Last Updated on November 27, 2025 by Bilal Hasdemir

Knowing the difference between angina and heart attack is key for quick medical help. At Liv Hospital, we stress the need to tell these two apart. This helps us give the best care possible.
Angina is when blood flow drops, causing chest pain. It usually happens when you exert yourself and goes away with rest or medicine. On the other hand, a heart attack happens when blood flow stops completely. This causes lasting damage to the heart muscle.
We aim to offer top-notch heart care to our patients from around the world. We follow the latest research and expert advice closely.
Key Takeaways
- Angina is a temporary condition, while a heart attack causes permanent damage.
- Understanding the differences between angina and heart attack is key for quick medical help.
- Liv Hospital provides world-class cardiac care guided by the latest research and expert protocols.
- Distinguishing between angina and heart attack is vital for the right treatment.
- Our team is committed to delivering the highest quality care to international patients.
Understanding Cardiac Chest Pain

It’s key to know the difference between angina and a heart attack. Both are caused by less blood reaching the heart. This is a big deal for your heart health.
The Importance of Recognizing Cardiac Symptoms
Spotting heart symptoms early is vital. Signs like chest pain or shortness of breath mean you might have a serious issue. Acting fast could save your life.
Knowing the signs helps you tell if you’re having angina or a heart attack. Angina is when blood flow drops but doesn’t stop. A heart attack, though, means blood flow is completely blocked.
How Blood Flow Affects Heart Health
Blood flow is super important for your heart. It brings oxygen and nutrients to the heart muscle. If blood flow is cut off, the heart can get damaged.
Keeping blood flow healthy is key to avoiding heart problems. Things like plaque in arteries, high blood pressure, and lifestyle choices can affect blood flow. This is why taking care of your heart is so important.
What is Angina?

Angina is a type of chest pain that happens when the heart doesn’t get enough oxygen. This usually means there’s a problem with the heart’s blood supply.
Definition and Types of Angina
Angina pectoris, or angina, is chest pain or discomfort from not enough oxygen to the heart. There are different types, including:
- Stable Angina: This is predictable chest pain that happens when you’re active or stressed. It goes away with rest or medicine.
- Unstable Angina: This is unpredictable chest pain that can happen at any time. It’s more serious and might mean a heart attack is coming.
- Variant Angina: This happens when you’re resting and is often caused by a spasm in the coronary artery. It can be very severe.
- Microvascular Angina: This is caused by problems with small blood vessels in the heart. It leads to chest pain.
Knowing the type of angina you have is key to getting the right treatment.
Common Triggers for Angina
Things that make the heart need more oxygen or get less can trigger angina. Common ones include:
| Trigger | Description |
|---|---|
| Physical Exertion | Walking, climbing stairs, or exercising can trigger angina. |
| Emotional Stress | Stress, anxiety, or strong feelings can cause angina by making the heart rate and blood pressure go up. |
| Cold Weather | Cold can make blood vessels narrow, reducing blood flow to the heart. |
| Heavy Meals | Eating a big meal can take blood away from the heart, possibly causing angina. |
Knowing what triggers your angina can help you avoid it and make it less severe.
Long-term Prognosis for Angina Patients
The future for people with angina depends on many things. These include the cause, how well treatment works, and lifestyle changes. The American Heart Association says managing angina well can greatly improve life and lower heart attack risk.
“Angina is a warning sign that your heart is not getting enough oxygen-rich blood. By managing your condition and making healthy lifestyle choices, you can reduce your risk of heart attack and improve your overall heart health.”
We stress the importance of working with your doctor to create a plan. This might include medicine, lifestyle changes, and sometimes surgery.
What is a Heart Attack (Myocardial Infarction)?
A heart attack, or myocardial infarction, happens when the heart’s blood supply stops. This is a serious medical emergency that needs quick action. We’ll look at what it is, how it happens, who’s at risk, and how it affects the heart.
Definition and Mechanism of Heart Attacks
A heart attack happens when blood flow to the heart stops for too long. This damages or kills part of the heart muscle. It’s usually because of a blockage in the coronary arteries, often from a blood clot.
Myocardial infarction vs angina is key to understand. Both cause chest pain, but a heart attack is more serious. It damages the heart muscle, unlike angina, which is usually temporary.
Risk Factors for Myocardial Infarction
Many things can increase your risk of a heart attack. These include high blood pressure, high cholesterol, smoking, diabetes, obesity, and a family history of heart disease. Knowing these risks helps prevent and treat heart problems early.
- High blood pressure can damage the coronary arteries, making them more susceptible to blockage.
