Anemia is a common problem for people with cancer who are receiving chemotherapy. It affects more than 60% of them. It happens when there are fewer red blood cells or hemoglobin, causing fatigue, shortness of breath, and dizziness. It’s very important to treat anemia during chemotherapy to improve life quality and treatment results.
About 89.5% of people with solid tumors who are getting chemotherapy have some low red blood cell count. It’s key to manage anemia well to lessen its effects on patients’ lives. Treatments include blood transfusions, erythropoietin-stimulating agents, iron supplements, and changing what you eat.
Key Takeaways
- Anemia is a common issue during chemotherapy.
- Symptoms include fatigue, shortness of breath, and dizziness.
- Treatment options are available to manage anemia.
- Blood transfusions and erythropoietin-stimulating agents are common treatments.
- Dietary adjustments, including iron supplements, can help.
Understanding Chemotherapy-Induced Anemia
It’s important to know about anemia in patients getting chemotherapy. Anemia happens when chemotherapy stops the bone marrow from making red blood cells. This leads to low hemoglobin levels. Symptoms can really affect a patient’s life quality.
What causes anemia during cancer treatment
Anemia in cancer treatment comes from chemotherapy. These drugs target fast-growing cells, like those in red blood cells.
“Chemotherapy medications attack rapidly dividing cells, including those that eventually form red blood cells, leading to anemia.”
Verywell Health
This makes the body make fewer red blood cells. This results in anemia because of low hemoglobin levels.
The red blood cell count is key to diagnosing anemia. A low count means the body isn’t making enough red blood cells. This can cause fatigue and weakness. Knowing why anemia happens is the first step to managing it.
How chemotherapy affects red blood cell production
Chemotherapy targets the bone marrow, where red blood cells are made. This stops the bone marrow from making new red blood cells. This leads to a lower red blood cell count and anemia.
Regular RBC blood tests are vital for checking red blood cell counts in chemotherapy patients. These tests help doctors see how bad anemia is and what treatment is best.
Common symptoms and their impact on quality of life
Anemia from chemotherapy can really hurt a patient’s quality of life. Symptoms include fatigue, weakness, and shortness of breath. These symptoms make simple tasks hard, affecting a patient’s well-being.
It’s important to understand how anemia affects life quality. Treatment options like erythropoiesis-stimulating agents (ESAs), iron supplementation, and blood transfusions aim to ease symptoms and improve outcomes.
By managing anemia well, doctors can greatly improve patients’ lives during chemotherapy. Regular checks and tailored treatment plans are essential for the best care.
The Prevalence and Impact of Anemia in Cancer Patients
Anemia is a big problem for cancer patients. It affects their health and how well treatments work. Anemia means not enough red blood cells or hemoglobin, making life harder.

Statistics show that 60% of patients develop anemia
About 60% of cancer patients on chemotherapy get anemia. This shows we need better ways to manage anemia. The American Cancer Society says anemia can hurt treatment results and life quality.
“Anemia is a common side effect of cancer and its treatment,” experts say. “It can really affect a patient’s life.”
The growing market for anemia management ($2.77 billion by 2025)
The market for fighting anemia is getting bigger fast. This is because more people get cancer and need chemotherapy. By 2025, it’s expected to hit $2.77 billion, growing 7.1% each year. This shows that more people see anemia as a big problem in cancer treatment.
Effects on treatment outcomes and patient quality of life
Anemia can change treatment plans and life quality a lot. It might make chemotherapy sessions late or reduce doses. It can also cause tiredness, weakness, and breathlessness, making daily tasks hard.
“The impact of anemia on cancer patients cannot be overstated, as it influences both treatment outcomes and patient well-being.”
Managing anemia well is key to better patient outcomes and life quality. We need to look at all treatment options and choose what’s best for each patient.
5 Primary Treatment Options for Anemia During Chemotherapy
There are several ways to treat anemia in people receiving chemotherapy. These methods help reduce symptoms, improve life quality, and achieve better treatment results. Main strategies include boosting red blood cell production, adding iron supplements, and sometimes giving blood transfusions.
Erythropoiesis-Stimulating Agents (ESAs)
ESAs are key in fighting anemia caused by chemotherapy. They help the bone marrow make more red blood cells, which raises hemoglobin levels. Research shows ESAs can increase hemoglobin by 2.28 g/dl and cut down on blood transfusions by up to 30%.
