
As a parent, it’s natural to worry when your child is sick. Knowing if they need antibiotics is key for their health. Antibiotics work on bacterial infections, but not on viral ones like the cold, so giving antibiotics for cold symptoms is usually not helpful.
At Liv Hospital, we use science to decide on treatments. So, how do you know if your child needs antibiotics? It’s important to talk to a doctor who can check your child and give a correct diagnosis, ensuring antibiotics are only used when truly needed.
Key Takeaways
- Antibiotics are only effective against bacterial infections.
- Viral infections, such as the common cold, do not require antibiotics.
- A proper diagnosis by a healthcare professional is critical.
- Evidence-based guidelines help decide if antibiotics are needed.
- Using antibiotics when not needed can cause harm.
Understanding Antibiotics and Their Purpose
As parents, knowing when to use antibiotics for kids is key. These medicines fight bacterial infections but not viral ones. It’s important to figure out what’s causing your child’s illness.

What Antibiotics Do and Don’t Treat
Antibiotics are strong against bacterial infections. They can help with pneumonia, strep throat, and some ear and sinus infections. But, they don’t work on viral infections like the cold or flu.
Types of Infections in Children
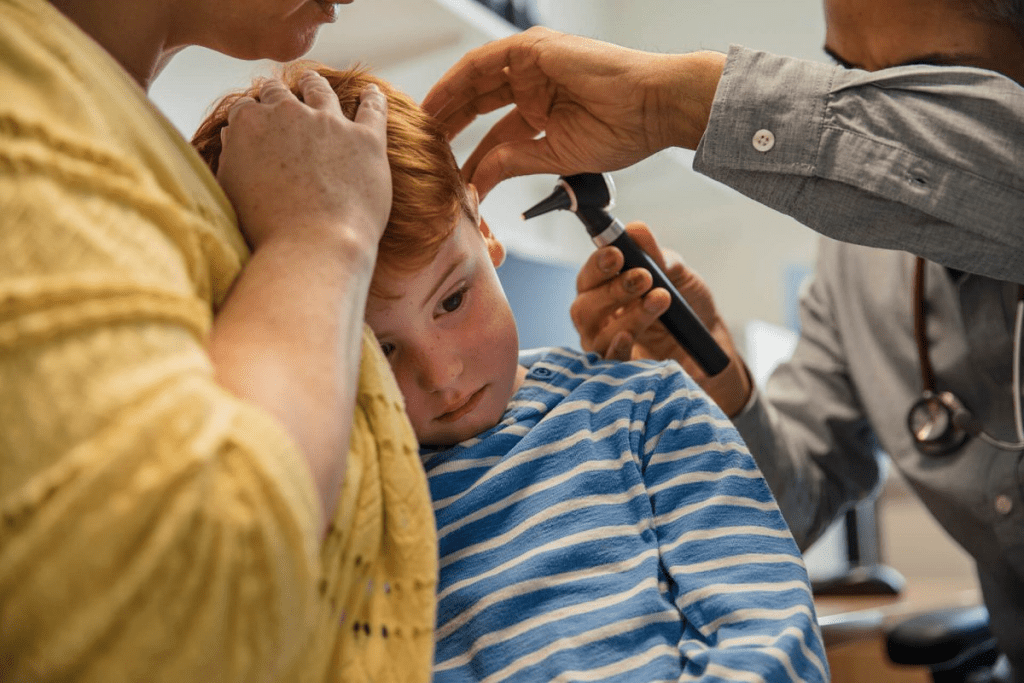
Children can get many infections, like ear and sinus problems, and pneumonia. Ear infections are a big reason for antibiotics in kids. But, not all ear infections need antibiotics because some are caused by viruses.
The Growing Concern of Antibiotic Resistance
Using children’s antibiotics too much is a big problem. It makes bacteria resistant to these medicines. The World Health Organization says antibiotics should only be used for 80% of common infections in kids.
We need to be careful with antibiotics. Working with doctors is important to use them wisely. This helps fight antibiotic resistance.
Common Childhood Conditions and Antibiotics for Cold
Understanding if antibiotics are needed for common childhood colds can be tough. Colds are caused by viruses, so antibiotics don’t work. It’s important to know if an infection is viral or bacterial to choose the right treatment.
Viral vs. Bacterial Infections
Viral infections, like the common cold, can’t be treated with antibiotics. Bacterial infections need antibiotics. Knowing the difference helps make better health choices for your child.
Most colds are viral and get better with rest, water, and over-the-counter meds. But sometimes a cold can turn into a bacterial infection. This might need antibiotics.
