
At Liv Hospital, we know how vital it is to manage heart rhythms well. Arrhythmias, or irregular heartbeats, can be treated with different medicines. It’s key to know the treatment options to manage heart rhythm disorders well.
Discover antiarrhythmic drugs list used for fast heart rate and palpitations.
Antiarrhythmic medicines are grouped into four main classes. These are based on the Vaughan-Williams classification system. We’ll look at the 15 key medicines for treating fast heart rates and palpitations.
Managing heart rhythm disorders well needs a full approach. We’ll give an overview of the different classes of medicines and their uses. This will help guide you through the treatment options for arrhythmias.
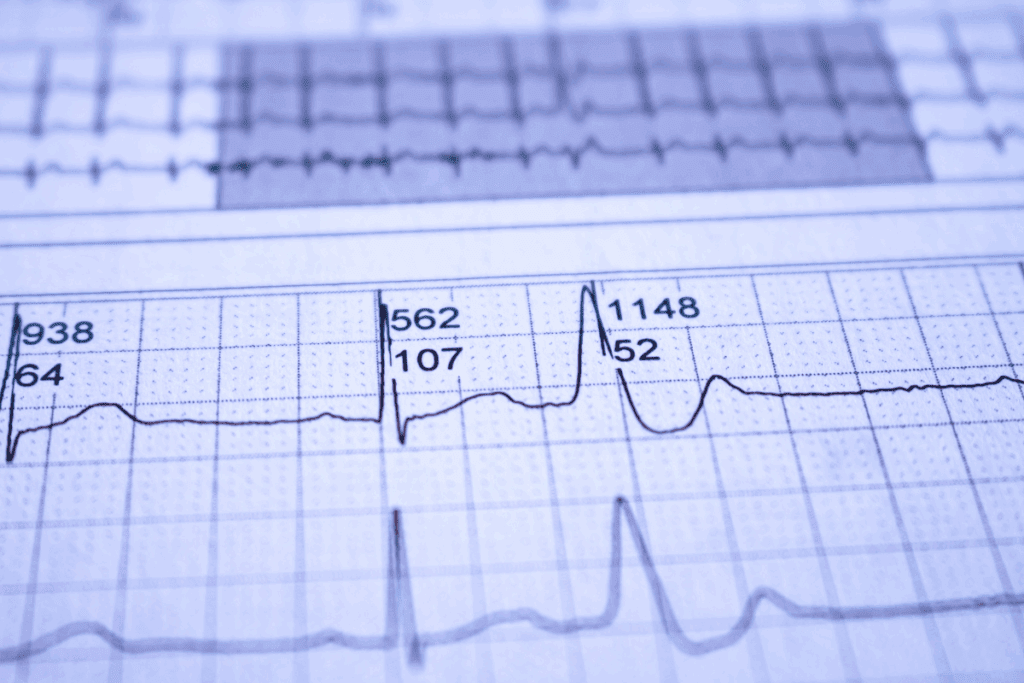
Cardiac arrhythmias happen when the heart’s electrical signals get mixed up. This can cause irregular heartbeats, known as arrhythmias. These can feel like a fast heart rate, palpitations, or irregular rhythms. Knowing about these conditions is key to managing and treating them well.
Cardiac arrhythmias are when the heart beats too slow, too fast, or not right. They can be caused by many things, like electrical problems in the heart. Some arrhythmias are harmless, but others can lead to serious issues like stroke or heart failure. Getting a diagnosis early and treating it right is very important.
There are many types of arrhythmias, like atrial fibrillation and ventricular tachycardia. Each one is different and needs its own treatment. Finding the right treatment starts with knowing exactly what you have.
Antiarrhythmic medications are key in treating cardiac arrhythmias. They help make the heart beat normally again, reduce symptoms, and prevent serious problems. There are many types of these medications, each working in its own way. The right medicine depends on the arrhythmia, how bad it is, and the patient’s health.
These medications can help control the heart rate, fix an abnormal rhythm, or stop arrhythmias from coming back. But, they can also have side effects and interact with other drugs. It’s important to watch how they work and adjust the treatment as needed to get the best results and avoid risks.
The Vaughan-Williams classification helps sort antiarrhythmic drugs by how they work. It’s key in cardiology, making it easier for doctors to pick the right meds for heart rhythm problems.
