after brain surgery headaches
Nearly 30,000 brain operations are done every year in the United States. This shows how common and complex these surgeries are.
Brain surgery is a big deal in medicine. It uses special techniques and can have risks. We need to understand its effects, like headaches after brain surgery.
When we talk about major surgery like brain surgery, we must cover the worries and problems. This includes headaches after surgery. We aim to help those going through this big medical step.
Key Takeaways
- Brain surgery is a complex and significant medical procedure.
- Understanding the risks and complications is crucial for patients.
- Headaches after brain surgery are a concern that needs to be addressed.
- Major surgery like brain operations requires comprehensive care and support.
- Patients undergoing brain surgery need to be aware of the potential outcomes.
Understanding Brain Surgery: Definition and Types
a realistic medical diagram depicting various types of brain surgery procedures, including craniotomy, stereotactic surgery, endoscopic surgery, and minimally invasive techniques. The image should show detailed cross-sections of the human skull and brain, highlighting the different surgical approaches and tools used, such as scalpels, retractors, and microscopes. The composition should be clean, well-lit, and utilize a neutral color palette to convey a sense of medical precision and professionalism, suitable for an educational article on the subject of brain surgery.
Brain surgery is a wide term for many surgical procedures. These are done to diagnose or treat brain disorders. It’s a complex field that needs precision, skill, and a deep understanding of the brain.
Common Types of Brain Surgeries
There are many types of brain surgeries, each for different conditions. Some common ones include:
- Craniotomy: A procedure where part of the skull is temporarily removed. This allows surgeons to access the brain.
- Neuroendoscopy: A minimally invasive technique. It uses a small camera and instruments through tiny incisions to perform surgery within the brain.
- Endovascular Surgery: Procedures that involve operating on blood vessels within the brain. This is often used to treat conditions like aneurysms.
Reasons Brain Surgery Is Performed
Brain surgery is done for many reasons. This includes removing tumors, relieving pressure on the brain, repairing blood vessels, and treating certain neurological conditions. The decision to have brain surgery is made after other treatments are tried. It’s based on a thorough evaluation of the patient’s condition and overall health.
We know that brain surgery can be scary. But knowing what to expect can help ease some of the anxiety. Our team is dedicated to providing comprehensive care and support. We ensure that patients get the best possible outcomes.
Why Brain Surgery Is Classified as Major Surgery
High-angle close-up view of a human brain with intricate neural networks, surrounded by surgical instruments and a sterile medical environment. Illuminated by bright, focused lighting to highlight the complexity of the brain’s internal structures. Tones are cool and clinical, conveying the precision and gravity of the procedure. Depth of field is shallow, drawing the viewer’s attention to the delicate, intricate details of the brain anatomy. Atmospheric elements like steam or condensation add a sense of technical sophistication. Emphasize the technical challenges and high stakes involved in performing brain surgery.
Brain surgery is considered major because it’s complex and risky. It affects the patient’s body deeply. This is due to the intricate nature of brain operations.
Criteria for Classifying Surgical Procedures
Surgeries are classified based on complexity, risk, and post-op care needs. Brain surgery meets these criteria because of its delicate nature and critical functions.
We call surgeries major based on several factors. These include the level of invasion, the body area affected, and the risks involved. Brain surgery is major because it requires opening the skull, a highly invasive procedure.
Risk Factors and Complexity
Brain surgery comes with significant risks like damage to brain tissue and infection. The brain’s complex structure and function make it challenging. Neurosurgeons need specialized training and expertise.
The table below shows some key risks and complexities of brain surgery:
Risk Factor/Complexity | Description | Mitigation Strategy |
Infection | Risk of infection at the surgical site or within the brain | Use of antibiotics, sterile surgical techniques |
Brain Swelling | Potential for swelling around the surgical site | Corticosteroids, careful monitoring |
Seizures | Risk of seizures during or after surgery | Anti-seizure medications, EEG monitoring |
Impact on Body Systems
Brain surgery can affect many body systems, depending on the brain area involved. It can impact motor functions, cognitive abilities, and emotional regulation.
