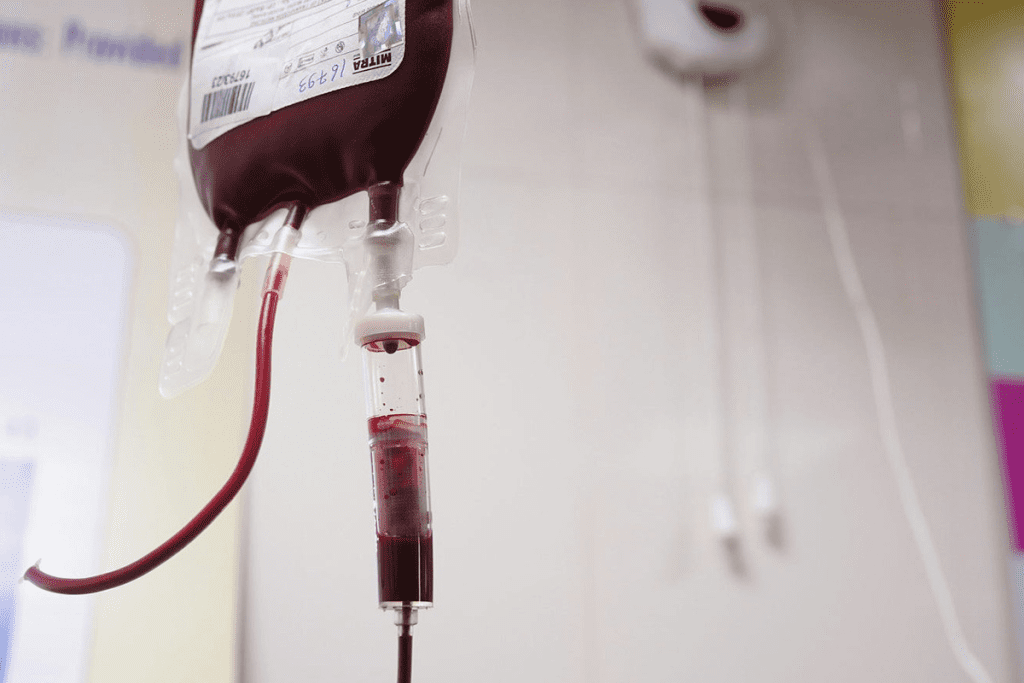
Healthcare is moving towards new solutions because of the limitations and dangers. The need for safer and better options is growing. This is due to blood shortages, matching issues, and contamination risks.
The market for artificial blood substitutes is big and getting bigger. It’s valued at $1.355 billion in 2024 and could hit $5.265 billion by 2035. This shows a big leap in patient safety and care quality with new blood management tech.
Key Takeaways
- The global market for artificial blood substitutes is experiencing significant growth.
- Traditional blood transfusions are associated with several risks and limitations.
- Innovative alternatives are being developed to address these challenges.
- Advanced blood management technologies are improving patient safety and care quality.
- The demand for safer and more effective transfusion alternatives is on the rise.
The Growing Need for Alternatives to Blood Transfusion
Traditional blood transfusions face shortages and compatibility issues. This has made alternatives more important than ever. New solutions are needed to overcome these challenges.
The market for blood transfusion alternatives is booming. It’s expected to reach $13.76 billion by 2029. This shows how fast this field is growing. The market will jump from $1.355 billion in 2024 to $5.265 billion by 2035, a big leap in investment.
Market Growth: $1.355 Billion in 2024 to $5.265 Billion by 2035
Several factors are driving the need for blood transfusion alternatives:
- More surgeries and trauma cases need transfusions.
- People are learning about the risks of traditional blood transfusions.
- New technology is creating safer, more effective options.

Addressing Shortages, Compatibility Issues, and Contamination Risks
Traditional blood transfusions have their own set of problems:
- There’s often a shortage of specific blood types, which is critical in emergencies.
- Compatibility issues can cause serious reactions.
- There’s a risk of contamination, including infectious diseases.
These issues have led to the creation of new alternatives. By investing in alternatives to blood transfusions, we can better care for patients. This also makes healthcare systems more efficient.
Hemoglobin-Based Oxygen Carriers (HBOCs)
Hemoglobin-based oxygen carriers (HBOCs) are emerging as a key alternative to blood transfusions in emergencies. They are made to carry oxygen like red blood cells do. This makes them useful for many medical needs.
Oxygen Transport Mechanism
HBOCs are made by changing hemoglobin from red blood cells. This change lets them carry oxygen well. They don’t need to be kept cold and work with all blood types, making them easy to use in emergencies.
These carriers work by using special hemoglobin that binds and releases oxygen. This is key for keeping tissues oxygenated in cases of blood loss or oxygen delivery issues.