The American Cancer Society says ESAs are a big step forward in treating anemia linked to cancer treatment.
For chemotherapy patients, we suggest starting with ESAs. They’re great for lowering the need for blood transfusions.
Intravenous Iron Supplementation
Intravenous iron is another important treatment. It’s best for those with iron deficiency anemia. It boosts iron levels, which can improve hemoglobin and reduce anemia symptoms.
Benefits of intravenous iron include:
- Quickly fills up iron stores
- Raises hemoglobin levels
- May reduce the need for ESAs or blood transfusions
Oral Iron Therapy
Oral iron is a traditional way to treat iron deficiency anemia. It can work, but its absorption might not be as good as intravenous iron in some cases.
It’s important to watch patients on oral iron therapy closely to see if it’s working well and adjust treatment if needed.
Blood Transfusions
Blood transfusions quickly raise red blood cell counts and are used for severe anemia. They’re effective but come with risks like immune reactions and complications.
“Blood transfusions are a key part of managing anemia in cancer patients, mainly in emergencies or when other treatments fail.”
Knowing these treatment options helps healthcare providers tailor care for anemia in chemotherapy patients. This approach can improve outcomes and life quality.
Risks and Considerations for Anemia Treatments
Treatments for anemia during chemotherapy are key, but they also have risks. We must weigh the benefits against the possible dangers when treating anemia in cancer patients.
ESA-associated Risks of Thromboembolism
Erythropoiesis-stimulating agents (ESAs) can raise the risk of blood clots in about 5% of cases. This has led to strict rules. Thromboembolism risks are a big worry, so we need to watch patients closely.
Hypertension and Other Cardiovascular Concerns
ESAs might also cause high blood pressure and heart problems. We have to think about these risks when using ESAs, even more so for those with heart issues.
Iron Overload Complications
Iron supplements help with anemia but can cause iron overload. This can lead to serious issues like hemochromatosis. So, managing iron carefully is very important.
Transfusion-related Immune Complications
Blood transfusions, a common anemia treatment, can lead to immune problems. We need to know about these risks and take steps to reduce them.
In summary, anemia treatments are essential, but we must also understand and manage their risks. By knowing these complications, we can offer safer and more effective care.
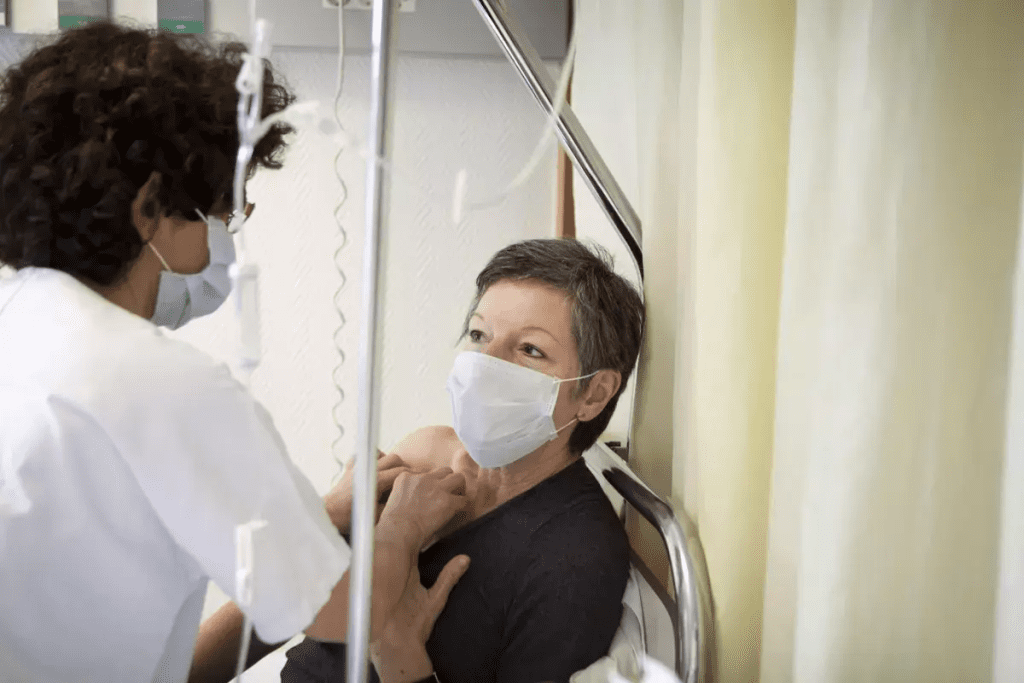
Multidisciplinary Approach to Managing Chemotherapy-Induced Anemia
Managing chemotherapy-induced anemia needs a team effort. At Liv Hospital, we work together with oncologists, hematologists, nutritionists, and more. This teamwork ensures the best care for our patients.