Post-operative care is key to managing these impacts. It includes monitoring for complications, rehabilitation, and support for cognitive and emotional challenges.
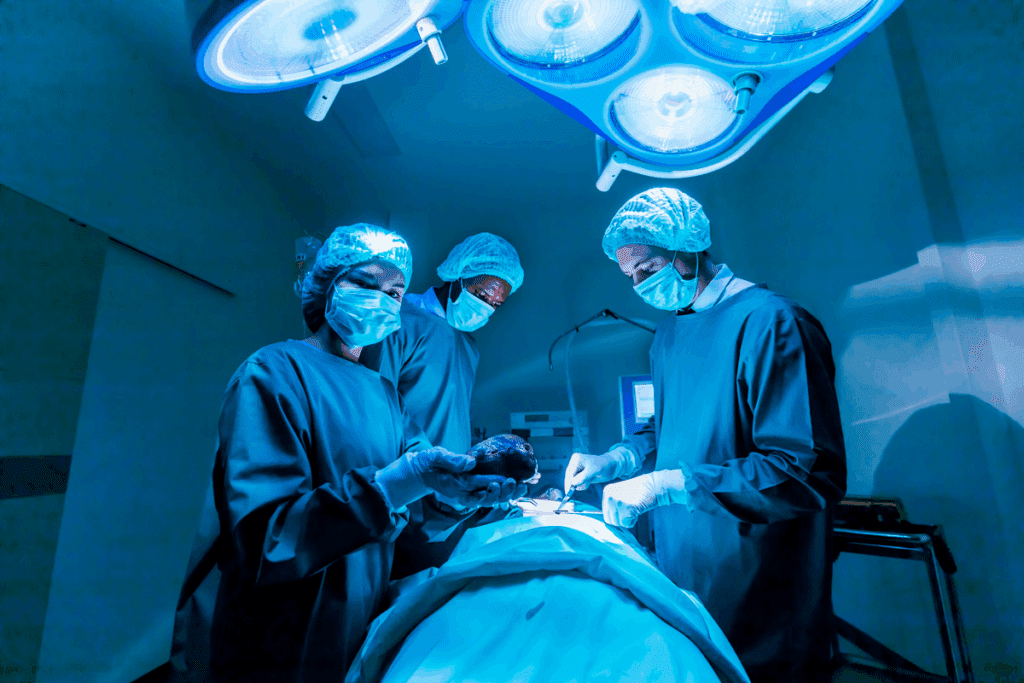
The Brain Surgery Procedure: What to Expect
A sterile operating room filled with state-of-the-art medical equipment, bathed in soft, indirect lighting. In the foreground, a team of skilled neurosurgeons meticulously perform a delicate brain surgery procedure, their hands moving with precision as they navigate the intricate folds of the patient’s brain. The patient’s head is carefully positioned, with a high-magnification microscope providing a clear, detailed view of the surgical site. In the background, various diagnostic monitors display real-time data, while the atmosphere conveys a sense of focus, concentration, and the gravity of the task at hand.
Brain surgery is a detailed process. It includes getting ready before surgery, the surgery itself, and care after. Knowing what to expect can help ease worries and prepare patients.
