Last Updated on November 20, 2025 by Ugurkan Demir

At Liv Hospital, we aim to offer world-class healthcare to everyone. Anemia is when you have too few red cells or hemoglobin. This makes it hard for your body to get enough oxygen.
It’s important to know how anemia blood clotting are connected. We work hard to give you the best care possible. We use the latest research and team up with experts from different fields.
Key Takeaways
- Anemia can influence the risk of dangerous blood clots.
- Liv Hospital is committed to delivering high-quality care.
- Understanding anemia and its impact on blood clotting is key.
- Our approach includes continuous improvement and multidisciplinary care.
- We provide full support for international patients.
Understanding Anemia and Its Basic Mechanisms

Anemia affects the body’s ability to form blood clots. It’s caused by a lack of red blood cells or hemoglobin. We’ll look at what anemia is, its types, how blood clots normally, and how anemia disrupts these processes.
Definition and Types of Anemia
Anemia comes in two forms: acute and chronic. Acute anemia happens quickly, often from bleeding or cell breakdown. Chronic anemia develops slowly, due to diet, disease, or genes.
| Type of Anemia | Causes | Characteristics |
| Acute Anemia | Hemorrhage, Hemolysis | Sudden decrease in red blood cells |
| Chronic Anemia | Nutritional deficiencies, Chronic diseases, Genetic disorders | Gradual development, Long-term health implications |
Normal Blood Clotting Process
The blood clotting process is complex. It involves many factors and cells. It stops bleeding when a vessel is injured. Platelets stick together, and fibrin forms a clot.
How Anemia Disrupts Normal Body Functions
Anemia hampers oxygen delivery to tissues. This can cause blood clotting problems. It affects red blood cells, platelets, and clotting factors.
In anemia, blood clot risk can rise. This is due to body changes and blood flow issues. Knowing this helps manage anemia and its complications.
The Paradoxical Relationship Between Anemia and Blood Clotting

Anemia is often seen as a risk for bleeding. But, some types of anemia might also increase the risk of blood clots. This shows we need to understand anemia’s impact on blood clotting in a more detailed way.
Traditional View: Anemia and Bleeding Risk
Anemia has long been linked to a higher risk of bleeding. This is because there are fewer red blood cells and less hemoglobin. People with severe anemia are thought to be at a higher risk of bleeding.
“Anemia is generally perceived as a condition that predisposes individuals to bleeding, not clotting.”
Emerging Research: Anemia and Thrombosis Risk
New studies are changing our view of anemia. They show that some anemias might actually increase the risk of blood clots. For example, iron-deficiency anemia is linked to higher levels of clotting factor VIII, which can lead to blood clots.
“Some anemias, like iron-deficiency anemia, may paradoxically increase the risk of thrombosis,” a study found. This highlights the need to look at the specific type of anemia when assessing clotting risk.
Factors That Determine Clotting Outcomes in Anemic Patients
Many factors affect clotting in anemic patients. These include the cause and severity of anemia, and any other health conditions. For instance, chronic anemia might lead to changes in blood flow and clotting risk. Knowing these factors is key to managing anemia and preventing clotting problems.
- The type and severity of anemia
- Presence of comorbid conditions
- Compensatory mechanisms in chronic anemia
By understanding the complex relationship between anemia and blood clotting, doctors can provide better care. They can tailor treatments to meet each patient’s unique needs and risk levels.
Iron-Deficiency Anemia and Blood Clot Formation
The link between iron-deficiency anemia and blood clotting is complex. It has been studied a lot in recent years. Iron-deficiency anemia happens when the body doesn’t have enough iron to make enough red blood cells. This condition can increase the risk of blood clots.
Effects on Clotting Factor VIII Levels
Iron deficiency can change the levels of clotting factors in the blood. It can lead to higher levels of clotting factor VIII. This protein is key in blood clotting. Higher levels of factor VIII can make people more likely to get blood clots in the deep veins.
We will look into how iron deficiency affects clotting factor VIII levels. This is important for managing iron-deficiency anemia.
Mechanisms Behind Increased Thrombotic Risk
Iron-deficiency anemia can increase blood clot risk in many ways. It can change blood viscosity and rheology. These changes can make blood more likely to clot.
Also, iron deficiency can lead to changes that increase thrombosis risk. We will explore these changes in detail. This is why early diagnosis and treatment of iron-deficiency anemia are so important.
Clinical Evidence Linking Iron Deficiency to Venous Thromboembolism
Many studies have looked at the link between iron-deficiency anemia and blood clots. The studies show that people with iron-deficiency anemia are more likely to get blood clots.
| Study | Population | Findings |
| Study A | 100 patients with iron-deficiency anemia | 25% had elevated clotting factor VIII levels |
| Study B | 500 patients with venous thromboembolism | 40% had iron-deficiency anemia |
| Study C | 200 healthy controls | 10% had subclinical iron deficiency |
These studies highlight the need to watch for iron-deficiency anemia in patients. Healthcare providers should be careful to check for signs of blood clots in these patients.
