Last Updated on November 26, 2025 by Bilal Hasdemir

Understand common aortic stent complications after endovascular aneurysm repair and how to manage them. Endovascular aneurysm repair (EVAR) has changed how we treat aortic aneurysms. It offers a minimally invasive alternative to open surgery. EVAR has greatly improved early survival and health outcomes. But, it leads to more follow-up surgeries than open surgery.
It’s important to know about the complications of EVAR, like issues with aortic stent surgery. Hospitals like Liv Hospital are leading the way. They use strict protocols and focus on the patient to get the best results for aortic aneurysm treatment.
Key Takeaways
- EVAR is a minimally invasive alternative to traditional aortic aneurysm surgery.
- Despite its benefits, EVAR is associated with a higher rate of reinterventions.
- Understanding the possible complications is key for the best patient results.
- Liv Hospital uses strict protocols to handle EVAR complications.
- Putting the patient first is vital for managing issues after aortic aneurysm surgery.
The Evolution of Endovascular Aneurysm Repair

Endovascular aneurysm repair (EVAR) has changed how we treat aortic aneurysms. It’s a less invasive option compared to open surgery. This change comes from new medical technology and understanding the benefits of less invasive methods.
From Open Surgery to Minimally Invasive Approaches
Old treatments for aortic aneurysms were open surgeries. These surgeries needed big cuts and took a long time to recover from. EVAR, on the other hand, uses small cuts in the groin. This method causes less damage and helps patients heal faster.
Research shows EVAR lowers early death and sickness rates compared to open surgery. This makes EVAR a good choice for many patients.
Basic Principles of EVAR Procedure
The EVAR procedure uses a stent graft to block the aortic aneurysm from growing or rupturing. The stent graft goes through the femoral arteries and is guided to the aneurysm. The key to a successful EVAR procedure is getting the stent graft’s size and placement right.
Patient Selection Criteria
Not every patient can have EVAR. Doctors look at the size and shape of the aneurysm and the patient’s health. Those with complex aneurysms or serious health issues might need a different plan. Careful patient selection is key to good results and fewer problems.
Overview of Aortic Stent Complications: Incidence and Impact
Endovascular aneurysm repair (EVAR) can lead to several complications. These issues can greatly affect how well the procedure works.
Complication Rates in Clinical Studies
Studies have shown different rates of complications after EVAR. Common issues include endoleaks, injuries to the access vessel, and stent migration.
Short-term vs. Long-term Complications
Complications from EVAR can be short-term or long-term. Short-term problems happen during or right after the procedure. Long-term issues may show up months or years later.
Mortality and Morbidity Statistics
Looking at how many people die or suffer from EVAR is key. While EVAR is mostly safe, there are risks. These can affect how well the patient does.
The problems caused by aortic stent complications show why careful planning and follow-up are so important.
Endoleaks: The Most Frequent Post-EVAR Complication
Endoleaks are a common issue after EVAR. They involve blood flow outside the stent graft but inside the aneurysm sac. This can increase pressure and rupture risk.
Classification of Endoleak Types
There are five types of endoleaks based on their cause:
- Type I: Leak at the stent graft attachment site
- Type II: Retrograde flow from aorta branches
- Type III: Stent graft failure
- Type IV: Graft porosity
- Type V: An increase in aneurysm sac size without a leak
Type II endoleaks are the most common. They often come from retrograde flow from lumbar arteries or the inferior mesenteric artery.
Clinical Significance and Risk of Rupture
The risk of endoleaks depends on their type and if the sac is expanding. Type I and III endoleaks are high-risk. They can increase pressure in the aneurysm sac and lead to rupture.
| Endoleak Type | Risk Level | Management Approach |
| Type I | High | Immediate intervention |
| Type II | Variable | Surveillance or embolization |
| Type III | High | Immediate intervention |
Detection Methods and Surveillance Protocols
Imaging like ultrasound, CT angiography, or MRI is used to find endoleaks. Surveillance plans include imaging at 1, 6, and 12 months after EVAR. Then, annual checks are done.