Current Products and Clinical Applications
Many HBOC products are being developed or used now. They aim to deliver oxygen effectively. They are used in trauma care, surgeries, and when a lot of blood is needed.
For more info on HBOCs’ safety and how well they work, the FDA has lots of resources.
| Product | Clinical Application | Status |
| HBOC-201 | Trauma Care, Surgical Procedures | In Clinical Trials |
| PolyHeme | Emergency Resuscitation | Under Review |
| MP4 | Surgical Procedures | Approved in Some Countries |
HBOCs are a big step forward in transfusion medicine. They offer a new way to help patients in critical care situations.
Perfluorocarbon Emulsions: Synthetic Oxygen Carriers
Perfluorocarbon emulsions are being studied as a synthetic oxygen carrier. They could help transport oxygen, reducing the need for blood transfusions.
Mechanism of Action and Oxygen Delivery Capacity
These emulsions carry oxygen through the bloodstream. Their ability to deliver oxygen is key to their use as transfusion alternatives. They work by dissolving oxygen, which is then released to tissues.
The oxygen delivery capacity of perfluorocarbon emulsions depends on the type of perfluorocarbon and the emulsion’s concentration. Researchers are working to improve these factors.
Current Development Status
Perfluorocarbon emulsions are being developed as synthetic oxygen carriers. They show promise but also have complex side effects that researchers are trying to address.
Improving stability, reducing side effects, and scaling up production are the main challenges. Despite these hurdles, perfluorocarbon emulsions are a promising option for alternatives to blood transfusion.
As we continue to study and develop perfluorocarbon emulsions, their role as transfusion alternatives grows. Ongoing research and clinical trials are bringing us closer to their clinical use.
Advanced Platelet Management Technologies
Breakthroughs in platelet management are tackling old problems. These include supply, storage, and compatibility issues in transfusion medicine. These advancements are key to ensuring patients get the platelet transfusions they need quickly.
Lower-Dose Platelet Protocols
One big step forward is the use of lower-dose platelet protocols. Research shows these protocols can boost platelet supply by up to 23%. By adjusting the dosage, we can use the platelets we have more efficiently. This helps ease the pressure on blood banks.
Cold-Stored Platelets
Cold-stored platelets are another important innovation. Traditional storage at room temperature for up to 5 days limits platelet availability. Cold storage extends shelf life, making platelet management more flexible and reducing waste.
Freeze-Dried and Split-Unit Platelet Innovations
Researchers are also exploring freeze-dried and split-unit platelet technologies. Freeze-drying could change how we store and transport platelets, making them more accessible in remote areas. Split-unit platelets allow for more precise dosing, meeting patient needs better, and improving inventory management.
These new technologies in platelet management are changing transfusion medicine. They improve platelet availability, storage, and compatibility. This leads to better patient care and outcomes.
| Technology | Description | Benefits |
| Lower-Dose Platelet Protocols | Optimizing platelet dosage for transfusions | Increased supply by up to 23% |
| Cold-Stored Platelets | Storing platelets at cold temperatures | Extended shelf life, reduced waste |
| Freeze-Dried Platelets | Freeze-drying platelets for storage | Improved storage, transportation, and accessibility |
Blood Recovery and Autologous Transfusion Systems
Autologous transfusion systems and blood recovery technologies are changing transfusion medicine. They help reduce the need for donor blood. This is important because traditional blood transfusions can have problems like compatibility issues and the risk of infectious diseases.
We are seeing a big change towards better blood management, mainly in surgeries. Blood loss is a big worry in these situations. Blood recovery and autologous transfusion systems offer a safer and more reliable option.
Intraoperative Cell Salvage Technology
Intraoperative cell salvage technology collects, processes, and reinfuses a patient’s own blood lost during surgery. It’s becoming more popular because it can greatly reduce the need for blood from others.
The process includes several steps:
- Aspirating shed blood from the surgical site.
- Processing the collected blood to remove contaminants and debris.
- Reinfusing the processed blood back into the patient.
This technology saves the patient’s blood and lowers the risk of blood transfusions from others. It’s very helpful in surgeries with a lot of blood loss, like heart, bone, and trauma surgeries.
Postoperative Blood Recovery
Postoperative blood recovery collects and reinfuses blood lost after surgery. It’s like intraoperative cell salvage but for blood lost after the operation. It aims to cut down on blood loss and the need for more transfusions later.
The advantages of postoperative blood recovery are:
- Less exposure to blood from others.
- Keeping the patient’s own blood.
- Potential decrease in complications after surgery.
By using these advanced blood recovery and autologous transfusion systems, healthcare providers can make patients safer and improve results. As medicine keeps evolving, we’ll see more of these technologies. They will shape the future of transfusion medicine.
Pharmaceutical Alternatives to Blood Transfusion
Pharmaceutical alternatives are changing healthcare by reducing blood transfusions. They tackle issues like shortages, compatibility problems, and contamination risks. This shift is towards new, innovative solutions.