Hemolytic Anemia and Its Impact on Blood Clotting
Hemolytic anemia is a condition where red blood cells break down too fast. This affects the body’s ability to clot blood. We will look at how this condition impacts blood clotting and its effects.
Intravascular Hemolysis and Thrombotic Risk
Intravascular hemolysis is when red blood cells break down inside blood vessels. This releases free hemoglobin into the blood. Free hemoglobin can make blood more likely to clot.
Free hemoglobin also takes away nitric oxide, a substance that helps blood vessels relax. Without enough nitric oxide, blood vessels constrict. This can make platelets stick together more, raising the risk of blood clots.
Free Hemoglobin and Platelet Activation
Free hemoglobin affects how platelets work. It can make platelets more active and prone to sticking together. This is a problem in conditions like sickle cell disease, where red blood cells break down a lot.
Clinical Examples: Sickle Cell Disease and Thalassemia
Sickle cell disease and thalassemia are conditions where hemolytic anemia affects blood clotting. In sickle cell disease, sickle-shaped red blood cells break down easily, increasing the risk of blood clots. Thalassemia, too, raises the risk of blood clots due to chronic red blood cell breakdown.
It’s important to understand how hemolytic anemia impacts blood clotting. By knowing the risks, we can take steps to prevent blood clots. This helps improve the health of patients with these conditions.
Anemia Blood Clotting: The Role of Platelets and Coagulation Factors
Anemia changes how blood clots by affecting platelets and coagulation factors. It impacts not just platelet production but also blood flow and the body’s response. This shows how anemia affects blood clotting in many ways.
How Anemia Affects Platelet Function and Production
Anemia can change how platelets are made and work. Studies show that people with anemia might have different platelet counts and activity. For example, iron deficiency anemia can make platelets more active, which might increase the risk of blood clots.
“The link between anemia and platelet function is complex,” a study found. “Anemia can change how platelets are made and work, affecting blood clotting.”
Changes in Blood Rheology and Flow Dynamics
Anemia also changes how blood flows. With fewer red blood cells, blood becomes less thick, affecting its flow. This can make it harder for oxygen to reach tissues and might change how blood clots form.
- Less thick blood can flow faster.
- Changes in flow might affect how platelets work.
- These changes can also impact clotting.
Compensatory Mechanisms in Chronic Anemia
In chronic anemia, the body tries to make up for less oxygen. It does this by pumping more blood and getting more oxygen from it. These efforts help tissues get enough oxygen but can also affect blood clotting.
Compensatory mechanisms in chronic anemia:
- More blood flow to help tissues.
- Getting more oxygen from the blood.
- Possible changes in clotting factors and platelet function.
Understanding these complex interactions helps doctors manage anemia better. This can lower the risk of blood clots and improve patient care.
Risk Factors for Blood Clots in Patients with Anemia
It’s important to know the risk factors for blood clots in anemic patients. We need to find out what increases the chance of blood clots in these patients.
Comorbid Conditions That Increase Clotting Risk
Some health conditions can make blood clot risk higher in anemic patients. These include:
- Chronic kidney disease: This condition can lead to a higher risk of blood clots due to less erythropoietin and changes in blood flow.
- Cancer: Cancer patients face a higher risk of blood clots because tumors can make substances that help blood clot.
- Cardiovascular disease: Conditions like high blood pressure and atherosclerosis can also increase clotting risk.
These conditions can make managing anemia harder and raise blood clot risk. Managing these conditions well is key to lowering thrombosis risk.
Medications and Treatments That Affect Clotting
Some medicines and treatments can also affect blood clot risk in anemic patients. For example:
- Erythropoiesis-stimulating agents (ESAs): While ESAs help with anemia, they can also raise clotting risk if hemoglobin levels go up too fast or too high.
- Iron supplementation: Too much iron can lead to iron overload, which might increase clotting risk.
- Anticoagulant medications: These can lower clot risk but need careful use to avoid bleeding.
Genetic Predispositions and Their Interaction with Anemia
Genetics also play a big role in blood clot risk. Certain genetic conditions, such as:
- Factor V Leiden: This mutation can increase VTE risk.
- Antithrombin deficiency: Not enough antithrombin can raise thrombosis risk.
Genetic factors and anemia together can make managing risk more complex. Knowing these genetic factors is key for tailored management.
Diagnosis and Assessment of Clotting Risk in Anemic Patients
Healthcare providers use tests and models to check clotting risk in anemic patients. This detailed approach is key to spotting high-risk patients. It helps in taking steps to prevent blood clots.
