occlusive thrombosis depend on several factors. These include where the blockage is and how long it lasts. The timeline for damage is different:
It’s important to understand these risks and timelines for quick diagnosis and treatment. We must recognize the symptoms of occlusive thrombosis and act fast to reduce damage.
It’s important to know the difference between acute and chronic Deep Vein Thrombosis (DVT) for the right treatment. The timing of symptoms and how they appear are key. These factors help tell acute from chronic DVT apart.
Figuring out if a DVT is new or old involves both doctors’ checks and imaging. Acute DVT shows up fast, with strong symptoms in days. On the other hand, chronic DVT might have milder or no symptoms because the body adapts over time.
Ultrasound is a key tool for spotting the difference. New clots are less solid and easier to push on, while old clots are firmer and harder to push. Old clots might also show signs of healing.
Treatment for DVT changes a lot depending on if it’s new or old. Acute DVT needs quick action with anticoagulant drugs to stop the clot from getting worse. Chronic DVT might focus on easing symptoms and stopping new clots, with more use of compression socks and long-term drugs.
Doctors need to understand these differences to give the best care. This helps patients get better and avoid serious problems.
Modern medicine has many effective treatments for acute thrombosis. These treatments help improve patient outcomes. The way we treat acute thrombosis has become more detailed. This shows how complex the condition is and how different patients’ needs are.
Anticoagulation therapy is key in managing acute thrombosis. It stops clots from growing and forming new ones. Anticoagulant medications can be taken by mouth or injected, based on the drug and the patient’s needs.
The right anticoagulant depends on several things. These include the patient’s kidney function, risk of bleeding, and other health conditions. Common anticoagulants are warfarin, apixaban, and rivaroxaban.
For more serious cases, interventional procedures and thrombolysis are options. Thrombolytic therapy uses drugs to break down clots. This helps restore blood flow. Thrombolysis is used for severe cases where there’s a high risk of organ damage or serious complications.
| Treatment Approach | Mechanism of Action | Indications |
| Anticoagulation Therapy | Inhibits clotting factors to prevent clot growth and formation | Primary treatment for acute thrombosis |
| Thrombolysis | Dissolves existing clots | Severe thrombosis with high risk of complications |
Managing acute thrombosis well needs a full plan. This includes medicines and sometimes procedures. Knowing all the treatment options helps doctors meet each patient’s unique needs.
“The timely and appropriate treatment of acute thrombosis is critical. It prevents long-term problems and improves patient results.”
— Cardiologist
Recent studies have greatly improved our understanding of acute venous thromboembolism. They show how vital early intervention is. Thanks to new research, we can now better manage this condition.
Research reveals that early action in treating acute venous thromboembolism greatly improves patient outcomes. Timely treatment cuts down on complications and boosts survival chances.
New and emerging therapies are being developed to further improve the treatment of acute venous thromboembolism. These include advanced anticoagulation therapies and innovative interventional procedures.
Some of the emerging trends in treatment protocols include:
After an acute thrombotic event, it’s key to have a solid prevention and management plan. This plan cuts down the chance of it happening again and helps manage the condition well.
Compression therapy is vital in stopping thrombosis from coming back. It uses compression stockings to boost blood flow and lessen swelling. Physical activity guidelines suggest doing regular exercise to improve circulation. But, it’s important to not overdo it. Patients should talk to their doctor to create a workout plan that fits them.
Keeping an eye on things long-term is key to spotting problems early. Regular check-ups with healthcare providers help tweak treatment plans as needed. Recurrence prevention strategies include sticking to anticoagulation therapy and making lifestyle changes. This includes keeping a healthy weight and not staying immobile for too long.
Acute thrombosis is a serious condition that needs quick action. Blood clots are normal for healing, but they can be dangerous. They can block blood flow to vital organs if they form in veins or arteries.
We’ve talked about acute thrombosis, including its symptoms and treatment. We’ve also covered the differences between acute and chronic conditions. Understanding how acute thrombus forms and the risk factors is key.
Managing acute thrombosis means getting medical help fast. Treatments like anticoagulation therapy and interventional procedures are vital. We also discussed the importance of prevention and managing after an event, like using compression therapy and following physical activity guidelines.
In summary, acute thrombosis requires attention to symptoms, timely treatment, and prevention. By knowing the risks and taking steps to prevent them, we can lower the risk of complications. This improves patient outcomes.
Acute thrombosis is when a blood clot forms inside a blood vessel. This can block blood flow and cause serious problems if not treated quickly.
Signs of acute thrombosis include pain, swelling, and redness in the affected limb. These happen because the clot blocks blood flow and causes inflammation.
Acute DVT is a new blood clot in the deep veins, usually within 14 days. Chronic DVT is an older clot that can cause long-term vein damage.
Occlusive thrombosis is when a blood clot blocks a blood vessel completely. This stops blood flow to the tissues downstream, leading to damage and serious complications.
Treatment for acute thrombosis includes anticoagulation therapy to stop the clot from growing. Sometimes, procedures like thrombolysis or thrombectomy are needed to remove the clot.
Risk factors include immobility, surgery, trauma, cancer, and genetic conditions like factor V Leiden or antiphospholipid syndrome.
Yes, preventing acute thrombosis is possible. Measures include regular exercise, compression therapy, and anticoagulant prophylaxis for those at high risk.
The 14-day timeframe is important because it’s when a blood clot is most likely to respond to treatment. After 14 days, the clot may become more chronic.
Symptoms of pulmonary embolism include sudden shortness of breath, chest pain, and coughing up blood. These happen when a clot blocks blood flow in the lungs.
Diagnosis involves imaging studies like ultrasound or CT scans, along with clinical evaluation and lab tests to check for clotting disorders.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us