Why Most Colds Don’t Require Antibiotics
Antibiotics don’t work on viruses, and using them too much can lead to antibiotic resistance. This can create ‘superbugs’ that are hard to treat.
Always listen to your doctor about antibiotics. They can tell if your child needs them based on the infection type.
When a Cold Might Lead to a Secondary Bacterial Infection
Sometimes, a cold can turn into a bacterial infection like sinusitis, ear infections, or pneumonia. These might need antibiotics. Look out for signs like a long-lasting fever, severe headache, or trouble breathing.
If your child shows these symptoms, see a doctor right away. They can check your child and decide if antibiotics are needed.
5 Clear Signs Your Child May Need Antibiotics
As a parent, it can be tough to know if your child needs antibiotics. But there are clear signs to look for. Most childhood illnesses are viral and don’t need antibiotics. Yet, some signs might mean your child has a bacterial infection that needs treatment.
Persistent High Fever
A high fever that doesn’t go away is a key sign your child might need antibiotics. Fever is a natural response to infection. But, a very high or long-lasting fever could mean a bacterial infection.
For babies under 3 months, a fever above 100.4 °F (38 °C) is a warning sign. For older kids, a fever over 102.2 °F (39 °C) that lasts more than 2-3 days might mean a bacterial infection.
Specific Symptoms by Infection Type
Different infections have different symptoms. For example, a child with a urinary tract infection (UTI) might have painful urination and frequent trips to the bathroom. On the other hand, a child with strep throat might have a very sore throat, fever, and swollen lymph nodes.
Knowing these symptoms can help you figure out if your child needs antibiotics.
“The diagnosis of bacterial infections often relies on a combination of clinical symptoms and laboratory tests.”
Duration of Illness Beyond Expected Timeline
Most viral infections get better in a certain amount of time. If your child’s illness lasts longer than expected, it could be a sign of a bacterial infection. For example, if a cold lasts more than 7-10 days or gets worse, it might be a sign of something like sinusitis or pneumonia.
Worsening Symptoms After Initial Improvement
Sometimes, a child might seem better at first but then get worse. This can be a sign of a secondary bacterial infection. For instance, a child with an initial viral pneumonia might later develop bacterial pneumonia, which needs antibiotics.
Knowing these signs can help you make better decisions about your child’s health. If you’re worried about your child’s symptoms or think they might need antibiotics, always talk to a healthcare professional.
7 Conditions That Usually Don’t Require Antibiotics
Many common childhood illnesses don’t need antibiotics. Knowing which ones helps avoid unnecessary use. Antibiotics don’t work on viral infections. This knowledge helps fight antibiotic resistance and keeps our children healthy.
Common Colds and Viral Upper Respiratory Infections
Most colds and upper respiratory infections are viral, not bacterial. They usually get better on their own in a week or two. Using antibiotics for these can harm your child and make bacteria resistant to them. For more info, check Cleveland Clinic’s page on the common.
Most Cases of Sore Throat
Sore throats are common in kids and are usually caused by viruses. Unless it’s strep throat, antibiotics aren’t needed. Strep throat is diagnosed with a throat swab. If it’s not strep, the sore throat is likely viral and will get better without antibiotics.
Bronchitis in Children
Bronchitis is an inflammation of the bronchial tubes, often viral. Antibiotics don’t work on viral bronchitis. Treatment aims to ease symptoms and help the body recover naturally.
Viral Gastroenteritis
Viral gastroenteritis, or stomach flu, affects the stomach and intestines. It causes diarrhea, vomiting, and stomach cramps. Antibiotics won’t help, so treatment focuses on managing symptoms and preventing dehydration.
Knowing about these common conditions can ease worries and cut down on antibiotic use. Always talk to a healthcare provider to figure out the best treatment for your child. When it comes to antibiotics for babies under 6 months or antibiotics for babies, always follow the doctor’s advice for safe treatment.
The Risks of Unnecessary Antibiotic Use in Children
Using antibiotics when not needed can harm children’s health. It’s important to know these risks to protect our kids. This helps us make better choices for their health.
Impact on the Developing Microbiome
Antibiotics can mess with a child’s gut bacteria. They upset the balance of gut bacteria, which is key for health. This can cause stomach problems and affect the immune system.
Connection to Asthma and Allergies
Studies show early antibiotic use may lead to asthma and allergies. The exact reasons are being researched. But, it’s thought that changing the microbiome is a big part. Cutting down on antibiotics might help prevent these issues.
Side Effects and Adverse Reactions
Antibiotics can have side effects in kids. These include stomach issues and allergies. Parents should watch for these signs when antibiotics are given.
Contributing to Antibiotic Resistance
Another big worry is antibiotic resistance. Overusing antibiotics lets bacteria become resistant. This makes treating infections harder. It’s a big problem worldwide that needs careful handling of antibiotics.
