Last Updated on November 26, 2025 by Bilal Hasdemir
We are dedicated to top-notch care through cutting-edge medical procedures. Endovascular Aneurysm Repair (EVAR) is a groundbreaking method for treating abdominal aortic aneurysms. This surgery is done without a big cut, using a stent graft inserted through the femoral arteries. It blocks the aneurysm from blood flow, greatly lowering the chance of it bursting.
Aortic aneurysm endovascular repair has changed how we treat aortic aneurysms by being a less invasive option. It leads to quicker recovery times and fewer side effects. The EVAR procedure requires great skill and knowledge of blood vessel anatomy.
Key Takeaways
- EVAR is a minimally invasive technique for treating abdominal aortic aneurysms.
- The procedure involves inserting a stent graft via the femoral arteries.
- EVAR reduces the risk of aneurysm rupture by excluding it from blood flow.
- This technique offers shorter recovery times compared to traditional open surgery.
- Precision and a deep understanding of vascular anatomy are key for EVAR success.
Understanding Abdominal Aortic Aneurysms (AAA)
It’s key to understand abdominal aortic aneurysms (AAA) for good vascular health. AAA is when the aorta in the belly gets too big. This is a serious condition.
Definition and Pathophysiology
An AAA is when the aorta in the belly gets bigger than 3 cm. This happens when the aortic wall gets weak. This weakness can come from genes or the environment.
The process behind AAA is complex. It involves inflammation, enzymes breaking down the wall, and stress on the aorta.
Risk Factors and Prevalence
Many things can make AAA more likely. These include being older, male, smoking, high blood pressure, and family history of aneurysms.
Smoking is a big risk factor. It makes AAA more likely and can make it grow faster.
AAA is more common in older men and smokers.
Indications for Intervention
Doctors decide when to fix an AAA based on size, growth, and health. Repair is often needed for aneurysms over 5.5 cm or growing fast.
Endovascular aneurysm repair (EVAR) is a common choice. It’s less invasive and has quicker recovery than open surgery.
Benefits of Aortic Aneurysm Endovascular Repair

EVAR treats AAA in many ways, from less pain during surgery to lower heart risks. It’s clear why many choose EVAR for their treatment.
Reduced Perioperative Morbidity and Mortality
EVAR cuts down on risks during and right after surgery. It doesn’t need a big cut in the belly, which means less damage to tissues. This makes EVAR safer, even for those with health issues.
Key advantages of EVAR include:
- Lower risk of perioperative complications
- Reduced need for blood transfusions
- Shorter hospital stays
Lower Cardiac Risk (1-5%)
EVAR also means less heart risk than open surgery. It’s gentler on the heart, which helps those with heart problems. The heart risk with EVAR is just 1-5%, making it safer for many.
Short-term Survival Advantages
Plus, EVAR can lead to better survival chances in the short term. It lowers the risk of death and serious problems right after surgery.
In summary, EVAR is a great choice for treating AAA. Knowing its benefits helps doctors and patients make better decisions together.
Patient Selection and Preoperative Assessment
The success of EVAR depends on choosing the right patients and doing detailed checks before surgery. We look at many factors to see if a patient is a good fit for the procedure.
Anatomical Considerations
It’s important to check if a patient’s body is right for EVAR. We look at the aortic aneurysm’s size, shape, and location. We also check the quality of the surrounding arterial wall.
The aneurysm’s neck is key. We check its length, diameter, and angle. This ensures the stent graft can seal properly.
Required Imaging Studies
For planning, we use high-resolution computed tomography angiography (CTA). This gives us detailed views of the aneurysm and nearby blood vessels. It helps us measure the aneurysm’s dimensions and plan the stent graft.
Risk Stratification
It’s important to know who will benefit most from EVAR. We look at the patient’s health, including cardiac, pulmonary, and renal function. This helps us tailor our approach to each patient.
Contraindications for EVAR
Even though EVAR is effective, there are times when it’s not the best choice. This includes unsuitable aortic anatomy, significant renal impairment, and allergy to contrast agents. We carefully check each patient to see if EVAR is right for them.