Antiarrhythmic drugs fall into four main groups based on the Vaughan-Williams system:
The Vaughan-Williams system is vital for picking the right antiarrhythmic treatment. It lets doctors choose the best drug for a specific heart rhythm issue based on how it works.
For example, Class III antiarrhythmics are often used for atrial fibrillation. Class II beta-blockers are used for controlling heart rate in atrial fibrillation and flutter. This system helps tailor treatments to each patient, leading to better results.
Using the Vaughan-Williams classification has several benefits:
Managing heart rhythm problems needs a deep understanding of antiarrhythmic drugs. These medicines are key in treating irregular heartbeats and helping patients get better.
Antiarrhythmic drugs fall into four main groups based on how they work. The Vaughan-Williams system helps doctors choose the right treatment. We’ll look at 15 important antiarrhythmic drugs, their types, and what arrhythmias they treat.
These drugs belong to all four classes: Class I (sodium channel blockers), Class II (beta-blockers), Class III (potassium channel blockers), and Class IV (calcium channel blockers). Each class has its own special uses.
Each antiarrhythmic drug is best for certain arrhythmias. For example, Class IA antiarrhythmics like quinidine and procainamide are good for ventricular arrhythmias. On the other hand, Class III antiarrhythmics like amiodarone and sotalol work well for both ventricular and supraventricular arrhythmias.
Here’s a list of 15 key antiarrhythmic drugs, sorted by class and use:
It’s important to know how each medication works and what it’s for. This way, doctors can pick the best drug for each arrhythmia. This approach helps patients get better and reduces side effects.
Sodium channel blockers, known as Class I antiarrhythmic drugs, are key in treating arrhythmias. They work by blocking sodium channels in the heart. This affects the cardiac action potentials.
Class IA drugs, like quinidine and procainamide, block sodium channels moderately. They also make the action potentials last longer. Quinidine is used for both atrial and ventricular arrhythmias, but its use has decreased due to side effects.
Class IB drugs, including lidocaine and mexiletine, have a small effect on action potentials. They are mainly used for ventricular arrhythmias. Lidocaine is great for sudden cases, like during surgery or heart attacks.
Class IC drugs, such as flecainide and propafenone, block sodium channels a lot but don’t affect action potentials much. They are used for different arrhythmias, like atrial fibrillation and ventricular tachycardia.
| Subclass | Drug Examples | Primary Use | Notable Side Effects |
| IA | Quinidine, Procainamide | Atrial and ventricular arrhythmias | Gastrointestinal issues, cinchonism (quinidine) |
| IB | Lidocaine, Mexiletine | Ventricular arrhythmias | Central nervous system effects, dizziness |
| IC | Flecainide, Propafenone | Atrial fibrillation, ventricular tachycardia | Proarrhythmic effects, negative inotropic effects |
As noted by a cardiology expert, “The choice of antiarrhythmic drug depends on the type of arrhythmia, patient comorbidities, and possible side effects.”
In conclusion, Class I antiarrhythmic drugs are essential in managing cardiac arrhythmias. Knowing about their subclasses and specific drugs is key for effective treatment.
Beta-blockers are key in treating heart rhythm problems. They help control heart rate and reduce symptoms. These drugs block epinephrine’s effects, slowing the heart and easing its workload.
Metoprolol is a top choice for heart rhythm issues. It’s great for controlling heart rate in atrial fibrillation or other fast heart rhythms. It’s perfect for those with palpitations or tachycardia.
Propranolol is also effective against various arrhythmias. It’s good for performance-induced tachycardia or anxiety-related palpitations. Its non-selective nature blocks both beta-1 and beta-2 receptors, providing a wide range of effects.
Atenolol and carvedilol are used for arrhythmia management too. Atenolol is beta-1 selective, making it safe for certain conditions. Carvedilol has alpha-blocking properties, helping in heart failure. Both are chosen based on the patient’s needs and medical history.
| Beta-Blocker | Primary Use | Notable Characteristics |
| Metoprolol | Rate control in atrial fibrillation | Beta-1 selective, effective for tachycardia |
| Propranolol | Arrhythmia management, performance-induced tachycardia | Non-selective, blocks beta-1 and beta-2 receptors |
| Atenolol | Arrhythmia management | Beta-1 selective, suitable for patients with certain comorbidities |
| Carvedilol | Arrhythmia management, heart failure | Non-selective with alpha-blocking properties |
Beta-blockers are versatile in managing arrhythmias. Knowing their specific uses helps healthcare providers tailor treatments. This improves patient outcomes and quality of life.