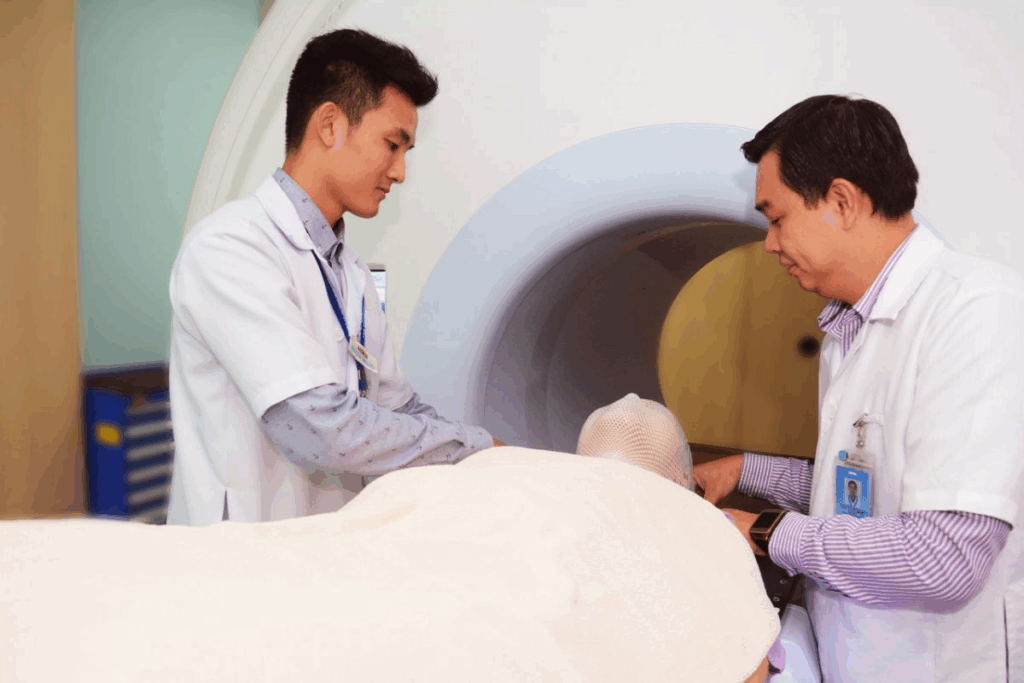
Pre-Surgical Preparation and Testing
Before brain surgery, patients go through a lot of preparation and tests. They have medical checks, imaging like MRI or CT scans, and talks with their healthcare team. Pre-surgical testing is key to spotting risks and making a plan just for them.
Patients also get advice on how to get ready for surgery. This includes changing medications, following diet rules, and making lifestyle changes. It’s very important to follow these steps to reduce risks and make the surgery go smoothly.
Anesthesia and Surgical Techniques
During brain surgery, anesthesia keeps the patient comfortable and pain-free. The type of anesthesia depends on the surgery and the patient’s health. Our skilled anesthesiologists work with the surgical team to keep an eye on the patient’s health and adjust anesthesia as needed.
The surgery uses special techniques and tools. Neurosurgeons use these advanced methods to protect the brain and get the best results.
Immediate Post-Operative Care
After surgery, patients go to the ICU for close care. The team watches for any problems and manages pain well. Immediate care after surgery is crucial for a smooth recovery and dealing with any issues quickly.
Patients and their families are kept updated on the patient’s status and post-operative instructions. Following these instructions is key for a good recovery and avoiding complications.
How Long Does Brain Surgery Take?
A highly detailed medical operation theater, bathed in bright surgical lighting. The operating table is the focal point, with a patient’s head exposed, surrounded by a team of skilled neurosurgeons performing delicate brain surgery. The scene conveys the intense focus and concentration required for this complex procedure, with various medical instruments and equipment visible in the foreground and middle ground. The background features the sterile, clinical environment of the operating room, with muted tones and minimal distractions to emphasize the gravity of the situation. The overall mood is one of professionalism, precision, and the critical importance of this life-saving surgery.
The time needed for brain surgery varies. It depends on the surgery’s complexity and the patient’s health.
Factors Affecting Surgery Duration
Several factors can influence brain surgery time. These include:
- The type of surgical procedure being performed
- The complexity of the condition being treated
- The patient’s overall health and age
- The surgical team’s experience and efficiency
Surgery duration can vary significantly. It can range from a few hours for simpler procedures to more than 12 hours for complex operations.
Type of Brain Surgery | Typical Duration |
Craniotomy for Tumor Removal | 4-8 hours |
Aneurysm Clipping | 4-6 hours |
Deep Brain Stimulation | 2-4 hours |
Recovery Time in the Hospital
Recovery time in the hospital varies after brain surgery. Generally, patients stay for:
- 1-3 days for less complex procedures
- 3-7 days or more for complex surgeries or if complications arise
The hospital stay lets medical staff watch over the patient. They manage pain and address any complications quickly.
Knowing what affects surgery and recovery time helps. It prepares patients and their families, reducing anxiety and improving outcomes.