By choosing the right patients and doing detailed checks before surgery, we can make EVAR more successful. This improves care for our patients.
“The key to successful EVAR lies in meticulous patient selection and thorough preoperative planning.”
Essential Equipment and Materials for EVAR
To do EVAR well, you need the right tools and materials. The quality of these tools is key to success.
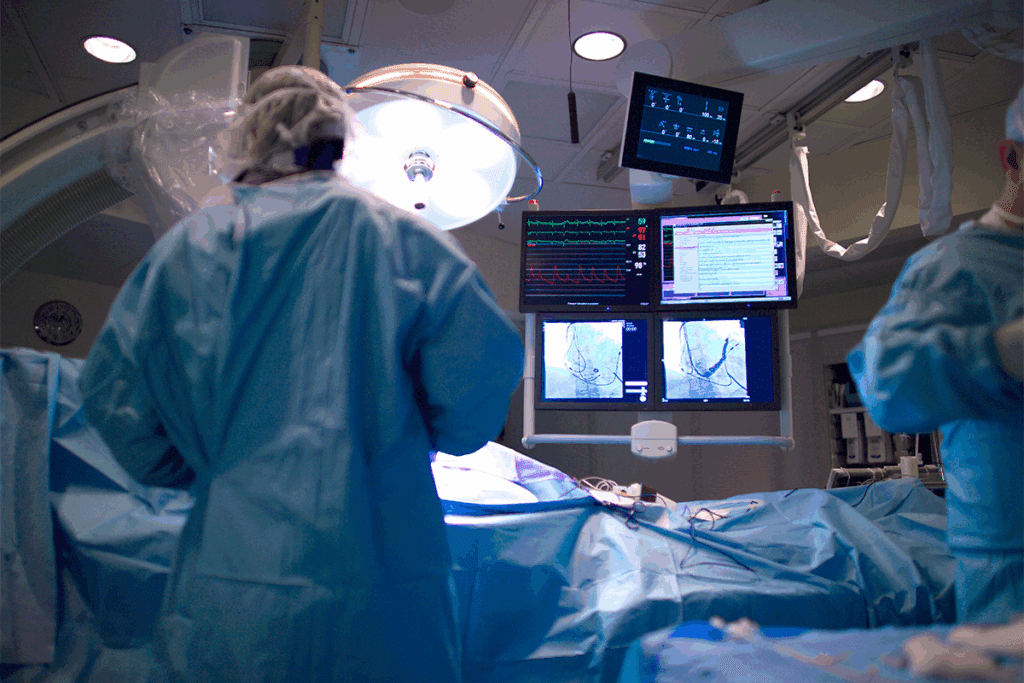
Advanced Imaging Systems
For EVAR, advanced imaging is vital. We use top-notch imaging to guide the procedure. This ensures the stent graft is placed correctly.
Fluoroscopy and digital subtraction angiography are our go-to technologies. They let us see the aorta and stent graft live, making adjustments as needed.
Endovascular Instruments
For EVAR, we need special tools to work in the blood vessels. These include guidewires, catheters, and sheaths in different sizes and shapes.
Choosing the right tools is key. It helps us navigate tricky anatomy and avoid problems.
Stent Graft Types and Selection Criteria
Choosing the right stent graft is a big decision in EVAR. There are many types, like main body grafts, extensions, and fenestrated or branched grafts for tough cases.
We look at the aneurysm’s size, location, and shape when picking a stent graft. Our goal is a tight seal and no endoleaks.
Operating Room Setup Requirements
A good operating room setup is essential for EVAR. It needs the right imaging gear, all the endovascular tools, and a team that works well together.
We make sure all equipment is ready and works before we start. This helps avoid problems and delays.
Preoperative Planning for Endovascular AAA Repair
Getting ready for EVAR is key to a good outcome. This step includes checking the patient’s body, picking the right stent grafts, and planning how to access the area.