Class III antiarrhythmic drugs are key in managing irregular heartbeats. They work by extending the action of the heart’s electrical impulses. This is done by blocking potassium channels. This action helps keep the heart rhythm steady and prevents arrhythmias.
Amiodarone is a top choice for treating irregular heart rhythms. It’s used for conditions like atrial fibrillation and ventricular tachycardia. Its complex action affects multiple ion channels, not just potassium.
Sotalol stands out because it blocks both beta receptors and potassium channels. This dual effect makes it effective against many arrhythmias. It’s used for both atrial and ventricular arrhythmias.
Dofetilide is a potassium channel blocker used to keep the heart in rhythm. It’s mainly for patients with atrial fibrillation or flutter. Dronedarone, a derivative of amiodarone, has similar effects but is safer. Yet, it’s not for everyone.
| Drug Name | Primary Use | Notable Characteristics |
| Amiodarone | Various arrhythmias | Complex pharmacology, multiple ion channel effects |
| Sotalol | Atrial and ventricular arrhythmias | Dual action: beta-blocking and potassium channel blockade |
| Dofetilide | Maintaining sinus rhythm in atrial fibrillation/flutter | Selective potassium channel blocker |
| Dronedarone | Atrial fibrillation/flutter | Amiodarone derivative, potentially better safety profile |
Calcium channel blockers are key in treating arrhythmias. They block calcium ions from entering heart cells. This action slows the heart rate and relieves arrhythmia symptoms.
These blockers are great for supraventricular tachycardias and other arrhythmias. We’ll look at verapamil and diltiazem, two common blockers used in treatment.
Verapamil is a strong calcium blocker for SVTs. It slows the AV node’s signal, stopping the arrhythmia or controlling the heart rate.
Key benefits of verapamil include:
Diltiazem is another calcium blocker for arrhythmias. It’s great for controlling heart rate in atrial fibrillation or flutter.
Diltiazem is safe and can be used in patients with certain health issues. Its ability to control heart rate makes it a good choice for managing arrhythmias.
Verapamil and diltiazem both work well for arrhythmias. But, they have different safety profiles and side effects.
| Medication | Efficacy | Common Side Effects |
| Verapamil | Highly effective for SVTs | Constipation, hypotension |
| Diltiazem | Effective for rate control in atrial fibrillation/flutter | Peripheral edema, headache |
Knowing the differences helps doctors choose the best treatment for arrhythmias.
Managing heart palpitations well means knowing their causes and treatment options. These irregular heartbeats can come from arrhythmias, stress, or certain drugs. It’s key to know the cause to pick the right treatment.
It’s important to tell apart palpitations from arrhythmias. Palpitations are the feeling of an irregular or strong heartbeat. Arrhythmias are actual rhythm problems in the heart. Not all palpitations are rhythm issues; some can be from stress, anxiety, or other reasons.
For many, the first step in treating heart palpitations is making lifestyle changes. This includes reducing stress, avoiding caffeine, and drinking enough water. Sometimes, over-the-counter drugs are suggested for relief.
If lifestyle changes don’t work, doctors might prescribe medication. The right drug depends on the cause of the palpitations and the patient’s health.
Doctors usually suggest prescription drugs for severe or frequent palpitations. They also consider symptoms like dizziness or chest pain. Starting medication should always be a doctor’s decision, based on the patient’s needs.
| Condition | Potential Medication | Considerations |
| Arrhythmia-induced palpitations | Beta-blockers, Anti-arrhythmic drugs | Monitor for side effects, adjust dosage as needed |
| Stress or anxiety-related palpitations | Anxiolytics, Beta-blockers | Short-term use recommended; address underlying causes |
| Palpitations due to other medical conditions | Varies based on underlying condition | Treat underlying condition; monitor palpitations |
In conclusion, treating heart palpitations needs a full approach. This includes understanding the cause, making lifestyle changes, and using medication when needed. With the help of healthcare providers, people can find relief from heart palpitations.