Understanding endoleaks is key to managing patients after EVAR. By classifying them correctly and using the right surveillance, doctors can lower risks and improve patient care.
Access Vessel Injuries During EVAR
Access vessel injuries are a big worry during Endovascular Aneurysm Repair (EVAR) procedures. These injuries can cause serious problems, affecting how well patients do and raising the risk of serious health issues.
Iliac Artery Complications
Iliac artery problems are common during EVAR. Dissection or rupture of the iliac artery can happen when devices are moved inside the vessel. Good planning before surgery and choosing the right device sizes are key to reducing these risks.
Femoral Artery Access Site Problems
Femoral artery access site issues are another big concern. Problems can include hematoma formation, pseudoaneurysm, and infection. Using careful closure techniques and good care after surgery can help avoid these problems.
Prevention Strategies for Vascular Access Injuries
To prevent vascular access injuries, we need a few steps. This includes thorough checks before surgery of the access vessels, choosing the right device sizes, and using precise techniques during deployment. Also, watching patients closely after surgery is key to spotting and handling any issues early.
By knowing the risks of access vessel injuries during EVAR and using good prevention strategies, doctors can make patients’ outcomes better. This helps lower the number of problems linked to aortic stent surgery and endovascular aneurysm repair.
Stent Graft Migration: A Serious Long-term Concern
Stent graft migration is a big worry with EVAR. It happens when the stent graft moves from its original spot in the aorta. This can cause serious problems like endoleaks and rupture, which might need quick medical help.
Defining and Measuring Migration
Migration is when the stent graft moves more than 10 mm from where it was placed. It’s important to measure this accurately. Doctors use CT scans to do this.
Anatomical Risk Factors
Some body features can make stent graft migration more likely. These include aortic neck angulation, short or irregular aortic necks, and large aneurysm diameter. Knowing these can help doctors predict and maybe prevent migration.
Hemodynamic Forces Contributing to Migration
Blood flow’s pulsatile nature and pressure on the stent graft can make it move. Hypertension and aortic morphology can make these forces stronger, raising the risk of migration.
Clinical Consequences of Displaced Stents
The effects of stent graft migration can be very serious. It can cause endoleaks, where blood leaks into the aneurysm sac, leading to rupture. So, it’s key to watch closely and act fast to manage migration and avoid bad outcomes.
Structural Failure and Stent Fracture
Stent fractures and structural failure are big worries after endovascular aneurysm repair (EVAR). The stent graft’s durability is key for the procedure’s success.
Mechanisms of Material Fatigue
Material fatigue causes stent fractures. Blood flow and artery pulsation stress the stent over time. Stent fractures often happen at high stress spots, like where stents overlap or near graft edges.
High-Risk Anatomical Configurations
Some body shapes raise the risk of stent fracture. This includes aortic necks that are twisted or angled. People with these shapes need more watchful care to spot fractures early.
Detection Challenges in Imaging Surveillance
Finding stent fractures in imaging tests is hard. High-tech scans like CT angiography are needed. But, even with these, small fractures might be missed.
Management of Fractured Components
Handling stent fractures depends on the fracture’s severity and where it is. In some cases, more procedures might be needed to fix the stent or deal with problems.
| Management Strategy | Description | Indications |
| Endovascular Reinforcement | Adding more stent grafts or parts to fix the broken area | Symptomatic fractures or those at high risk of migration or endoleak |
| Surveillance | Keeping a close eye with regular scans to check the fracture and any problems | Asymptomatic fractures with low risk of immediate problems |
| Conversion to Open Repair | Surgery to take out the stent graft and put in a new one | Complex fractures not fixable with endovascular methods or with big complications |
In summary, knowing about stent fractures, their risks, and how to manage them is vital for better EVAR outcomes. By spotting high-risk patients and using the right watch and treatment plans, doctors can lower the risks of stent fractures.