Detailed Imaging Analysis Techniques
Imaging is a big part of getting ready. We use CT scans to look at the aneurysm’s size, shape, and how it fits with other parts of the body. “Good imaging is key for deciding if EVAR is right and for planning,” say top vascular surgeons.
We carefully look over the scans to spot any possible problems. We check the aortic neck, iliac arteries, and how to get to them.
Precise Graft Sizing and Configuration
Choosing the right graft size is very important. It helps avoid leaks and other issues. We use special software to measure the aorta and pick the best graft. Then, we adjust it to fit the patient’s body perfectly.
A study found that the right graft size and shape are key for a lasting fix and fewer problems.
Access Route Planning Strategies
Figuring out how to get to the aorta is also important. We look at the iliac and femoral arteries to find the best spot. We check their size, twists, and hardening.
- Identifying possible access points
- Looking at the risk of blood vessel problems
- Picking the best way to get in
Team Preparation and Briefing Protocols
Getting the team ready and briefed is essential. Before the surgery, we go over the patient’s details, talk about possible issues, and plan the approach.
“Good communication and teamwork are vital for a smooth and successful surgery,” our team says from their experience with tough EVAR cases.
Step-by-Step EVAR Surgical Procedure
Understanding the EVAR surgical procedure is key to its success. It’s a complex process that needs precision and skill.
Patient Positioning and Preparation
Getting the patient in the right position is vital. They lie on a special table that lets us see them clearly on a screen. Their arms are kept up to help us work.
We clean the area well and cover it with drapes. The patient gets anesthesia to stay comfortable and pain-free.
Femoral Artery Access Techniques
Getting to the femoral artery is a big step. We might use surgery or a needle to get there. It depends on the patient and what we think is best.
- Surgical cutdown lets us see and control the artery directly.
- Percutaneous access uses a needle and guidewire, then a closure device.
Guidewire and Catheter Navigation Methods
After we’re in, we guide wires and catheters to the aneurysm. This part needs careful watching on the screen and knowing the patient’s body well.
We pick the right tools for each patient. This helps us do the job right.
- We start with a basic guidewire and catheter.
- Then, we switch to stiffer ones for the stent graft.
Main Body Deployment Process
Putting in the stent graft’s main part is a big moment. We place it carefully, making sure it’s right next to the renal arteries and the aneurysm.
We put in the main part first, then the other limb. We use special techniques to make sure it’s in the right spot and works well.
Key considerations during main body deployment include:
- Getting it right next to the renal arteries.
- Setting it up so we can easily add the other limb.
- Making sure it doesn’t twist or bend.
Advanced AAA Techniques in Complex Anatomies
Dealing with complex AAAs requires new EVAR methods. This includes using fenestrated and branched grafts. These methods are needed because standard EVAR can’t handle certain complex cases. This is due to issues like short necks or major branch vessel involvement.
Fenestrated EVAR for Juxtarenal Aneurysms
Fenestrated EVAR is a good option for juxtarenal aneurysms. These aneurysms are close to or involve the renal arteries. The technique customizes the stent graft with special fenestrations. These align with the patient’s renal and visceral arteries, keeping blood flow going.
Fenestrated EVAR is useful for aneurysms that standard EVAR can’t treat. This is because of short or angled necks. The process needs careful planning and precise execution to place the graft correctly.
Branched Endografts for Thoracoabdominal Aneurysms
Branched endografts are a big step forward for TAAAs. These aneurysms affect both the thoracic and abdominal aorta and often touch critical branch vessels. The grafts have branches for the patient’s vital arteries, allowing for blood flow while excluding the aneurysm.
Using branched endografts needs detailed planning. This includes 3D aortic anatomy scans and precise graft sizing. It’s a good option for those with extensive TAAAs who face high risks with open surgery.
Chimney and Snorkel Techniques
The chimney and snorkel techniques help keep blood flow to branch vessels during EVAR. They involve placing a stent graft alongside the main graft. This creates a “chimney” for blood flow into the branch vessel.
