Learn about Alzheimer’s Disease, a progressive condition affecting memory and thinking. Discover what neurologists do, how they examine patients, and the basics of dementia care.
Send us all your questions or requests, and our expert team will assist you.
Overview And Definitions
What is Alzheimer’s Disease
Alzheimer’s Disease is a progressive neurologic disorder that causes the brain to shrink and brain cells to die. It is the most common cause of dementia which is a continuous decline in thinking behavioral and social skills that affects a person’s ability to function independently. The disease begins slowly and worsens over time.
In the early stages memory loss is mild but with late stage disease individuals lose the ability to carry on a conversation and respond to their environment. The condition is not a normal part of aging although increasing age is the greatest known risk factor. It involves the gradual destruction of the hippocampus which is the region of the brain primarily responsible for memory formation.
What is a Neurologist?

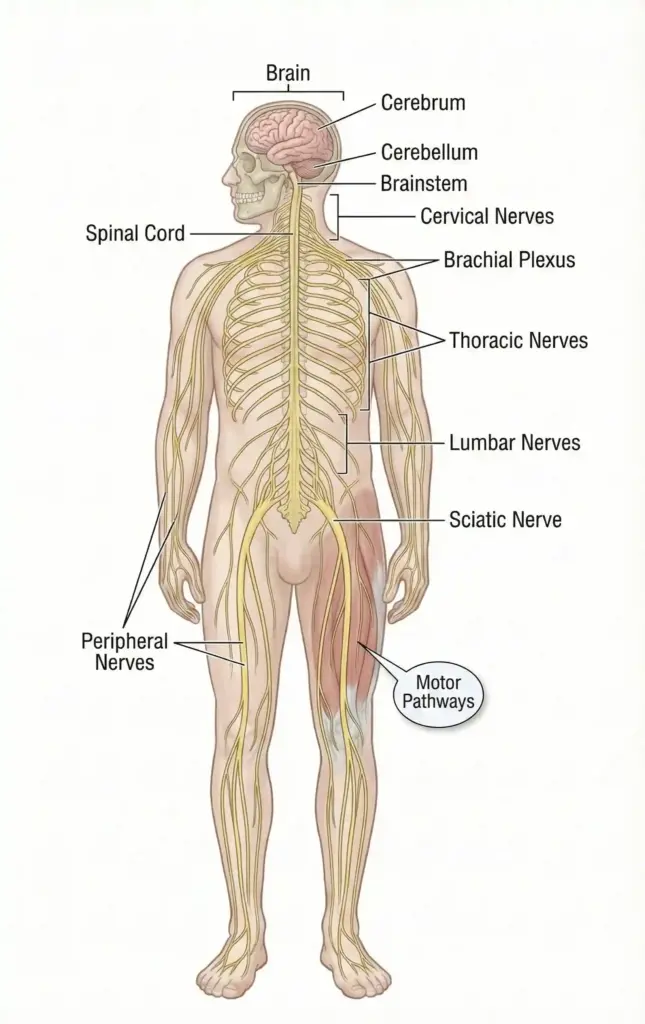
A neurologist is a medical doctor who specializes in diagnosing, treating, and managing disorders of the brain and nervous system. The nervous system is a complex, sophisticated system that regulates and coordinates body activities. It has two major divisions including the central nervous system composed of the brain and spinal cord, and the peripheral nervous system composed of all other neural elements.
Neurologists undergo extensive training including four years of medical school, a one year internship, and at least three years of specialized residency in neurology. For conditions like Alzheimer’s Disease, neurologists are often the primary specialists who confirm the diagnosis. They differ from neurosurgeons as they do not perform surgery. Instead, they rely on clinical examination, cognitive testing, and medical management to help patients.
Their role involves:
What Do They Treat?

Neurologists treat a vast array of conditions that affect the nervous system. While they are central to the management of Alzheimer’s Disease, their expertise covers the entire spectrum of neurological health. They manage conditions that are acute, such as strokes, as well as chronic degenerative conditions.
In the specific context of cognitive disorders, they treat various forms of dementia. They distinguish Alzheimer’s Disease from other types such as vascular dementia, Lewy body dementia, and frontotemporal dementia. This distinction is crucial because the treatment and progression for each type can differ. They also manage the complications associated with these diseases, such as sleep disorders, depression, and seizures.
Common conditions treated include:
Symptoms and Risk Factors
Memory loss is the key symptom of the disease. Early signs include difficulty remembering recent events or conversations. As the disease progresses memory impairments worsen and other symptoms develop. Individuals may repeat statements and questions over and over or forget conversations appointments or events. They often misplace possessions and put them in illogical locations.
Beyond memory patients experience confusion regarding time and place and may get lost in familiar places. Language problems arise causing difficulty finding the right words or following conversations. Behavioral changes are also common including depression apathy social withdrawal mood swings distrust in others irritability and aggressiveness.
Age is the single most significant risk factor for the disease with the likelihood of developing the condition increasing notably after the age of sixty five. Family history and genetics play a major role particularly if a first degree relative has the disorder. Specific genetic mechanisms such as the presence of the apolipoprotein E gene can increase the risk.
Women are slightly more likely to develop the disease than men primarily because they live longer. There is also a strong link between head trauma and future risk of dementia. Lifestyle factors that affect heart health such as lack of exercise obesity smoking high blood pressure and high cholesterol are also associated with a higher risk of developing the disease.