- Smoking damages the inner lining of blood vessels, making them more prone to blockages.
- Diabetes can damage blood vessels and nerves that control the heart.
Immediate and Long-term Impact on Heart Muscle
A heart attack can severely damage the heart muscle right away. The damage depends on how long the blockage lasts and where it is. Quick medical care is key to reduce damage.
Long-term, a heart attack can lead to heart failure. This is when the heart can’t pump enough blood. Recovery and lifestyle changes are vital to avoid more heart problems.
It’s critical to know the signs of a heart attack and get help fast. Understanding the difference between MI and angina can save lives.
Angina vs Heart Attack: The 4 Key Differences
Angina and heart attacks are two heart conditions that are often mixed up. But they are different. Knowing these differences is key for the right treatment.
Difference #1: Cause and Mechanism
Angina happens when the heart’s blood flow drops, often due to stress or hard work. This is because the heart’s arteries are narrowed. A heart attack, or myocardial infarction, is when a heart part dies because it didn’t get enough blood. This usually happens when a blood clot blocks a coronary artery.
Difference #2: Duration and Pattern of Pain
Angina pain is temporary and predictable. It happens during stress or hard work and goes away with rest. Heart attack pain, on the other hand, is long-lasting and unpredictable. It can last over 15 minutes and doesn’t always stop with rest.
Difference #3: Associated Symptoms
Both can cause chest pain, but the symptoms differ. Angina might also cause shortness of breath, fatigue, or nausea, but these go away with rest. Heart attacks have more severe symptoms like intense chest pain, sweating, lightheadedness, or pain in the arm, neck, or jaw.
Difference #4: Long-term Damage and Outcomes
Angina’s long-term effects on the heart are different from heart attacks. Angina doesn’t cause permanent heart muscle damage if treated right. But, a heart attack leads to permanent damage to the heart muscle. This can cause heart failure or other serious issues.
It’s important to know these differences to get the right medical help. While both need doctor’s attention, a heart attack is a life-threatening emergency that needs quick action.
Recognizing the Symptoms: When to Seek Help
Knowing the signs of angina and heart attacks helps you act fast. We’ll show you the warning signs of a heart attack, the signs of angina, and when to call 911.
Red Flags That Indicate a Heart Attack
A heart attack is a serious emergency. Look out for these symptoms:
- Chest pain or discomfort that feels like pressure, tightness, or pain
- Pain or discomfort in one or both arms, the back, neck, jaw, or stomach
- Shortness of breath or difficulty breathing
- Lightheadedness or dizziness
- Cold sweats or nausea
Spotting these symptoms early can save lives.
Symptoms That Suggest Angina
Angina symptoms are similar to heart attacks but follow a different pattern. Common signs include:
- Chest pain or discomfort triggered by exertion or emotional stress
- Pain that is relieved by rest or medication
- Shortness of breath
- Fatigue or weakness
Knowing these symptoms helps manage angina better.
When to Call 911 Immediately
If you or someone else has heart attack symptoms like severe chest pain or trouble breathing, call 911 right away. Quick medical help is key to treating heart attacks and reducing damage.
To understand the difference between angina and heart attack symptoms, let’s compare:
| Symptom | Angina | Heart Attack |
|---|---|---|
| Chest Pain | Triggered by exertion, relieved by rest | Occurs at rest, more severe and prolonged |
| Shortness of Breath | May occur with exertion | Can occur at rest |
| Duration of Pain | Typically short, 5-10 minutes | Prolonged, often more than 15 minutes |
Understanding these differences helps you make better health choices and seek help when needed.
Real-Life Scenarios: Identifying Your Chest Pain
Figuring out if you’re having an angina attack or a heart attack often starts with knowing the details of your chest pain. Real-life examples can help us understand how to spot and talk about symptoms.
Case Study: Exertion-Related Chest Pain
A 55-year-old man felt chest pain when he walked uphill. The pain felt like a squeeze in his chest and went away when he rested. This is common in angina pectoris, where pain happens when the body needs more oxygen during hard work.
Knowing what causes exertion-related chest pain helps in diagnosing angina. It’s important to remember how long and how bad the pain was, and what makes it better.
Case Study: Sudden Severe Chest Pain
A 60-year-old woman suddenly felt very bad chest pain, like a tear, along with trouble breathing and nausea. This is more like a heart attack (myocardial infarction), where pain is very strong and not just from hard work.
It’s key to know how bad and sudden chest pain is, and any other symptoms you have. Quick action is needed to protect the heart muscle.