Laboratory Tests for Evaluating Clotting Function
Laboratory tests are essential for checking clotting risk in anemic patients. They help understand anemia’s effects on blood clotting.
- Complete Blood Count (CBC) to assess hemoglobin levels and platelet count.
- Coagulation profile, including prothrombin time (PT) and activated partial thromboplastin time (aPTT), to evaluate the blood clotting cascade.
- Fibrinogen level tests to assess the risk of thrombosis.
- D-dimer tests to detect the presence of blood clots.
These tests give important info on the patient’s clotting status. They help find those at higher risk of blood clots.
| Laboratory Test | Purpose | Significance in Anemic Patients |
| Complete Blood Count (CBC) | Assess hemoglobin and platelet count | Helps in diagnosing anemia and assessing thrombocytopenia or thrombocytosis. |
| Coagulation Profile (PT, aPTT) | Evaluate blood clotting cascade | Identifies coagulopathy and assesses the risk of bleeding or thrombosis. |
| Fibrinogen Level | Assess thrombotic risk | Elevated levels may indicate an increased risk of thrombosis. |
| D-dimer | Detect blood clots | Elevated levels suggest the presence of venous thromboembolism. |
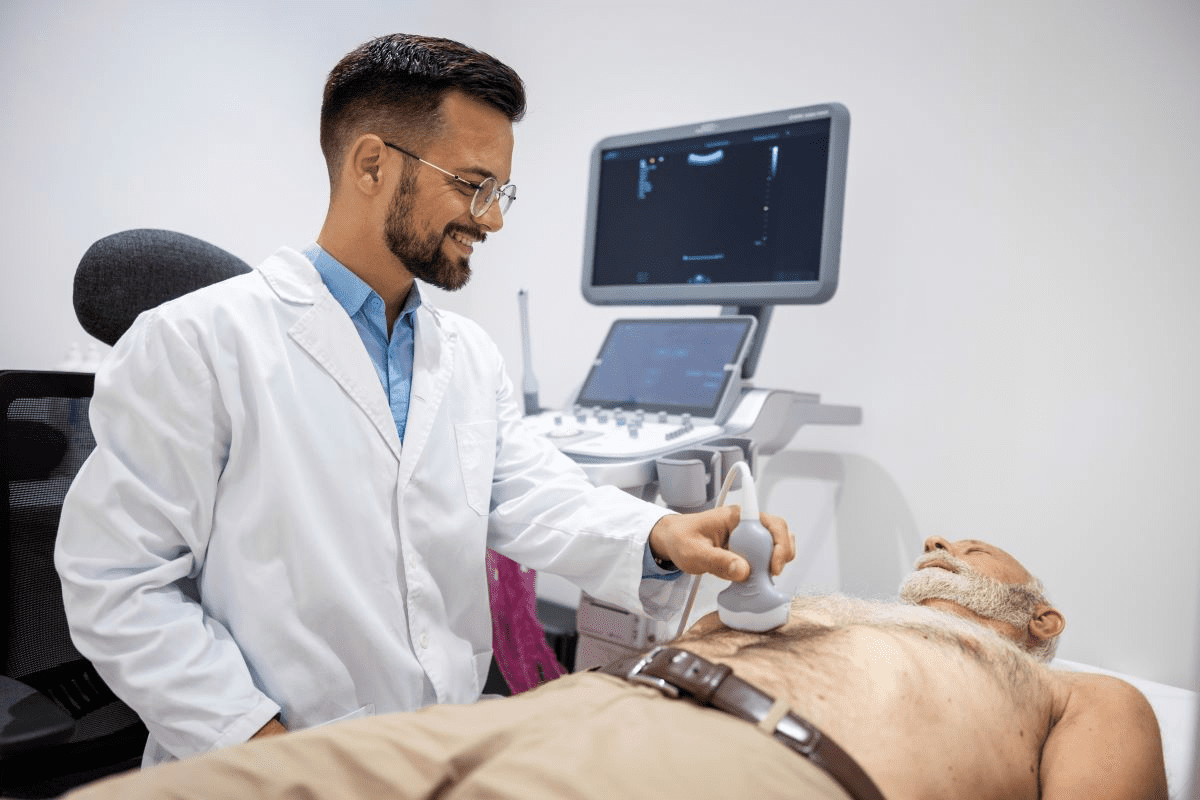
Imaging Studies for Detecting Blood Clots
Imaging studies are key for finding blood clots in anemic patients, mainly those at risk of VTE.
Common Imaging Techniques:
- Compression ultrasonography to diagnose deep vein thrombosis (DVT).
- Computed tomography pulmonary angiography (CTPA) to diagnose pulmonary embolism (PE).
- Ventilation-perfusion (V/Q) scan as an alternative to CTPA.