The Cost of Brain Surgery in the United States
A detailed medical office with modern equipment and supplies, illuminated by a warm, focused lighting that casts dramatic shadows. In the foreground, a high-tech brain imaging display showcases intricate neural pathways. The middle ground features a sleek, high-precision surgical robot, conveying the advanced technology involved in brain procedures. In the background, a panoramic view of a bustling city skyline, hinting at the urban setting and the specialized expertise required for such a complex operation. The overall atmosphere exudes a sense of professionalism, innovation, and the gravity of the medical challenge at hand.
It’s important for patients and their families to know the cost of brain surgery. The price can change a lot, depending on where you are, who does the surgery, and your insurance.
Average Costs and Insurance Considerations
The cost of brain surgery can be from $50,000 to over $100,000. This depends on how complex the surgery is and how long you stay in the hospital. Insurance is a big help in covering these costs.
Insurance Considerations:
- Make sure your insurance covers the brain surgery you need.
- Know what you’ll have to pay out of pocket, like deductibles and co-payments.
- Find out if your insurance needs you to get approval for the surgery first.
Financial Resources and Support Programs
There are many ways to help with the cost of brain surgery. These include:
Resource | Description |
Patient Assistance Programs | Hospitals and non-profits offer help with surgery costs. |
Government Programs | Medicaid and Medicare can help with costs for some patients. |
Fundraising | Crowdfunding can be used to raise money for surgery. |
How Neurological Surgeon Fees Impact Costs
The fees for neurological surgeons can greatly affect the cost of brain surgery. These fees change based on the surgeon’s experience, where they are, and how complex the surgery is.
Understanding what affects the cost of brain surgery and looking into financial help can make a big difference. This way, patients can handle the financial side of their care better.
Brain Surgery Recovery Timeline
A detailed series of medical illustrations showcasing the stages of brain surgery recovery, from the initial incision to the final healing process. The foreground depicts the surgical site, with delicate sutures and bandages, while the middle ground shows the patient’s gradual progress, from resting in a hospital bed to engaging in gentle exercises. The background features a serene, clinical environment, with medical equipment and a soothing color palette. The overall mood is one of professionalism and reassurance, conveying the expertise and care required for a successful brain surgery recovery.
Recovering from brain surgery takes time, patience, and a good plan. The recovery time varies for everyone. It depends on the surgery type, health, and age. We’ll explain what to expect in each stage of recovery.
First Week After Surgery
The first week is very important and often involves staying in the hospital. Doctors watch for any problems and manage pain. Rest is key, and patients might feel tired, have headaches, and feel confused or disoriented.
First Month of Recovery
In the first month, patients start to feel stronger. They need to see their neurosurgeon often to check on healing. They might still have headaches or feel tired, but these symptoms usually lessen. They can start doing light things, but should avoid hard activities.
Three to Six Months Post-Surgery
By three to six months, most people see big improvements. They can usually go back to their usual life, but should still avoid heavy work. Their thinking skills also get better, and some might need extra help.
Long-Term Recovery Expectations
Long-term recovery can be different for everyone. Some might fully recover in a year, while others face ongoing challenges. It’s important to keep seeing doctors to manage any lasting effects and adjust treatment plans.
Recovery Stage | Typical Symptoms/Activities | Expected Progress |
First Week | Fatigue, headaches, hospital stay | Initial recovery, pain management |
First Month | Gradual strength regain, follow-up appointments | Symptom reduction, resuming light activities |
Three to Six Months | Returning to normal activities, avoiding strenuous tasks | Significant improvement, cognitive function enhancement |
Long-Term | Varies by individual, potential for full recovery | Ongoing management, potential for full or significant recovery |
Knowing the recovery timeline after brain surgery helps patients and their families prepare. While it’s tough, understanding what’s ahead can help manage recovery better.
20 Things to Expect After Brain Surgery
A person lying in a hospital bed, their head wrapped in bandages, with visible stitches or staples along the incision line. The expression on their face conveys a mix of discomfort, fatigue, and concern. The lighting is soft and natural, casting gentle shadows that emphasize the changes to their appearance. The background is a sterile, clinical hospital environment, with medical equipment and supplies visible in the periphery. The overall mood is one of introspection and the gravity of the situation, conveying the significant physical and emotional impact of undergoing brain surgery.