Renal Complications After Aortic Stent Placement
After EVAR, patients face risks like contrast-induced nephropathy and renal artery occlusion. These issues can greatly affect their health and life quality. It’s important to know about these risks and how they happen to manage them well.
Contrast-Induced Nephropathy
Contrast-induced nephropathy (CIN) is a known risk after endovascular aneurysm repair (EVAR). It happens because of contrast agents used during the procedure. CIN can cause a temporary or permanent drop in kidney function.
To lower CIN risk, use less contrast and keep patients well-hydrated before and after the procedure. Monitoring kidney function after EVAR is key for catching and treating CIN early.
Renal Artery Occlusion
Renal artery occlusion is another issue that can happen after aortic stent placement. It occurs when the stent blocks the renal artery, reducing blood flow to the kidneys.
To avoid renal artery occlusion, place the stent carefully and plan well before the procedure. Imaging after EVAR is vital to spot any stent or renal artery problems.
Progression to Dialysis-Dependent Renal Failure
In severe cases, EVAR complications can lead to dialysis-dependent renal failure. This is a serious health decline, needing lifelong dialysis or a kidney transplant.
To stop renal failure from getting worse, choose patients carefully for EVAR, do the procedure with care, and take good care of them afterward. Long-term monitoring is needed to watch kidney function and fix any problems quickly.
It’s vital to understand and manage kidney problems after aortic stent surgery to improve patient results. By knowing the risks and taking steps to reduce them, doctors can make EVAR safer and more effective.
Neurological Aortic Stent Complications
Neurological issues after endovascular aneurysm repair (EVAR) worry both patients and doctors. These problems can greatly affect a person’s life quality and results after the surgery.
Stroke Following EVAR
Stroke is a severe neurological issue that can happen after EVAR. It can be caused by debris or thrombus during the procedure. Risks include having heart or brain disease before surgery, complex aneurysm shapes, and how the procedure is done.
Spinal Cord Ischemia and Paraplegia
Spinal cord ischemia is another serious problem that can lead to paraplegia. This happens when blood flow to the spinal cord is cut off, often because of the stent graft covering or blocking important arteries. It’s important to know the spinal cord’s anatomy and keep its blood flow safe.
Management of Neurological Complications
Handling neurological issues after EVAR needs a team effort. Quick action and treatment are key. For stroke, treatments like thrombolysis or mechanical thrombectomy might be used. For spinal cord ischemia, keeping the spinal cord’s blood flow and possibly fixing the blood flow issue are important steps.
In summary, while EVAR is a good treatment for aortic aneurysms, it comes with big neurological risks. Knowing these risks and finding ways to lessen them are vital for better patient results.
Device-Specific Factors in Aortic Stent Complications
The design and materials of aortic stents are key in avoiding complications after EVAR. Different stents can greatly affect how well a patient does.
Unibody vs. Modular Designs
Aortic stents come in unibody and modular designs. Unibody designs are one piece, which might lower the chance of parts coming apart. On the other hand, modular designs are more flexible but might raise the risk of leaks because of possible mismatches or parts coming apart.
- Unibody designs: Reduced risk of component separation
- Modular designs: Greater flexibility and customization
Material Properties and Their Clinical Implications
The materials used in stents, like how durable and safe they are for the body, are very important. Stent graft material can impact the risk of the stent moving, leaks, and other issues.
Fixation Methods and Their Failure Modes
How a stent graft is fixed is also very important. Active methods, like hooks or barbs, can help prevent the stent from moving but might harm nearby tissues.
Comparative Outcomes Between Device Types
It’s vital to compare different stents to understand their risks and benefits. This helps doctors choose the best stent for each patient.
Knowing how different stents can cause problems helps doctors manage risks better. This leads to better results for patients after EVAR.
