Last Updated on November 27, 2025 by Bilal Hasdemir

Spotting arteriosclerosis cardiovascular disease early can save lives. At Liv Hospital, we focus on top-notch, patient-focused care. Studies show arteriosclerotic heart disease is a major killer worldwide, hitting millions and raising heart attack and stroke risks.
Knowing the heart disease risk factors is vital for prevention and early catch. We teach our patients about their heart health, helping them manage their well-being.
Key Takeaways
- Arteriosclerosis cardiovascular disease is a big global health problem.
- Spotting it early is key to avoiding heart attacks and strokes.
- Liv Hospital offers patient-centered care for international patients.
- Understanding risk factors is essential for heart health.
- Knowing the 7 key signs can save lives.
Understanding Arteriosclerosis Cardiovascular Disease

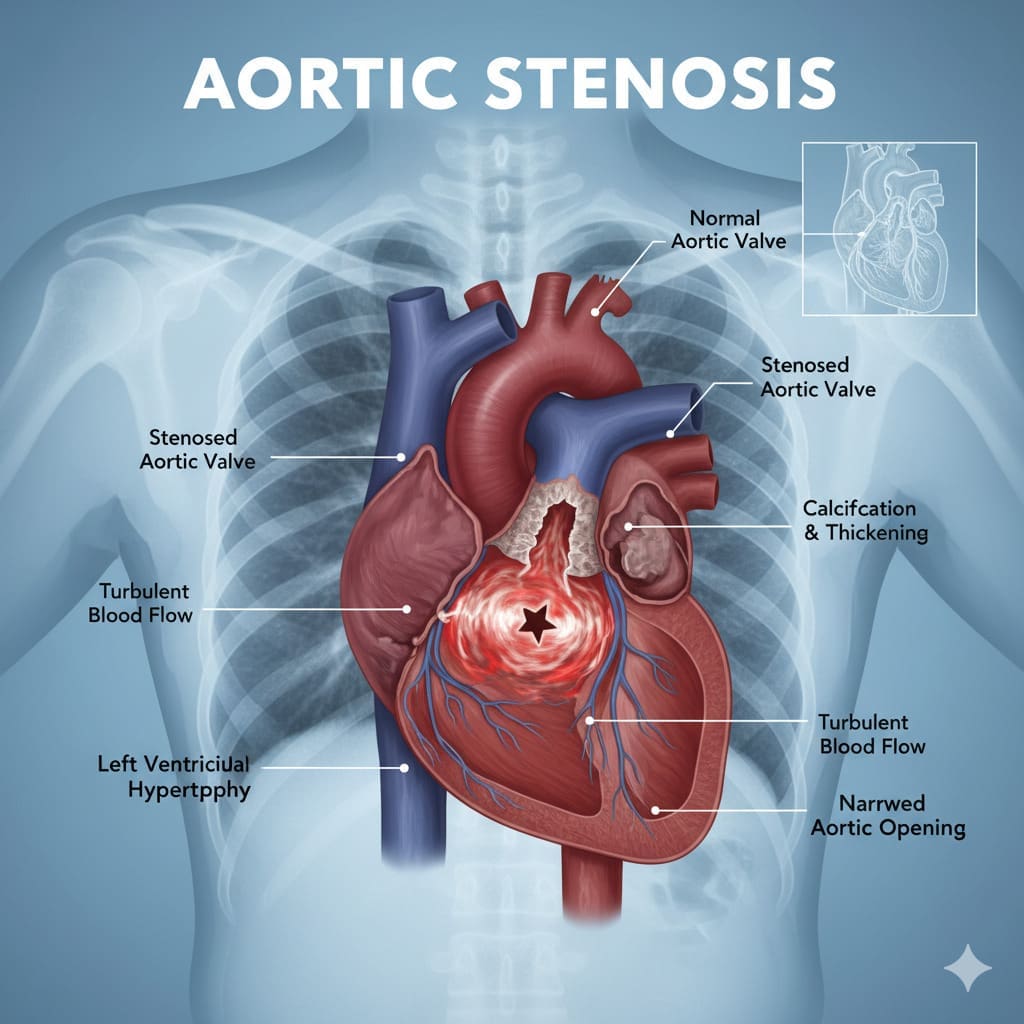
Arteriosclerosis is a condition where arteries become thick and stiff. It’s a major cause of heart disease. High cholesterol and blood pressure often lead to this problem.
What Is Arteriosclerosis?
Arteriosclerosis means arteries get hard and narrow because of plaque buildup. This plaque is made of fat, cholesterol, and other stuff. It blocks blood flow to important organs like the heart and brain.
How Arteriosclerosis Affects Your Cardiovascular System
The heart needs flexible arteries to work well. Arteriosclerosis makes arteries stiff and narrow. This reduces blood flow and raises the risk of heart attacks and strokes.