Knowing what to expect after brain surgery can make recovery easier. It’s important to understand the physical, cognitive, and emotional changes that might happen.
Physical Changes and Challenges
Patients often face physical changes after brain surgery. These can include:
- Headaches and swelling
- Numbness or tingling sensations
- Weakness in certain parts of the body
- Changes in vision or hearing
- Fatigue and general feeling of being unwell
- Pain at the surgical site
- Nausea and vomiting
The intensity and length of these changes depend on the surgery type and the patient.
Cognitive and Emotional Effects
Brain surgery can also affect how we think and feel. Patients might notice:
- Memory issues or difficulty concentrating
- Mood swings or irritability
- Anxiety or depression
- Difficulty with speech or language processing
- Changes in personality
- Confusion or disorientation
These effects are usually short-term but can be tough. Getting support from doctors and loved ones is key.
Lifestyle Adjustments and Restrictions
Recovery requires some lifestyle changes. Patients might need to:
- Avoid heavy lifting or bending
- Limit driving or operating heavy machinery
- Adjust their work schedule or take a temporary leave
- Avoid strenuous activities or exercise
- Follow a specific diet or nutrition plan
- Attend follow-up appointments with their healthcare provider
Understanding these changes helps patients prepare for recovery after brain surgery.
Recovering from brain surgery needs patience, support, and knowledge. Knowing about physical, cognitive, and emotional changes helps patients manage their recovery better.
After Brain Surgery Headaches: Causes and Patterns
Headaches after brain surgery are common and need to be understood. Knowing what causes them is key to managing them. We’ll look at the many factors that lead to these headaches.
Types of Post-Craniotomy Headaches
There are different types of headaches after brain surgery. Acute post-craniotomy headaches happen right after surgery. They can be due to tissue damage, swelling, or the body’s reaction to surgery.
Chronic post-craniotomy headaches last longer. They can be affected by many things, like the patient’s past headaches, the surgery’s extent, and complications after surgery.
When Headaches Are Normal vs. Concerning
Some headaches after brain surgery are normal. But, it’s important to tell the difference between normal discomfort and signs of trouble. Mild to moderate headaches that get better are usually okay.
Severe, getting worse, or lasting headaches might mean there’s a problem like infection or bleeding. It’s vital to watch how bad your headaches are and tell your doctor if they’re concerning.
The Relationship Between Anesthesia and Headaches
Anesthesia is a big part of brain surgery. It’s not the main cause of headaches after surgery. But, how anesthesia is given and how you recover from it can lead to headaches in some people.
The type of anesthesia, how long it lasts, and how you react to it can affect headaches. Knowing this helps in planning care after surgery.
Managing and Treating Headaches After Brain Surgery
Managing headaches after brain surgery is key to recovery. It involves medical treatments, non-pharmaceutical strategies, and lifestyle changes. Knowing these options can help patients feel better and live better during recovery.
Medical Treatments for Post-Surgical Headaches
Medical treatments are crucial for managing post-surgical headaches. Medications like acetaminophen or ibuprofen are often used to ease symptoms. Sometimes, stronger pain meds are needed for severe headaches. Always follow your doctor’s dosage advice to avoid side effects.
Preventive medications may also be given to lessen headache frequency and severity. These can include beta-blockers, anticonvulsants, or antidepressants, based on the headache cause.
Non-Pharmaceutical Pain Management Strategies
Non-pharmaceutical methods can add to medical treatments and offer more relief. Relaxation techniques like deep breathing, meditation, or yoga can help reduce stress and ease headaches. Using cold or warm compresses on the forehead or neck can also help.
Moreover, cognitive behavioral therapy (CBT) can help manage stress and develop coping strategies for headache pain. It aims to change negative thought patterns and behaviors that may lead to more headaches.
Lifestyle Modifications to Reduce Headache Frequency
Changing your lifestyle can also help reduce post-surgical headaches. Keeping a regular sleep schedule and getting enough rest can prevent headaches. Drinking plenty of water and eating a balanced diet are also important.