These methods offer flexibility and can be lifesaving. But, they also come with challenges like endoleaks and the need for careful planning. We decide on a case-by-case basis, based on the patient’s anatomy and condition.
Critical Intraoperative Considerations
Intraoperative considerations are key to the success and safety of aortic aneurysm endovascular repair. We must manage several important factors during the EVAR procedure. This ensures a good outcome for the patient.
Detecting and Managing Endoleaks
Endoleaks are a big problem in EVAR that can cause aneurysm rupture if not fixed. We divide endoleaks into five types based on their cause. These include Type I (seal issues), Type II (branch flow), Type III (graft failure), Type IV (porosity), and Type V (endotension).
To spot endoleaks, we use completion angiography. This method gives us a real-time look at the graft’s placement and any leaks. The way we handle endoleaks depends on their type and how bad they are.
| Endoleak Type | Description | Management Strategy |
| Type I | Inadequate seal at graft ends | Additional ballooning or stenting |
| Type II | Retrograde flow from branches | Embolization or observation |
| Type III | Graft failure | Relining with a new graft |
Ensuring Proper Proximal and Distal Seal Zones
Good seal zones are vital to avoid endoleaks and ensure EVAR’s long-term success. We achieve this by carefully sizing and placing the stent graft. We consider the aneurysm neck and iliac arteries’ anatomy.
Preserving Renal and Visceral Perfusion
Keeping blood flow to the renal and visceral arteries is key to prevent ischemic issues. We use techniques like fenestrated or branched endografts. This keeps blood flowing to these vital areas.
- Fenestrated EVAR for juxtarenal aneurysms
- Branched endografts for thoracoabdominal aneurysms
Completion Angiography Assessment
Completion angiography is a key part of the EVAR procedure. It lets us check if the repair was successful. We look at the graft’s position, the arteries’ patency, and any endoleaks.
By managing these intraoperative factors well, we can improve EVAR’s outcomes and patient safety.
Potential Complications and Troubleshooting
Potential complications can happen during or after EVAR. We need to manage them carefully. We will talk about common problems during surgery, when to switch to open repair, handling vascular access issues, and fixing technical failures.
Common Intraoperative Complications
Intraoperative complications during EVAR can be tough. These include:
- Endoleaks: Immediate detection and management are key to avoid more problems.
- Vascular injuries: These can happen during access or device deployment, needing quick repair.
- Device malfunction: Though rare, having a plan for these events is essential.
Emergency Conversion to Open Repair Indications
In some cases, emergency conversion to open repair is needed. This includes:
- Uncontrollable bleeding
- Significant vascular injury
- Device failure that can’t be fixed endovascularly
We must be ready for these situations, with a clear plan and the right surgical skills.
Vascular Access Complications Management
Vascular access complications can happen, including:
- Hemorrhage
- Thrombosis
- Dissection
Prompt recognition and management of these issues are critical. Using ultrasound-guided access and careful closure methods can reduce these risks.
Technical Failures and Evidence-Based Solutions
Technical failures, though rare, can be serious. Evidence-based solutions include:
- Advanced imaging to guide treatment
- Specialized endovascular tools and devices
- Working with a team to solve complex problems
By knowing these complications and having ways to fix them, we can make EVAR procedures better.
Postoperative Care and Follow-up Protocol
Postoperative care and follow-up are key to EVAR success. They help monitor recovery, catch early complications, and ensure long-term health.
Immediate Postoperative Management
Right after surgery, care focuses on keeping the patient stable and watching for immediate issues. This often happens in an ICU or step-down unit, based on the patient’s health and the surgery’s complexity.
Key aspects of immediate postoperative management include:
- Monitoring vital signs and hemodynamic stability
- Assessing for signs of endoleak or other procedural complications
- Managing pain and discomfort
- Initiating appropriate anticoagulation or antiplatelet therapy as needed
Surveillance Imaging Schedule
A set schedule for surveillance imaging is vital. It helps catch complications and check the endograft’s long-term health. The schedule includes:
- Initial postoperative imaging (e.g., CT angiography) before discharge or within 30 days
- Follow-up imaging at 6, 12, and 24 months post-procedure
- Annual imaging thereafter, or as dictated by the patient’s clinical status and initial findings
Surveillance imaging is key for spotting endoleaks and checking the aneurysm sac size and graft patency.