- Hardening and narrowing the arteries
- Reducing blood flow to vital organs
- Increasing the risk of heart attacks, strokes, and other cardiovascular events
As arteriosclerosis gets worse, it can cause many heart problems. These include coronary artery disease and peripheral artery disease.
The Global Impact of Arteriosclerotic Heart Disease
Arteriosclerotic heart disease is a big problem worldwide. It leads to a lot of sickness and death. The World Health Organization says it’s the top cause of death globally.
| Region | Cardiovascular Disease Mortality Rate |
| Global | 17.9 million deaths per year |
| North America | 1.8 million deaths per year |
| Europe | 2.2 million deaths per year |
Knowing how big a problem arteriosclerotic heart disease is shows why we need to act. We must change our lifestyles and use medicine to fight heart disease.
The Silent Progression: Why Early Detection Matters

Early detection of arteriosclerosis is key because it can be silent until it’s too late. At Liv Hospital, we stress the need to catch arteriosclerosis early to avoid heart problems.
The Asymptomatic Nature of Early Arteriosclerosis
Arteriosclerosis often starts without symptoms. This makes it hard for people to know they have it until it’s advanced.
Key factors contributing to the asymptomatic nature include:
- Lack of visible symptoms
- Gradual progression of the disease
- Limited awareness of risk factors
Complications When Left Undetected
If arteriosclerosis is not caught, it can cause serious heart issues. This includes heart attacks and strokes. Early detection is critical to avoid these risks.
| Complication | Description | Risk Factors |
| Heart Attack | Occurs when the blood flow to the heart is blocked | High blood pressure, high cholesterol, smoking |
| Stroke | Occurs when the blood supply to the brain is interrupted | High blood pressure, diabetes, atrial fibrillation |
Risk Assessment Importance
Checking for risk factors is essential for catching arteriosclerosis early. At Liv Hospital, we use top-notch tests to spot risks and create prevention plans for each person.
Common risk factors for arteriosclerosis include:
- Family history of heart disease
- High blood pressure
- High cholesterol levels
- Smoking and tobacco use
- Diabetes
Arteriosclerosis Cardiovascular Disease Symptoms: The 7 Warning Signs
Arteriosclerosis can show different symptoms, but there are seven main signs to look out for. This condition makes arteries narrow and hard due to plaque, affecting blood flow. It can lead to serious heart problems.
How Symptoms Develop in Arteriosclerosis
Symptoms appear when blood flow to the body decreases. As arteriosclerosis worsens, arteries get stiffer and narrower. This limits oxygen and nutrients to tissues and organs.
Key factors influencing symptom development include:
- The rate of plaque buildup
- The location of affected arteries
- The overall health of the individual
Symptom Variations by Affected Artery
Symptoms change based on which arteries are affected. For example, chest pain or angina can happen when coronary arteries are involved. On the other hand, leg pain or cramping during walking can occur with peripheral artery disease.
| Affected Artery | Common Symptoms |
| Coronary Arteries | Chest pain (angina), shortness of breath |
| Carotid Arteries | Dizziness, numbness, cognitive changes |
| Peripheral Arteries | Leg pain, cramping during walking (claudication) |
The Importance of Recognizing Early Signs
Spotting arteriosclerosis symptoms early is key for timely treatment. Early detection helps make lifestyle changes and treatments. These can slow disease progress and lower risks of heart attack or stroke.
Early recognition can lead to:
- Improved management of cardiovascular risk factors
- Enhanced quality of life through appropriate treatment
- Reduced risk of severe cardiovascular events
Knowing and spotting the seven warning signs of arteriosclerosis can help keep your heart healthy. It encourages a healthier lifestyle.
Warning Sign 1: Chest Pain and Discomfort
Chest pain is a serious warning sign that should not be ignored. It can be a sign of arteriosclerosis cardiovascular disease. We will look at chest pain related to arteriosclerosis, its patterns, and when it’s an emergency.
Recognizing Angina and Its Patterns
Angina is chest pain caused by reduced blood flow to the heart. It feels like a squeezing or pressure in the chest. It’s important to recognize angina patterns to understand its link to arteriosclerosis. Angina can be triggered by physical activity or stress and usually goes away with rest.
- Stable angina follows a predictable pattern and is often triggered by exertion.
- Unstable angina is more unpredictable and can occur at rest.
Knowing these patterns helps in diagnosing and managing angina effectively.
Differentiating Cardiac Chest Pain from Other Types
Not all chest pain is from heart conditions. Differentiating cardiac chest pain from other types is essential for proper diagnosis and treatment. Cardiac chest pain feels like pressure or squeezing in the chest. Other types might be sharp or stabbing.
| Characteristics | Cardiac Chest Pain | Non-Cardiac Chest Pain |
| Sensation | Pressure, squeezing | Sharp, stabbing |
| Triggers | Exertion, stress | Movement, deep breathing |
When Chest Pain Requires Emergency Attention
Chest pain can sometimes mean a heart attack, which is a medical emergency. If you have severe, prolonged chest pain, or other symptoms like shortness of breath, dizziness, or nausea, seek emergency care immediately.