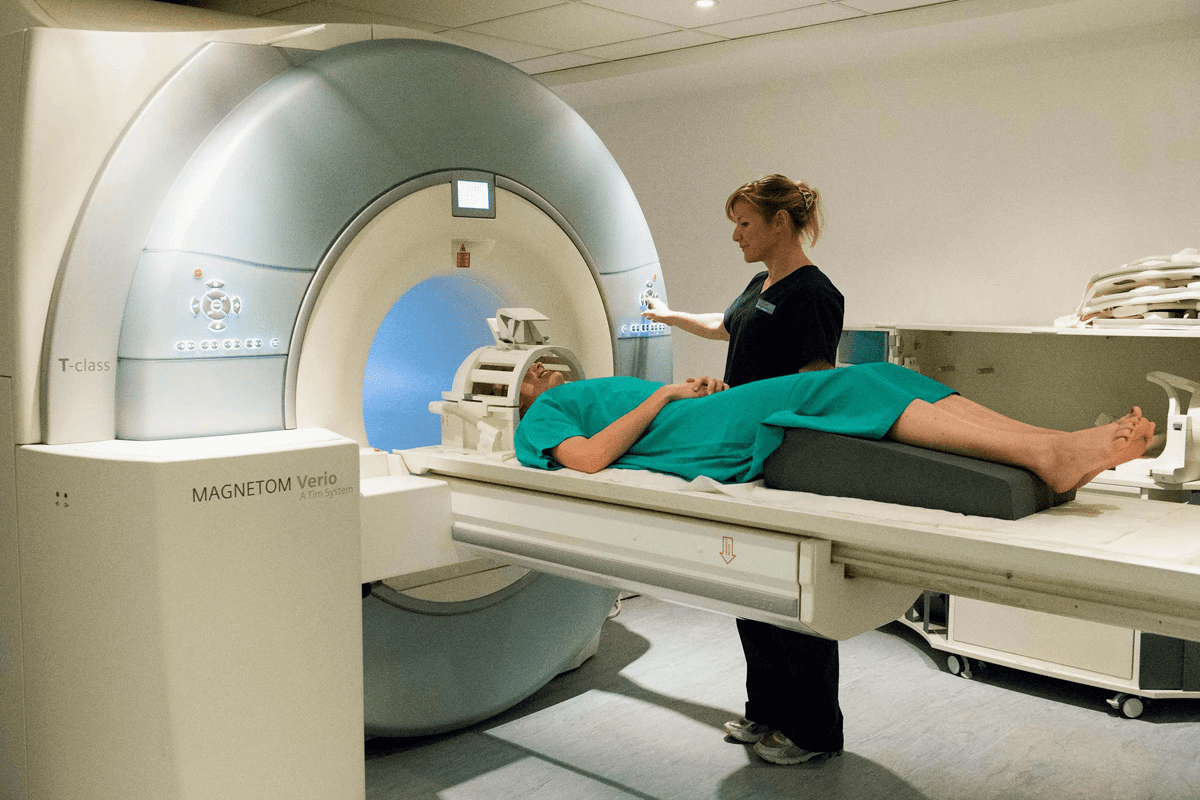
Post-EVAR Surveillance Protocols
After Endovascular Aneurysm Repair (EVAR), it’s key to watch for complications early. Regular checks help doctors fix problems fast, which helps patients get better.
Imaging Modalities for Follow-up
Several imaging methods are used for checking up after EVAR. These include Computed Tomography Angiography (CTA), Ultrasound, and Magnetic Resonance Angiography (MRA). CTA is seen as the best because it spots problems like endoleaks well.
Recommended Surveillance Schedules
Guidelines suggest a set schedule for follow-ups after EVAR. Patients usually get scans at 1, 6, and 12 months after the procedure. Then, they get checked every year. This plan can change if a patient’s risk is higher or if they have complications.
Signs Requiring Urgent Intervention
Some findings during checks need quick action. These include large or growing endoleaks, stent graft migration, and aneurysm sac enlargement. Finding these problems fast is key to avoiding rupture and other serious issues.
Following these surveillance guidelines helps doctors make EVAR procedures more successful in the long run.