Avoiding triggers like bright lights, loud noises, or strong smells can also reduce headache frequency. Regular exercise, like walking or gentle activities, can improve well-being and lessen headaches.
Long-Term Side Effects of Craniotomy and Brain Operations
It’s important to know the long-term side effects of brain surgery. Craniotomy and other brain operations can affect patients’ health in many ways. This includes their brain, body, and mind.
Neurological Side Effects
Neurological side effects can differ for each patient. Some common issues include:
- Seizures: Patients might have seizures because of the surgery or their condition.
- Cognitive Changes: They might have trouble remembering things or focusing.
- Motor Function Impairment: They could experience weakness, numbness, or paralysis.
One study found that neurological problems after craniotomy are a big worry for doctors and patients.
“Neurological complications can arise from the surgery itself or from the underlying pathology… careful preoperative planning and postoperative care can mitigate some of these risks.”
Physical Side Effects
Physical side effects can also be tough. They might include:
Side Effect | Description |
Fatigue | Prolonged tiredness that can last for weeks or months after surgery. |
Pain | Headaches or pain at the surgical site can be a persistent issue. |
Infection | Risk of infection at the surgical site or within the brain. |
Psychological Impact and Coping Strategies
The mental effects of brain surgery are significant. Patients might feel anxious, depressed, or have mood swings. It’s key for them to get psychological support and counseling.
Effective coping strategies include:
- Seeking support from family and friends.
- Engaging in stress-reducing activities like meditation or yoga.
- Joining support groups for those who have had similar surgeries.
We know that every patient’s experience is different. Understanding these potential long-term side effects helps patients and their families prepare for what’s ahead.
Life After Brain Tumor Removal: What to Know
Life after brain tumor removal is unique for everyone. It depends on the tumor type and the patient’s health. Knowing what to expect can help with the healing process.
Physical and Cognitive Rehabilitation
Rehabilitation is key to getting back on track. Physical therapy helps with movement and strength. Cognitive rehabilitation focuses on memory and concentration.
Every patient is different, so rehabilitation plans are made just for them. This ensures the best care possible.
Occupational therapy helps with daily tasks and independence. Our team works with patients and families for a full recovery plan.
Follow-up Care and Monitoring
Follow-up care is crucial for tracking progress and catching any problems early. Regular visits with healthcare providers are important. They help ensure the patient stays on the right path.
These visits might include tests like MRI or CT scans. They check for tumor signs. Our team also looks at the patient’s overall health, offering advice on managing symptoms.
Adjusting to the “New Normal”
Adjusting to life after surgery is more than physical. It’s about adapting to a new reality. Patients may need to change their work, social life, and routines. We help them find ways to keep living well.
Emotional and psychological support are also key. Support groups, counseling, or mental health professionals can help. They provide the tools to deal with emotional challenges.
When to Contact Your Neurological Surgeon After Surgery
It’s crucial to know when to reach out to your neurological surgeon after surgery. After brain surgery, it’s important for patients and their caregivers to watch their recovery closely.
Warning Signs That Require Immediate Attention
Some symptoms can mean complications after brain surgery. If you notice any of these, call your neurological surgeon right away:
- Severe headache that doesn’t get better with medicine
- Confusion or disorientation
- Weakness or numbness in any part of your body
- Seizures or convulsions
- Fever over 101.5°F (38.6°C)
- Infection signs at the surgical site, like redness, swelling, or drainage
- Difficulty speaking or understanding speech
- Vision changes, such as double vision or loss of vision
Knowing these warning signs can help you get medical help quickly. This might prevent serious problems.
Scheduled Follow-ups and Their Importance
Seeing your neurological surgeon after surgery is very important. These visits help your surgeon:
- Check how you’re recovering
- Look for any signs of complications
- Change your treatment plan if needed
- Answer any questions or concerns you have
To get the most from these visits, keep a record of your symptoms, medicines, and questions.