Knowing these risks helps us use antibiotics wisely. This protects our kids and the community. We should work with doctors to make sure antibiotics are used correctly.
Working With Your Healthcare Provider
Deciding if your child needs antibiotics is a big decision. Working closely with their healthcare provider is key. This ensures your child gets the best care for their condition.
Questions to Ask During the Appointment
Ask questions during the appointment to understand your child’s diagnosis and treatment plan. Some important questions include:
- What is the likely cause of my child’s symptoms?
- Are antibiotics necessary, and if so, why?
- What are the possible side effects of the antibiotic?
- How long will my child need to take the antibiotic?
- What signs should I look for to see if the treatment is working?
Understanding Watchful Waiting
Watchful waiting is when healthcare providers closely watch your child’s condition without antibiotics right away. They use this when the condition might get better on its own or when they’re not sure of the diagnosis.
It’s important to follow your healthcare provider’s advice during watchful waiting. They’ll tell you when to seek more medical help if your child’s symptoms get worse or don’t get better.
When to Follow Up If Symptoms Don’t Improve
If your child’s symptoms don’t get better or get worse during watchful waiting, you need to follow up with their healthcare provider. This appointment lets the provider check on your child’s condition and change the treatment plan if needed.
To get ready for the follow-up, keep a record of your child’s symptoms. Include their temperature, any changes in their condition, and any medicine they’ve taken.
The Importance of Completing Prescribed Antibiotic Courses
If your child is given antibiotics, it’s important to finish the whole course as told by their healthcare provider. Stopping antibiotics early can cause antibiotic resistance. This makes infections harder to treat in the future.
Finishing the antibiotic course makes sure the infection is fully gone. This reduces the chance of complications or needing more treatment.
Conclusion: Making Informed Decisions About Your Child’s Health
Deciding on your child’s health, like when to use antibiotics, is a big job. Knowing when antibiotics are needed and the dangers of using them too much is key. Working closely with doctors helps protect your child’s health and fights antibiotic resistance worldwide.
At Liv Hospital, we’re here to help with the latest medical info and caring support. Using antibiotics wisely in kids is vital. It keeps them working well and reduces risks.
Being well-informed and active helps keep your child safe and healthy. Making smart choices about antibiotics is what’s best for them.
FAQ’s:
What are antibiotics and how do they work?
Antibiotics are medicines that fight bacterial infections. They either kill the bacteria or stop them from growing. But they don’t work against viral infections.
How can I tell if my child’s infection is viral or bacterial?
Knowing the difference between viral and bacterial infections is key. Look for signs like persistent high fever and specific symptoms. Illnesses that last longer or get worse after getting better might be bacterial.
Do children with colds need antibiotics?
Most colds are caused by viruses, so antibiotics don’t help. But, sometimes a cold can turn into a bacterial infection like sinusitis or pneumonia. Then, antibiotics might be needed.
What are the risks of giving my child antibiotics unnecessarily?
Giving antibiotics when not needed can harm your child’s microbiome. It might increase the risk of asthma, allergies, and other immune problems. It also makes infections harder to treat because of antibiotic resistance.
How can I work effectively with my child’s healthcare provider regarding antibiotic use?
Ask important questions during appointments and understand the treatment plan. Know when to follow up if symptoms don’t get better. Always finish the antibiotic course as directed.
What is watchful waiting, and when is it appropriate?
Watchful waiting means watching symptoms before deciding on antibiotics. It’s good for conditions that might get better on their own or when the diagnosis is unsure.
Can antibiotics prevent complications from a cold?
Antibiotics can’t prevent cold complications if the cold is viral. But if a bacterial infection develops, antibiotics might be needed to treat it.
Are there any long-term effects of antibiotic use in children?
Using antibiotics too much can lead to long-term problems. It might increase the risk of asthma, allergies, and antibiotic resistance. It’s important to use antibiotics wisely.
How do I know if my child’s condition requires antibiotics?
Look for signs of bacterial infection, like persistent high fever and specific symptoms. If the illness lasts longer or gets worse, it might need antibiotics. Always check with your child’s healthcare provider.
REFERENCES:
- Intermountain Healthcare. (2025). Acute Otitis Media (ear infection), pediatric. Provides antibiotic dosing schedules for amoxicillin and alternatives depending on allergies and severity, highlighting individualized treatment approaches in line with AAP guidelines. Retrieved fromhttps://intermountainhealthcare.org/ckr-ext/Dcmnt?ncid=522927223


