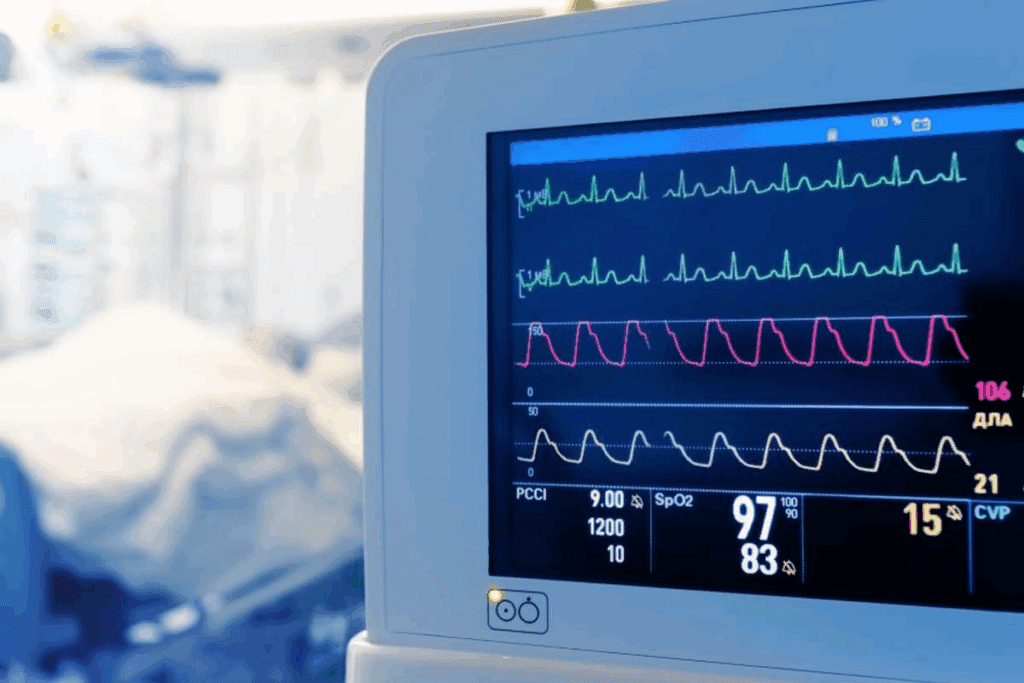
Tachycardia, or fast heart rate, can be managed with different drugs and treatments. We will look into these in detail. Managing tachycardia means controlling the heart rate and fixing the underlying causes. It needs a detailed and personalized plan.
In urgent situations, the main goal is to quickly slow the heart rate and ease symptoms. Intravenous beta-blockers, like metoprolol and propranolol, are often used. They slow the heart by blocking adrenaline’s effects.
For those with supraventricular tachycardia (SVT), adenosine is usually the first choice. It works fast and doesn’t last long. Sometimes, calcium channel blockers like verapamil are given intravenously to control the heart rate.
For managing tachycardia over time, oral drugs are used. Beta-blockers are key, with metoprolol and atenolol being common choices. They control the heart rate and lower the chance of tachycardia happening again.
Antiarrhythmic medications, like flecainide and propafenone, are used in some cases. They keep the heart rhythm normal by stabilizing the heart’s electrical activity.
For some, one drug isn’t enough to manage tachycardia well. In these cases, combination therapy is used. This means mixing two or more drugs with different ways of working. For example, mixing a beta-blocker with a calcium channel blocker can control the heart rate better than either one alone.
When using combination therapy, it’s important to watch patients closely for side effects and drug interactions. The right mix of medications and their doses must be chosen carefully for each patient’s needs and how they react to treatment.
The Vaughan-Williams classification is not complete. Other important drugs help manage arrhythmias. These drugs are used in addition to the ones listed in the classification.
Adenosine is a quick-acting drug for treating supraventricular tachycardia (SVT). It blocks the AV node, stopping SVT. Adenosine works fast and doesn’t last long, making it perfect for sudden SVT episodes. But, it can cause side effects like flushing and chest pain.