Intravenous and Oral Iron Supplementation
Iron supplements are key in cutting down blood transfusion needs. Intravenous iron helps those with severe iron deficiency or who can’t take oral iron. Oral iron is good for mild to moderate cases.
Iron supplements have lowered blood transfusion needs in surgeries and chronic disease care. They improve patient results and cut healthcare costs.
Hemostatic Medications to Reduce Blood Loss
Hemostatic drugs, like tranexamic acid (TXA), are known for reducing bleeding. TXA stops fibrin clots from breaking down, helping blood to clot better.
TXA has shown great results in surgeries and trauma. It cuts down on blood loss and transfusion needs, making patients safer and outcomes better.
Other hemostatic agents are being studied for their blood loss reduction and transfusion avoidance. These include topical and systemic agents that help with clotting.
Volume Expanders and Fluid Resuscitation Options
Volume expanders are key in fluid resuscitation. They help restore blood volume in patients who have lost a lot of blood. These solutions are vital for trauma, surgical, dehydration, or shock cases.
Crystalloid Solutions in Emergency Settings
Crystalloid solutions are the first choice in emergencies to replace lost plasma volume. They have electrolytes and solutes in water, making them good for initial volume expansion.
Key characteristics of crystalloid solutions include:
- Easy to administer and widely available
- Inexpensive compared to colloid solutions
- Effective in expanding intravascular volume
Examples of crystalloid solutions are normal saline and Ringer’s lactate. They help treat hypovolemia and keep blood pressure stable in emergencies.
Colloid Solutions: Applications and Limitations
Colloid solutions have larger molecules that stay in the bloodstream longer. They provide sustained blood volume expansion. They are used when crystalloids are not enough or in specific cases.
Advantages and limitations of colloid solutions:
- Advantages: Better at expanding plasma volume, possibly reducing blood transfusion needs.
- Limitations: More expensive than crystalloids, can cause allergic reactions, and may affect blood clotting.
Hospital Integration of Non-Blood Volume Management
Effective non-blood volume management in hospitals needs a team effort. This includes:
- Creating clear fluid resuscitation protocols
- Training healthcare staff on volume expanders
- Watching patient outcomes to adjust treatments
By doing these things, hospitals can better care for patients. They can also use less blood, saving resources and reducing transfusion risks.
Conclusion: The Future of Transfusion Medicine
The future of transfusion medicine is changing fast. New technologies and medicines are making patient care better. They help solve problems like blood shortages and contamination risks.
Many new options are coming up. These include Hemoglobin-Based Oxygen Carriers (HBOCs) and Perfluorocarbon Emulsions. There are also advanced ways to manage platelets and blood recovery systems. Plus, new medicines and volume expanders are being developed.
These new methods will change how we treat patients. They will make treatments safer and more effective. Healthcare providers will be able to give better care and meet the growing need for blood transfusions.
FAQ’s:
What are the main challenges associated with traditional blood transfusions?
Traditional blood transfusions have many challenges. These include shortages, issues with compatibility, and risks of contamination. This shows why we need new ways to help patients instead of just blood transfusions.
How do Hemoglobin-Based Oxygen Carriers (HBOCs) work?
HBOCs carry oxygen in the blood. They work with all blood types and don’t need to be kept cold. This makes them a good option for blood transfusions.
What are perfluorocarbon emulsions used for?
Perfluorocarbon emulsions are synthetic oxygen carriers. They help deliver oxygen to tissues. They could be used as an alternative to blood transfusions in some cases.
How are advanced platelet management technologies improving transfusion medicine?
New technologies for managing platelets are helping a lot. These include using fewer platelets, storing them cold, and freeze-drying them. This increases the supply of platelets and improves transfusions.
What is the role of blood recovery and autologous transfusion systems?
Blood recovery and autologous transfusion systems are key. They use the patient’s own blood, reducing the need for blood from others. This includes technologies used during and after surgery.
How do pharmaceutical alternatives help reduce the need for blood transfusions?
Pharmaceutical alternatives are very helpful. They include iron supplements and medications like tranexamic acid (TXA). These help reduce blood loss and the need for blood transfusions.
What are volume expanders and fluid resuscitation options used for?
Volume expanders and fluid resuscitation options are used in emergencies. They help manage blood volume and support patients. They are alternatives to blood transfusions in urgent situations.
What is the future of transfusion medicine?
The future of transfusion medicine looks bright. New alternatives like HBOCs, perfluorocarbon emulsions, and advanced platelet management are improving care. Blood recovery systems, pharmaceuticals, and volume expanders are also playing a big role. Together, they are making transfusions safer and less needed.
References
- Mokhtar, G., et al. (2024). Transfusion ofbloodcomponents in pediatric age groups. Annals of Hematology, 103(2), 423-435.