How to Communicate Your Symptoms Effectively
Telling your doctor about your symptoms clearly is key for the right diagnosis and treatment. Here are some tips:
- Be clear and concise about the nature, duration, and intensity of your chest pain.
- Mention any triggers or factors that relieve the pain.
- List any associated symptoms such as shortness of breath, nausea, or dizziness.
| Symptom | Angina | Heart Attack |
|---|---|---|
| Trigger | Often triggered by exertion or stress | Can occur at any time, not necessarily related to exertion |
| Pain Description | Squeezing or pressure | Severe, often described as tearing or crushing |
| Duration | Typically resolves with rest or medication | Persists and may radiate to other areas |
| Associated Symptoms | May have mild shortness of breath | Often accompanied by shortness of breath, nausea, or dizziness |
By understanding these differences and talking clearly, you can help your doctor make the right call and get the right treatment.
Diagnosis and Medical Response
Diagnosing angina and heart attacks needs a detailed approach. This includes looking at medical history, doing a physical exam, and running tests. We’ll walk you through how these steps help figure out these heart issues.
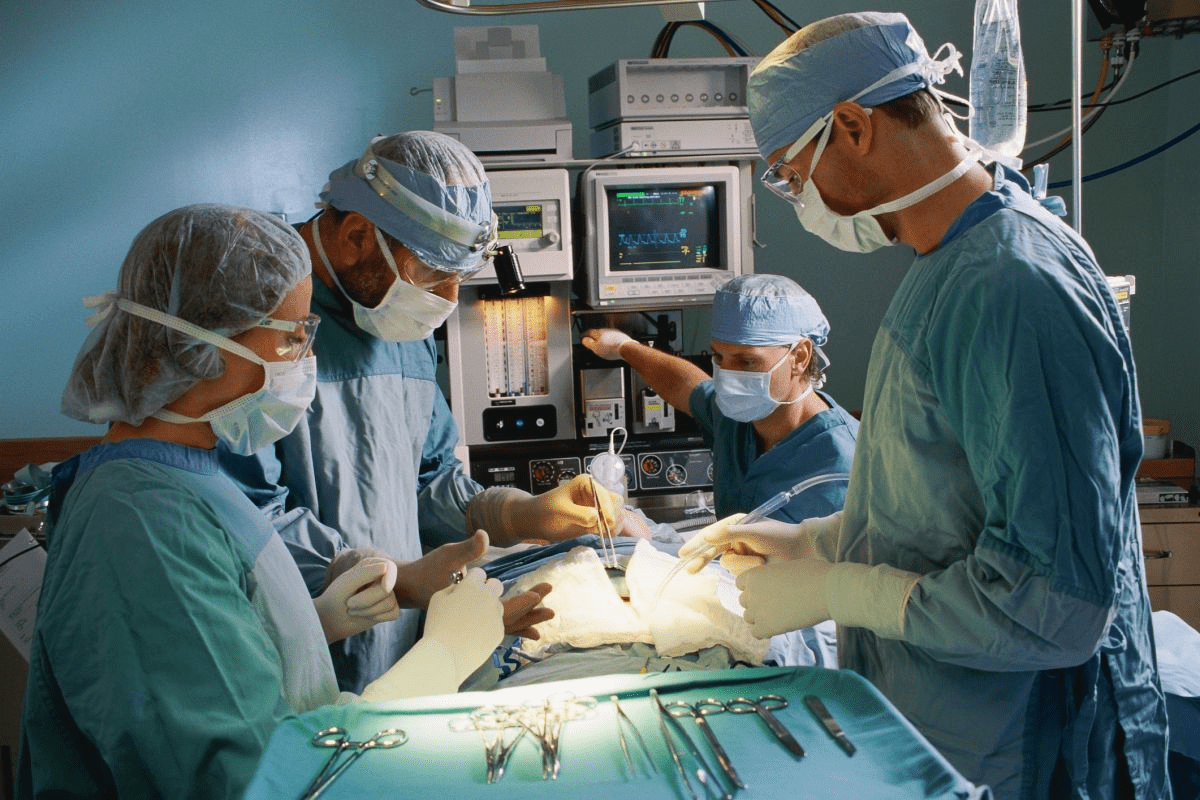
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check-up. We look at symptoms, risk factors, and past heart problems. This helps us guess if it’s angina or a heart attack.
A physical exam might show signs of heart trouble. For example, abnormal heart sounds or signs of heart failure. These signs lead us to more tests.
Diagnostic Tests and Procedures
There are key tests to tell angina from a heart attack. These include:
- Electrocardiogram (ECG or EKG) to check heart rhythm and find ischemia or infarction.