Diagnosis and Imaging
There is no single test that confirms the disease. Diagnosis is a multi step process that aims to rule out other causes for memory loss and cognitive decline. Physicians conduct a thorough medical history and evaluate mental status through specific cognitive tests that assess memory and thinking skills.
They also interview family members or close friends to gain insight into changes in behavior and daily function. Neurological exams are performed to test reflexes muscle tone and sense of sight and hearing. Blood tests are routinely ordered to rule out other potential causes of confusion such as thyroid disorders or vitamin deficiencies.
Brain imaging is crucial in the diagnostic evaluation. Magnetic resonance imaging or computed tomography scans are used primarily to rule out other conditions that may cause similar symptoms such as strokes tumors or head trauma. These scans can also reveal distinct patterns of brain shrinkage that are characteristic of the disease. Positron emission tomography scans can help detect the presence of amyloid plaques or tau tangles in the brain which supports a more accurate diagnosis.
While definite confirmation was historically only possible via autopsy advanced imaging and newer analysis of biomarkers in cerebrospinal fluid are improving the accuracy of clinical diagnoses in living patients.and anxiety. Non pharmaceutical approaches are generally considered the first line of defense such as creating a calm environment to reduce agitation. The financial impact of the disease is profound with global estimates for care often ranging from tens of thousands to over one hundred thousand dollars annually depending on whether professional home nursing or residential care is required.
Rehabilitation strategies focus on maintaining the highest possible level of function and safety. Physical therapy helps improve balance and muscle strength to reduce the risk of falls which is a frequent complication. Occupational therapy involves modifying the home environment to remove hazards and simplifying daily tasks like dressing and bathing.
Cognitive stimulation therapy provides social engagement and mental exercises that may improve quality of life. Nutritional support is also critical as patients often lose the ability to recognize hunger or use utensils properly leading to weight loss and dehydration.

Send us all your questions or requests, and our expert team will assist you.
Treatment and Rehabilitation
Current medical management aims to temporarily improve symptoms or slow the rate of decline as there is no cure that stops the disease process. Physicians prescribe medications that help regulate neurotransmitters in the brain which are chemicals that transmit messages between neurons. These drugs may help maintain thinking memory and communication skills for a period of time.
Management also includes treating behavioral symptoms like sleeplessness wandering and anxiety. Non pharmaceutical approaches are generally considered the first line of defense such as creating a calm environment to reduce agitation. The financial impact of the disease is profound with global estimates for care often ranging from tens of thousands to over one hundred thousand dollars annually depending on whether professional home nursing or residential care is required.
Rehabilitation strategies focus on maintaining the highest possible level of function and safety. Physical therapy helps improve balance and muscle strength to reduce the risk of falls which is a frequent complication. Occupational therapy involves modifying the home environment to remove hazards and simplifying daily tasks like dressing and bathing.
Cognitive stimulation therapy provides social engagement and mental exercises that may improve quality of life. Nutritional support is also critical as patients often lose the ability to recognize hunger or use utensils properly leading to weight loss and dehydration.
Long-Term Care
As the disease progresses to severe stages patients lose the ability to respond to their environment and control movement. They become entirely dependent on caregivers for all activities of daily living including eating toileting and bathing. Incontinence and immobility are common issues that require constant management to prevent complications like pressure ulcers.
Safety becomes a primary concern as wandering and swallowing difficulties increase. The physical and emotional burden on family caregivers is significant often necessitating the transition to a specialized memory care unit or full time professional home assistance.
The final phase of the disease focuses exclusively on comfort and dignity rather than extending life. Palliative care teams work to manage symptoms such as pain anxiety and rigidity. Advance care planning is essential to address decisions regarding artificial nutrition and hydration as swallowing mechanisms fail.
Hospice care is frequently utilized to provide comprehensive support to both the patient and their family. The goal is to ensure a peaceful end of life experience while offering counseling and resources to loved ones to help them cope with grief and loss.

Alzheimer’s Disease is a progressive brain disorder causing dementia and is defined by plaques and tangles. A specialist (neurologist/geriatrician) diagnoses the disease, manages medications to slow symptoms, and coordinates supportive care.
Alzheimer’s disease does not treat conditions; rather, it is the condition. Specialists treat the associated symptoms, which include memory loss, cognitive decline, confusion, and challenging behavioral changes (like aggression or wandering).
The main classification is by onset age: Late-Onset (mid-60s and older) is the most common form, while Early-Onset (30s to 60s) is rare and often linked to specific genetic factors.
You should see a specialist if memory loss or cognitive issues consistently interfere with daily life, such as repeatedly getting lost, struggling to manage money, or asking the same question repeatedly without retaining the answer.
Most common forms (like diabetic) are acquired. Some rare forms of neuropathy are genetic. A family history of diabetes is an indirect risk factor, as it raises the likelihood of developing the primary disease.

Can Stress Cause Epilepsy? Understanding the Connection Between Stress and Seizures <image1> Did you know that stress can trigger seizures in some individuals? Research shows
A recent study in the Radiation Oncology journal found that 13% of patients died within 30 days after getting palliative radiotherapy for bone metastases. Another

Choosing to have a carotid endarterectomy is a big decision. It’s important to know what to expect during recovery. Did you know that almost 100,000

Finding a lump inside your cheek can be scary. But knowing what it might be and when to see a doctor can help. At Liv
When serious bone damage happens, like from fractures or disease, our body might not heal on its own. That’s when a bone graft operation is

Cadaver bone grafts have changed orthopedic surgery a lot. They help patients who need bone replacement because of injuries, diseases, or surgery problems. Johns Hopkins

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)