Role of Oncologists, Hematologists, and Nutritionists
A team-based approach is key in fighting anemia during chemo. Oncologists lead the treatment plan. Hematologists focus on blood disorders like anemia. Nutritionists give dietary advice to support health.
- Oncologists watch the cancer treatment and make changes when needed.
- Hematologists diagnose and treat anemia and blood disorders.
- Nutritionists offer diet plans to help with recovery and side effects.
Personalized Treatment Planning Based on Patient Factors
Every patient is different, needing a personalized treatment plan. We look at the patient’s health, cancer type and stage, and chemo regimen. This approach helps manage anemia and improves outcomes.
Regular Monitoring Protocols and Adjustments
Keeping an eye on the patient’s health is vital. We do regular blood tests to check red blood cell count. Based on these results, we adjust the treatment plan for the best care.
- Regular blood tests check red blood cell count.
- The treatment plan changes based on the patient’s response.
- We constantly assess the patient’s health and well-being.
International Best Practices in Anemia Management
At Liv Hospital, we follow international best practices for anemia management. We stay updated with the latest research and guidelines. This ensures our patients get the best care available.
Our multidisciplinary approach and adherence to international standards help us deliver top-notch care. We’re committed to improving our patients’ outcomes in managing chemotherapy-induced anemia.
Conclusion: Optimizing Care for Patients with Chemotherapy-Induced Anemia
Managing anemia during chemotherapy is key to better patient outcomes and quality of life. The American Cancer Society agrees. Anemia is a big problem for those getting chemotherapy, affecting their treatment and well-being.
Healthcare teams can offer better care by working together. They can plan treatments, check on patients, and make changes when needed. Knowing why anemia happens, like how chemotherapy affects red blood cells, helps a lot.
We aim to give top-notch healthcare with full support for patients from around the world. By using the best international practices for treating anemia, we can make patients’ lives better. This improves their quality of life.
FAQ
What is chemotherapy-induced anemia?
Chemotherapy-induced anemia happens when chemo stops the bone marrow from making red blood cells. This leads to low hemoglobin levels. Symptoms include fatigue, weakness, and shortness of breath.
What are the common symptoms of anemia during chemotherapy?
Symptoms of anemia during chemo include fatigue, weakness, shortness of breath, and dizziness. These symptoms can really affect a patient’s quality of life.
How is anemia diagnosed in cancer patients?
Doctors use blood tests to find anemia in cancer patients. These tests check hemoglobin levels, hematocrit, and red blood cell count. This helps doctors know how severe the anemia is and plan treatment.
What are the treatment options for anemia during chemotherapy?
Treatments for anemia during chemo include ESAs, iron supplements, and blood transfusions. The right treatment depends on how bad the anemia is, the patient’s health, and why they have anemia.
What are the risks associated with ESAs?
ESAs can raise the risk of blood clots and high blood pressure. Patients on ESAs need close monitoring to avoid these risks.
How can iron overload be managed during iron supplementation?
Iron overload is managed by checking iron levels, adjusting supplements, and using iron chelators if needed.
What is the role of a multidisciplinary team in managing chemotherapy-induced anemia?
A team of doctors, including oncologists and nutritionists, is key in managing anemia. They create personalized plans, watch patient progress, and adjust treatments as needed.
How can patients undergoing chemotherapy manage anemia?
Patients can manage anemia by working with their healthcare team, following their treatment plan, and making lifestyle changes. This helps reduce symptoms and improve treatment results.
What is the impact of anemia on treatment outcomes for cancer patients?
Anemia can cause delays in chemo, dose cuts, and lower treatment success. This affects treatment results and patient quality of life.
How can healthcare providers optimize care for patients with chemotherapy-induced anemia?
Providers can improve care by following best practices, giving complete care, and using a team approach. This helps manage anemia and its effects on treatment and patient life.
References
U.S. National Library of Medicine. (2022). Chemotherapy-Induced Anemia: Pathophysiology and Management. Journal of the National Comprehensive Cancer Network, 20(4), 398“408. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9010001/