- Stress test to see how the heart works when exerted.
- Echocardiogram to look at heart structure and function.
- Coronary angiography to see the coronary arteries and find blockages.
The Role of Cardiac Biomarkers
Cardiac biomarkers, like troponin levels, are very important in diagnosing heart attacks. High troponin levels mean heart muscle damage, a sign of a heart attack.
Angina usually doesn’t raise cardiac biomarkers. This is because it doesn’t cause much heart muscle damage.
Evidence-Based Approaches to Cardiac Care
We use the latest evidence and guidelines to diagnose and manage heart conditions. This ensures our patients get the best care possible.
| Diagnostic Tool | Angina | Myocardial Infarction |
|---|---|---|
| Electrocardiogram (ECG) | May show ischemia during episodes | Often shows signs of infarction |
| Cardiac Biomarkers | Typically normal | Elevated troponin levels |
| Stress Test | May induce angina symptoms | Not typically performed during acute MI |
Treatment and Recovery
Managing angina and treating heart attacks needs a mix of medicine, lifestyle changes, and rehab. Every patient’s path is different. Our aim is to give care that meets their unique needs.
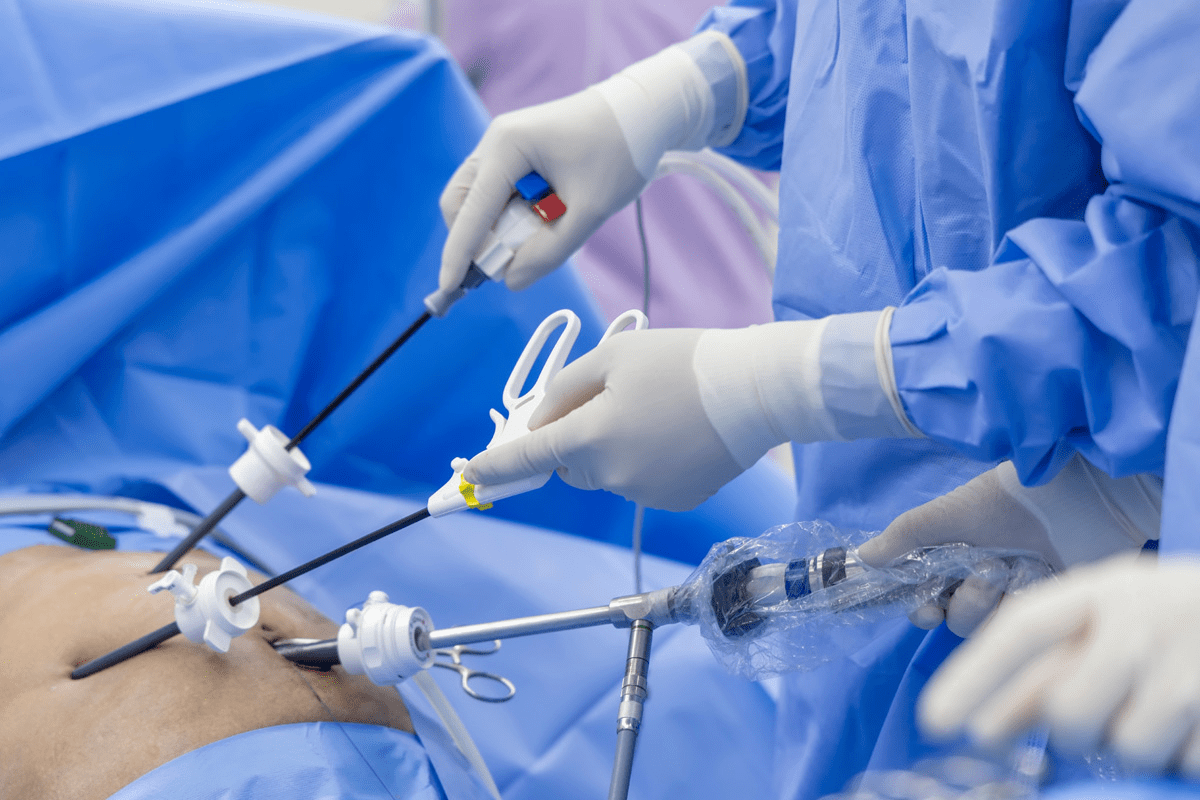
Immediate Interventions for Heart Attacks
When a heart attack happens, quick medical help is key. We focus on fast treatment to protect the heart muscle. The main goal is to get blood flowing back to the heart as fast as we can.