Follow-up Care Aspect | Description | Importance |
Monitoring Recovery | Regular check-ups to assess healing and recovery | High |
Complication Detection | Early identification of potential complications | High |
Treatment Adjustments | Modifying treatment plans based on recovery progress | Medium |
Patient Support | Addressing patient concerns and questions | High |
Questions to Ask During Post-Operative Appointments
Don’t be shy to ask questions during your follow-up visits. Some good ones include:
- What are the expected outcomes of my surgery?
- Are there any specific signs of complications I should watch for?
- How should I manage my pain or discomfort?
- Are there any activities I should avoid or modify?
- What is the plan for my long-term care and follow-up?
Asking these questions helps you understand your recovery better. It also tells you what to expect after surgery.
Conclusion: The Journey of Healing from Brain Surgery
The journey to heal from brain surgery is complex. It involves the surgery itself, getting ready for it, caring for yourself after, and recovering for a long time. Understanding brain surgery and its effects is key for patients and their families.
Our recovery path includes dealing with physical, mental, and emotional changes. Knowing what to expect helps us move forward. We stress the need for full care and support to help patients recover well.
Recovering from brain surgery takes time, strength, and a caring community. Recognizing the journey’s complexity helps us prepare for its ups and downs. As we get better, we can regain our strength and improve our health.
FAQ
What is brain surgery and why is it considered major surgery?
Brain surgery, also known as neurosurgery, treats brain disorders or injuries. It’s major because it’s complex, risky, and affects many body systems.
What are the common types of brain surgeries?
Common surgeries include craniotomy, neuroendoscopy, and tumor surgery. These treat conditions like tumors, aneurysms, and brain injuries.
How long does brain surgery typically take?
Surgery time varies by procedure complexity, patient condition, and surgeon experience. It can last from a few hours to several hours.
What can I expect during the recovery process after brain surgery?
Recovery brings physical, cognitive, and emotional changes. You’ll need lifestyle adjustments. Recovery time is different for everyone, but it usually takes days to weeks in the hospital and months at home.
Why do I experience headaches after brain surgery?
Headaches can come from the surgery, anesthesia, or swelling. The type and severity vary. Always talk to your surgeon about your headaches.
How can I manage and treat headaches after brain surgery?
Treatments include medication, pain management strategies, and lifestyle changes. Your surgeon will suggest the best treatment for you.
What are the potential long-term side effects of craniotomy and brain operations?
Long-term effects can include neurological, physical, and psychological impacts. Discuss these with your surgeon and follow their care advice.
How much does brain surgery cost in the United States?
Costs vary by procedure, location, and insurance. Brain surgery is often expensive. Talk to your healthcare provider about financial help.
When should I contact my neurological surgeon after surgery?
Contact your surgeon for severe headaches, confusion, or weakness. Regular follow-ups are also important for monitoring your recovery.
What are the 20 things to expect after brain surgery?
Expect physical, cognitive, and emotional changes, along with lifestyle adjustments. Common experiences include fatigue, pain, and cognitive changes. Your surgeon can guide you through recovery.
How can I cope with the psychological impact of brain surgery?
Use counseling, support groups, and lifestyle changes to cope. Your healthcare provider can recommend resources for mental health support.
What is the typical recovery timeline for brain surgery patients?
Recovery time varies, but most spend days to weeks in the hospital and months at home. Your surgeon can give you a personalized timeline.
How can I adjust to life after brain tumor removal?
Adjust by focusing on physical and cognitive rehabilitation, follow-up care, and lifestyle changes. Your healthcare provider can help you navigate this new reality.
What are the signs that I should seek immediate medical attention after brain surgery?
Seek immediate help for severe headaches, confusion, weakness, or cognitive changes. Contact your surgeon or go to the emergency room if you notice these symptoms.
How can I manage dizziness after brain surgery?
Manage dizziness with rest, hydration, and avoiding strenuous activities. Your surgeon can suggest more strategies to help.
What are the available financial resources and support programs for brain surgery patients?
Financial help includes insurance, government programs, and non-profit organizations. Your healthcare provider can help you find the best resources for your situation.
References
World Health Organization. Postoperative Headaches After Brain Surgery Prevalence and Management. Retrieved from https://www.who.int/publications/i/item/9789240051997