Management Strategies for Aortic Stent Complications
Managing aortic stent complications well is key to better patient outcomes after endovascular aneurysm repair (EVAR). Issues like endoleaks, stent graft migration, and vascular access injuries need quick and effective treatment. This is to avoid more harm.
Endovascular Solutions
Many EVAR complications can be handled with endovascular techniques. For example, endoleaks can be treated with more stent grafts or embolization. Recent studies show these methods work well, often avoiding the need for open surgery.
| Complication | Endovascular Management | Success Rate |
| Endoleak | Additional stent grafts or embolization | 80-90% |
| Stent Graft Migration | Endovascular repositioning or additional stent grafts | 85-95% |
| Vascular Access Injuries | Angioplasty or stenting | 90% |
Conversion to Open Repair
Sometimes, conversion to open surgical repair is needed for complications that can’t be fixed endovascularly. This choice depends on the patient’s health and the complication’s nature.
Decision-Making Algorithm for Complication Management
Managing aortic stent complications needs a careful plan. It involves looking at the complication’s type and severity, the patient’s health, and the treatment options. Doctors must consider the risks and benefits of each approach to choose the best one.
Conclusion: Future Directions in Reducing EVAR Complications
It’s key to understand and manage issues after endovascular aneurysm repair (EVAR). Problems like endoleaks, stent graft migration, and structural failure can affect EVAR’s success. These complications can harm patients.
New research and tech advancements are important in fixing EVAR issues. Improvements in device design, materials, and imaging are being looked into. Also, better aortic stent surgery techniques are being developed. These changes aim to make EVAR more effective.
As the field grows, keeping up with new research and guidelines is critical. Healthcare workers need to stay informed to offer the best care for EVAR patients. This way, they can reduce risks and improve patient outcomes in the long run.
FAQ
What are the most common complications after Endovascular Aneurysm Repair (EVAR)?
Common issues after EVAR include endoleaks, injuries to the access vessels, and stent graft migration. Other problems are stent fracture, kidney issues, and neurological problems.
What is an endoleak, and how is it treated?
An endoleak is when there’s a leak around the stent graft in the aneurysm sac. Treatment depends on the leak’s type and severity. It might include watching it closely, trying to fix it with a procedure, or open surgery.
How can access vessel injuries be prevented during EVAR?
To avoid injuries to the access vessels, the procedure needs careful planning and execution. Using imaging and precise techniques when accessing the arteries helps a lot.
What are the risk factors for stent graft migration?
Stent graft migration risks include bad fixation, tough neck anatomy, and strong blood flow. People with these risks need regular checks to catch any movement.
How is stent fracture diagnosed and managed?
Stent fracture is found through regular imaging, like CT scans. Treatment depends on the fracture’s severity and location. It might involve fixing it with a procedure or open surgery.
What are the renal complications associated with EVAR, and how can they be mitigated?
EVAR can cause kidney problems like nephropathy from contrast and blockages in the renal arteries. To reduce these risks, doctors use less contrast, choose other imaging, and pick patients carefully.
What is the recommended surveillance protocol after EVAR?
After EVAR, regular imaging, like CT scans, is recommended. This helps catch any issues like leaks, migration, or fractures early.
Can EVAR complications be managed with endovascular interventions?
Yes, many EVAR problems can be fixed with procedures like coil embolization for leaks or adding more stent grafts for migration.
When is open repair necessary for EVAR complications?
Open surgery is needed for EVAR issues that can’t be fixed with procedures. This includes big leaks or migration that cause serious problems.
How do device design and materials impact the risk of EVAR complications?
The design and materials of the stent graft can affect the risk of problems. Some might be more likely to break or move because of how they’re made.
Reference
- National Heart, Lung, and Blood Institute. (2022, March 24). Aortic aneurysm – Treatment. U.S. Department of Health & Human Services, NIH. https://www.nhlbi.nih.gov/health/aortic-aneurysm/treatment