Quick medical attention can greatly improve outcomes in heart attack or other serious conditions.
Warning Signs 2 & 3: Shortness of Breath and Fatigue
Arteriosclerosis can cause reduced blood flow. This shows up as shortness of breath and fatigue. These signs are important to notice and can mean heart problems.
Breathing Difficulties During Activity vs. Rest
Shortness of breath, or dyspnea, happens when the heart can’t pump enough blood. This is common in arteriosclerosis, where arteries narrow or harden. At first, it might only happen when you’re active. But as it gets worse, it can happen even when you’re resting.
A study in BMC Emergency Medicine shows how important it is to understand dyspnea. It helps doctors diagnose and treat heart diseases.
- Activity-induced dyspnea: Often an early sign of cardiovascular compromise.
- Dyspnea at rest: Indicates more severe cardiac dysfunction.
Understanding Cardiovascular Fatigue
Fatigue is a common symptom of arteriosclerosis. It happens when the heart can’t pump blood well. This leads to less oxygen for tissues and organs, making you feel tired all the time.
Cardiovascular fatigue is different from other kinds of fatigue. It’s linked to heart problems and doesn’t go away with rest.
Several factors contribute to cardiovascular fatigue:
- Reduced cardiac output due to arteriosclerotic changes.
- Increased energy expenditure by the heart to maintain circulation.
- Potential comorbid conditions such as anemia or thyroid disorders.
How Reduced Blood Flow Affects Energy Levels
Reduced blood flow affects energy levels a lot. When arteries narrow or harden, tissues and organs get less oxygen and nutrients. This means less energy at the cellular level. You might feel tired all the time, affecting your daily life.
Managing cardiovascular health means spotting these symptoms early. Understanding arteriosclerosis, shortness of breath, and fatigue helps. It’s key to keeping your heart healthy.
Warning Signs 4 & 5: Muscle Weakness and Numbness
Muscle weakness and numbness are important signs that might mean you have peripheral artery disease. This is a sign of arteriosclerosis. These symptoms happen because your muscles and nerves don’t get enough blood, usually in your limbs.
Patterns of Weakness in Peripheral Artery Disease
Peripheral artery disease (PAD) happens when your peripheral arteries narrow or block. This mainly affects your legs. It makes your muscles weak, mostly when you’re active, because they don’t get enough oxygen and nutrients.
For example, if the femoral artery narrows, you might feel weak in your calf muscles. This makes walking or climbing stairs hard. Knowing these patterns helps doctors diagnose PAD early.
Numbness and Tingling as Circulation Warning Signs
Numbness and tingling are big signs of poor circulation due to arteriosclerosis. These happen when nerves don’t get enough blood, making them work poorly. Numbness feels like you can’t feel anything, and tingling feels like pins and needles.
These feelings can come and go or stay all the time. If not treated, they can get worse. Sometimes, you might also feel pain, making things even harder.
“The presence of numbness and tingling in the context of peripheral artery disease should prompt further investigation into the underlying cause and appropriate management strategies.” -A vascular specialist
Distinguishing Vascular Symptoms from Other Conditions
It’s important to tell if muscle weakness and numbness come from vascular diseases or other problems. Other conditions like neurological disorders, musculoskeletal issues, and metabolic diseases can also cause these symptoms.
Getting a full medical check-up is key. This includes talking about your health and doing tests like the ankle-brachial index (ABI) or imaging studies. Living a healthy heart lifestyle helps a lot. This means exercising regularly, eating well, and quitting smoking.
Preventing and catching problems early is the best way to deal with arteriosclerosis. By knowing the warning signs and taking steps to prevent arteriosclerosis, you can greatly improve your heart health.
Warning Signs 6 & 7: Difficulty Walking and Cognitive Changes
Arteriosclerosis can make it hard to move and think clearly. As it gets worse, it can affect different parts of the body. This leads to various symptoms.
Claudication and Mobility Challenges
Walking problems, like claudication, are a big warning sign. Claudication happens when blood flow to the legs is cut off during exercise. This causes pain, cramps, or tiredness in the legs, making it hard to walk or do physical activities.
Claudication is more than just leg pain. It shows that the blood vessels are getting worse. To fix it, we need to treat the cause, like narrowing or blockage of arteries. This can be done through lifestyle changes, medicine, or surgery.
| Symptom | Cause | Impact |
| Leg Pain during walking | Reduced blood flow to leg muscles | Limited mobility |
| Cramping | Narrowing or blockage of arteries | Reduced quality of life |
| Fatigue | Insufficient oxygen supply | Decreased physical activity |
Carotid Artery Disease and Brain Function
When arteriosclerosis hits the carotid arteries, it can mess with the brain. This can lead to memory problems, cognitive issues, and a higher stroke risk.