Digoxin helps control heart rate in atrial fibrillation, mainly in heart failure patients. It slows the heart by affecting the AV node. Digoxin is useful, but newer drugs have changed its role. It’s important to watch digoxin levels closely.
Ivabradine targets the If channel in the heart, reducing heart rate. It’s for patients with fast heart rates or heart failure. Ivabradine is a new option when beta-blockers don’t work. It needs careful use and monitoring.
In summary, adenosine, digoxin, and ivabradine are key in treating arrhythmias. Each drug has its own way of working and when to use it. Knowing about these drugs helps doctors give better care to patients with heart rhythm problems.
Antiarrhythmic medications are key in managing irregular heartbeats. But, they come with side effects and risks. It’s a delicate balance between their benefits and drawbacks.
Different types of antiarrhythmic drugs have unique side effects. Class I drugs, which block sodium channels, can cause stomach issues, dizziness, and worsen heart failure. For example, quinidine might lead to tinnitus, headaches, and nausea.
Class II drugs, or beta-blockers, are usually safe but can make you feel tired, cold, and depressed. Metoprolol and propranolol are common beta-blockers used for arrhythmias.
Class III drugs, like amiodarone, have serious side effects due to their complex nature. Amiodarone can harm the thyroid, lungs, and liver over time.
One major risk of antiarrhythmic therapy is proarrhythmic effects. This means the drug can make the arrhythmia worse. This risk is high with Class IC agents like flecainide and propafenone. It’s vital to monitor heart rhythm with ECGs.
Monitoring is key for patients on antiarrhythmic therapy. Regular ECGs, blood tests, and check-ups help adjust dosages and catch problems early. Also, these drugs can interact with other medications, like blood thinners and antibiotics. It’s important to review all medications carefully.
Understanding the side effects and risks of antiarrhythmic therapy helps healthcare providers manage arrhythmias better. This careful approach is essential for the best patient outcomes.
Managing cardiac arrhythmias requires a deep understanding of antiarrhythmic medications. We’ve seen how new drugs and treatments come from studying heart electrophysiology. This knowledge helps doctors treat arrhythmias better.
We’ve talked about different types of antiarrhythmic drugs. These include sodium channel blockers and beta-blockers. We’ve also looked at potassium and calcium channel blockers, as well as adenosine and ivabradine. Knowing about these drugs helps doctors choose the right treatment for each patient.
The study of arrhythmia management is always growing. New research brings better treatments for patients. As we learn more, we can use the right drugs to help patients. This way, treatment fits each patient’s needs perfectly.
Antiarrhythmic drugs help treat heart rhythm problems. They manage fast heart rates, palpitations, and irregular beats.
The Vaughan-Williams system groups antiarrhythmic drugs by how they work. It helps doctors pick the best treatment for patients.
There are four main classes. Class I blocks sodium channels, Class II are beta-blockers, Class III block potassium channels, and Class IV block calcium channels.
Class I drugs include quinidine, procainamide, lidocaine, mexiletine, flecainide, and propafenone.
Beta-blockers slow the heart rate and reduce contraction force. They help manage arrhythmias like atrial fibrillation and supraventricular tachycardia.
Metoprolol, propranolol, atenolol, and carvedilol are common beta-blockers for arrhythmias.
Amiodarone treats various arrhythmias, including atrial fibrillation and ventricular tachycardia. It’s a powerful medication.
Calcium channel blockers slow the heart rate and reduce contraction force. They help manage arrhythmias like supraventricular tachycardia.
Verapamil and diltiazem are examples of calcium channel blockers used for arrhythmias.
Adenosine treats acute supraventricular tachycardia. It quickly converts the heart rhythm back to normal.
Side effects vary by class and medication. They can include proarrhythmic effects, gastrointestinal issues, and fatigue.
They’re monitored with regular ECGs, blood tests, and clinical assessments. This ensures they’re safe and effective.
Yes, they can be used with cardioversion, ablation, or pacemakers to manage arrhythmias.
Lifestyle changes like avoiding triggers, reducing stress, and eating healthy can help manage palpitations. They may reduce the need for medication.
Seek medical help for persistent or severe palpitations, chest pain, shortness of breath, or dizziness.
National Center for Biotechnology Information. (2025). 15 Antiarrhythmic Drugs List Fast Heart Rate. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482322/)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us