Long-term Follow-up Considerations
Long-term follow-up after EVAR is essential for patient health management. It includes:
- Regular clinical assessment to monitor for symptoms or signs related to the aneurysm or endograft
- Ongoing surveillance imaging as outlined in the scheduled follow-up
- Management of risk factors for aneurysm progression or graft-related complications
Managing Late Complications
Late complications like endoleaks, graft migration, or aneurysm rupture can happen. Effective management involves:
- Prompt identification of complications through surveillance imaging and clinical assessment
- Intervention as necessary, which may include additional endovascular procedures or conversion to open repair in complex cases
- Patient education on signs and symptoms that warrant immediate medical attention
By following a detailed postoperative care and follow-up plan, healthcare providers can improve patient outcomes and ensure EVAR success.
Conclusion: Optimizing Outcomes in EVAR Procedures
Improving results in EVAR procedures needs a detailed plan. This includes choosing the right patients, planning carefully before surgery, using precise techniques, and caring for patients well after surgery. Knowing how to handle abdominal aortic aneurysms and the benefits of endovascular repair helps a lot.
We talked about the role of advanced imaging, different stent grafts, and setting up the operating room. The guide to EVAR surgery shows how important it is to do everything right, from starting to finishing the procedure.
By taking a complete approach to EVAR, doctors can reduce problems and get the best results for patients. As we keep improving our methods and tools, making EVAR procedures better is a key goal. This goal helps us give patients better care and improve their chances of survival.
FAQ
What is EVAR and how does it differ from open surgical repair?
EVAR, or Endovascular Aneurysm Repair, is a new way to treat aortic aneurysms. It’s less invasive than open surgery. A stent graft is inserted through small incisions in the groin, guided by imaging. This method helps avoid rupture risks.
What are the benefits of choosing EVAR over open repair for AAA?
EVAR has many advantages. It lowers the risk of complications and death right after surgery. It’s also safer for the heart. It’s great for patients with complex cases or high risks for open surgery.
What are the key anatomical considerations for patient selection in EVAR?
Important factors include the aneurysm’s size and shape. The length and diameter of the seal zones matter too. Any bends or twists in the aorta are also considered. These help decide if EVAR is right for the patient and what stent graft to use.
What imaging studies are required before undergoing EVAR?
Detailed imaging like CT angiography is key. It shows the aneurysm’s details and the aorta’s condition. This helps pick the right stent graft size and design.
How is risk stratified for patients undergoing EVAR?
Doctors assess the patient’s health before surgery. They look at the heart, kidneys, and lungs. This helps find patients at higher risk and plan better care.
What are the most common complications associated with EVAR?
Common issues include endoleaks and access problems. Post-surgery, endoleaks and stent graft migration can happen. Kidney problems are also a risk.
How are endoleaks detected and managed during EVAR?
Doctors use imaging during and after surgery to find endoleaks. Treatment depends on the type and severity. It can range from watching it to more invasive methods.
What is the typical follow-up protocol after EVAR?
Patients get regular imaging checks. This starts with a CT scan right after surgery. Then, scans at 1, 6, and 12 months, and yearly after. This helps catch any problems early.
Can EVAR be used for complex or thoracoabdominal aneurysms?
Yes, EVAR can treat complex cases. Techniques like fenestrated EVAR and branched endografts help. They offer hope for patients with tough anatomy.
What is the role of preoperative planning in ensuring the success of EVAR?
Planning is vital. It includes detailed imaging and precise graft sizing. It ensures the stent graft fits well, making the procedure more likely to succeed.
References:
- Björck, M., Wanhainen, A., & Koelemay, M. (2024). Endovascular aneurysm repair: Current status and future perspectives. The Lancet, 403(10387), 753-765. Retrieved fromhttps://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02027-7/fulltext