- Administering clot-busting medications to dissolve the blockage
- Performing percutaneous coronary intervention (PCI) to open the blocked artery
- Providing coronary artery bypass grafting (CABG) in some cases
These steps are vital to lower the risk of serious problems and boost survival chances.
Managing Angina Effectively
For those with angina, managing it well means lifestyle changes, medicines, and sometimes surgery. Our goal is to lessen symptoms, enhance life quality, and stop it from turning into a heart attack.
Key strategies include:
- Medicines like nitrates, beta-blockers, and calcium channel blockers to control symptoms
- Lifestyle changes, such as diet, exercise, and quitting smoking
- Keeping an eye on and managing conditions like high blood pressure and diabetes
“Lifestyle changes are key in managing angina. By living healthier, patients can greatly reduce symptoms and boost heart health.”
Rehabilitation After a Cardiac Event
Cardiac rehab is a big part of getting better after a heart attack or other heart issues. Our programs help patients get stronger, improve heart health, and lower the chance of future heart problems.
Rehab includes:
- Supervised exercise to boost heart fitness
- Learning about heart-healthy living
- Support and counseling for stress and emotional challenges
Long-term Medication Strategies
Managing angina and after a heart attack often means taking medicine long-term. We work with patients to create a medicine plan that fits their needs. We make sure they know why sticking to the plan is important and the possible side effects.
Common long-term medicines include:
- Aspirin and other antiplatelet drugs to stop clots
- Beta-blockers to ease the heart’s work
- ACE inhibitors or ARBs to control blood pressure and heart strain
By sticking to a detailed treatment plan and making lifestyle changes, patients can greatly improve their health and life quality.
Conclusion: Protecting Your Heart Health
It’s important to know the difference between angina and a heart attack to keep your heart healthy. Recognizing symptoms early and getting medical help quickly can lower your risk of heart disease.
Keeping your heart healthy means making lifestyle changes and managing risk factors. At Liv Hospital, we offer top-notch cardiac care to patients from around the world. We make sure you get the best support and treatment.
Learning about angina and heart attacks and taking steps to care for your heart can improve your health. We urge everyone to focus on their heart health. Always seek advice from a qualified healthcare professional.
FAQ
What is the main difference between angina and a heart attack?
Angina is chest pain or discomfort from reduced blood flow to the heart. A heart attack is when blood flow is blocked, damaging the heart muscle.
How can I tell if I am experiencing angina or a heart attack?
Angina pain is triggered by exertion or stress and goes away with rest or meds. A heart attack pain is more severe and lasts longer, often with shortness of breath or nausea.
What are the common triggers for angina?
Angina can be triggered by physical exertion, emotional stress, cold weather, heavy meals, or smoking.
What are the risk factors for myocardial infarction?
Risk factors include high blood pressure, high cholesterol, diabetes, smoking, family heart disease history, and obesity.
How is angina diagnosed?
Doctors use medical history, physical exam, ECG, stress test, and coronary angiography to diagnose angina.
What is the role of cardiac biomarkers in diagnosing cardiac conditions?
Cardiac biomarkers like troponin show heart muscle damage. High levels can mean a heart attack or other heart issues.
How is a heart attack treated?
Heart attack treatment includes immediate medical care, clot-busting meds, angioplasty, or bypass grafting.
What is the long-term prognosis for angina patients?
With proper care, many with angina can live active lives. But, it’s key to manage it to avoid heart attacks.
Can angina be a sign of an underlying heart condition?
Yes, angina can signal heart disease like coronary artery disease. Seek medical help if you have symptoms.
How can I manage angina effectively?
Manage angina by quitting smoking, exercising, eating healthy, and following your doctor’s medication advice.
What is the difference between angina pectoris and myocardial infarction?
Angina is chest pain from reduced blood flow. A heart attack is damage from a coronary artery blockage.
Can I have a heart attack without experiencing chest pain?
Yes, some, like women or older adults, may have heart attacks without chest pain. Look for shortness of breath or nausea instead.
How can I differentiate between angina and a heart attack?
It’s hard to tell, but heart attacks have more severe symptoms and often include shortness of breath or nausea.
References
Healthline. Angina vs. Heart Attack: How to Tell the Difference and Next Steps. https://www.healthline.com/health/heart/angina-vs-heart-attack
Drugs.com. Heart Attack – What You Need to Know. https://www.drugs.com/cg/heart-attack.html
American Heart Association (AHA). Angina (Chest Pain). https://www.heart.org/en/health-topics/heart-attack/angina-chest-pain