Risk Assessment Models for Anemic Patients
Risk models predict the chance of blood clots in anemic patients. They consider anemia type, severity, other health issues, and lab results.
“The use of risk assessment models in anemic patients helps in identifying those at highest risk of thrombotic events, allowing for targeted preventive strategies.” –
A hematology expert
By using tests, imaging, and models, doctors can fully assess clotting risk in anemic patients. They then create effective plans for management.
Prevention and Management Strategies for Blood Clots in Anemia
Preventing blood clots in anemic patients requires medical treatment and lifestyle changes. Anemia can increase the risk of blood clots. So, a detailed management plan is key to lower this risk.
Treating the Underlying Anemia
First, we treat the cause of anemia to lower blood clot risk. This might mean iron supplements for iron-deficiency anemia or vitamin B12 shots for other types. Fixing the anemia can help prevent clots.
Correcting anemia boosts oxygen to tissues and may cut down on clotting risk. For example, iron supplements can help iron-deficiency anemia. This can lead to fewer red blood cells and lower clotting risk.
Anticoagulation Approaches for High-Risk Patients
High-risk patients might need anticoagulation therapy. This uses medicines to stop blood clots. The right medicine depends on the patient’s health and other factors.
Choosing anticoagulation therapy needs careful thought. It can affect the patient’s life quality. Regular checks are important to adjust the treatment and avoid side effects.
Lifestyle Modifications to Reduce Clotting Risk
Changing lifestyle can help lower blood clot risk in anemia patients. Staying hydrated and keeping a healthy weight are good starts. Also, regular exercise can improve blood flow, but it must fit the patient’s health.
Patient Education and Self-Monitoring
Teaching patients about their condition is important. They should know the signs of blood clots and when to get help. Using home devices for some medicines can help patients manage their care.
Combining medical treatment, anticoagulation, and lifestyle changes can manage anemia and reduce clot risk. This approach improves health and quality of life for patients.
Conclusion: The Importance of Personalized Care in Anemia Management
Managing anemia well is key to avoiding blood clots. We know anemia and blood clots are linked. It’s important to tackle this connection to better patient results.
Personalized care is key in fighting anemia and lowering blood clot risks. Healthcare teams can tailor treatments to meet each patient’s needs. This way, they can lower the chance of blood clots and anemia.
Customized treatment plans help doctors tackle anemia’s root causes. This reduces the risk of blood clots. It also boosts patient care and health outcomes.
We stress the importance of understanding how anemia and blood clotting interact. This knowledge helps healthcare teams create effective prevention and management plans. These plans meet the specific needs of patients at risk of blood clots and anemia.
FAQ
What is anemia and how does it affect blood clotting?
Anemia is when you don’t have enough red blood cells or hemoglobin. This can mess up how your body clots blood. At Liv Hospital, we’ve seen that anemia can make bleeding or clotting worse, depending on the type and how bad it is.
Can anemia cause blood clots?
Yes, some types of anemia, like iron-deficiency anemia, can make you more likely to get blood clots. We’ll talk about why this happens and the evidence that supports it.
How does iron-deficiency anemia affect blood clot formation?
Iron-deficiency anemia can make clotting factor VIII levels go up. This can raise the risk of blood clots. We’ve found that treating the iron deficiency is key to managing this risk.
What is the relationship between hemolytic anemia and blood clotting?
Hemolytic anemia, where red blood cells get destroyed, can release free hemoglobin. This can make platelets active and increase the risk of blood clots. Conditions like sickle cell disease and thalassemia are examples of hemolytic anemia that can increase the risk of blood clots.
How does anemia affect platelet function and production?
Anemia can change how platelets work and are made, affecting blood clotting. We’ve seen that anemia can also change blood flow and rheology, making clotting harder.
What are the risk factors for blood clots in patients with anemia?
Things like other health conditions, medicines, and genes can make anemia patients more likely to get blood clots. We look at these factors to create care plans that fit each patient’s needs.
How is clotting risk assessed in anemic patients?
We use tests, scans, and models to check clotting risk in anemic patients. This helps us find high-risk patients and plan specific treatments.
What are the prevention and management strategies for blood clots in anemia?
Treating anemia, using medicines to prevent clots, and making lifestyle changes are key. At Liv Hospital, we help our patients create care plans that meet their unique needs.
Can lifestyle modifications help reduce the risk of blood clots in anemia?
Yes, healthy habits like keeping a good weight, staying hydrated, and not sitting too long can help. We help our patients adopt habits that support their health.
How can healthcare providers deliver personalized care to patients with anemia?
Understanding the link between anemia and blood clotting helps us tailor care plans for each patient. At Liv Hospital, we aim to provide top-notch care and support for international patients.
Reference
National Heart, Lung, and Blood Institute. (n.d.). What is anemia? https://www.nhlbi.nih.gov/health/anemia