It’s important to understand how carotid artery disease affects the brain. We can manage it with lifestyle changes, medicine, and sometimes surgery like carotid endarterectomy.
Cognitive Impairment and Vascular Dementia Risk
Arteriosclerosis can cause brain problems that might turn into vascular dementia. Vascular dementia makes it hard to think, remember, and solve problems.
We need to know the risks and take steps to avoid them. This includes keeping blood pressure in check, managing diabetes, quitting smoking, and eating well. By doing these things, we can lower the chance of getting vascular dementia.
Spotting arteriosclerosis early and treating it is key to avoiding brain and mobility problems. By catching the signs early and acting fast, we can improve our lives and lower the risk of serious health issues.
Prevention and Management of Arteriosclerosis
Managing arteriosclerosis requires lifestyle changes and medical care. At Liv Hospital, we focus on a full approach. We use the newest treatments and care methods.
Lifestyle Modifications for Arterial Health
Making lifestyle changes is key to preventing arteriosclerosis. Regular physical activity boosts heart health by improving blood flow and lowering blood pressure. We suggest at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly.
Dietary habits are also important. Eating more fruits, vegetables, whole grains, and lean proteins can lower arteriosclerosis risk. It’s important to eat less saturated fats, trans fats, and cholesterol.
Dietary Approaches to Reduce Arteriosclerosis Risk
Eating a heart-healthy diet is essential to lower arteriosclerosis risk. Include foods rich in omega-3 fatty acids like salmon and walnuts. Also, increase fiber with whole grains and legumes.
- Choose healthy fats, such as those found in olive oil and avocados.
- Limit sodium intake to less than 2,300 milligrams per day.
- Drink alcohol in moderation, if at all.
Medical Management and Monitoring
Medical care is a big part of preventing and treating arteriosclerosis. This may include medicines for blood pressure, cholesterol, and blood sugar.
At Liv Hospital, we use advanced tools to check heart health and adjust treatments. Regular check-ups and screenings help catch arteriosclerosis early.
Combining lifestyle changes with medical care can greatly lower arteriosclerosis risk and its complications.
Conclusion: Taking Action for Long-term Cardiovascular Health
Keeping your heart healthy is key to feeling good overall. Knowing the 7 signs of arteriosclerosis can help you prevent heart problems. Catching and treating arteriosclerosis early can lower your heart disease risk.
Living a healthy lifestyle is important for your heart. This includes exercising regularly, eating well, and not smoking. A balanced diet and staying active can greatly improve cardiovascular health. Managing heart issues also means making lifestyle changes and following doctor’s advice.
Choosing wisely and getting medical help when needed can lower your heart disease risk. We urge everyone to take charge of their heart health. Making healthy choices can help keep your heart strong for the long term.
FAQ
What is arteriosclerosis cardiovascular disease?
Arteriosclerosis is a condition where arteries harden and narrow. This reduces blood flow to vital organs. It increases the risk of heart attacks and strokes.
What are the early symptoms of arteriosclerosis?
Early arteriosclerosis often doesn’t show symptoms. But as it gets worse, symptoms like chest pain and shortness of breath appear. Other signs include fatigue, muscle weakness, and numbness.
How does arteriosclerosis affect the cardiovascular system?
Arteriosclerosis hardens and narrows arteries. This reduces blood flow to vital organs. It also raises the risk of heart attacks and strokes.
What is the importance of early detection in arteriosclerosis?
Finding arteriosclerosis early is key. It helps prevent heart attacks and strokes. It also helps manage heart health through early medical action.
How can I reduce my risk of developing arteriosclerosis?
A healthy lifestyle can lower arteriosclerosis risk. Eat well, exercise regularly, and manage risk factors.
What are the treatment options for arteriosclerosis?
Treatments include lifestyle changes and medical management. Advanced tests and treatments are available at places like Liv Hospital.
Can arteriosclerosis be managed and treated?
Yes, arteriosclerosis can be managed. This is done through lifestyle changes, medical care, and monitoring. It improves heart health and lowers complication risks.
What is the link between reduced blood flow and symptoms like fatigue and shortness of breath?
Reduced blood flow causes fatigue and shortness of breath. This is because vital organs don’t get enough oxygen and nutrients.
How does peripheral artery disease relate to arteriosclerosis?
Peripheral artery disease is a form of arteriosclerosis. It affects arteries in the legs, causing muscle weakness, numbness, and walking problems.
What is the role of diet in preventing and managing arteriosclerosis?
A balanced diet is key. It should include fruits, vegetables, whole grains, and lean proteins. It helps prevent arteriosclerosis and manage its progression by controlling risk factors.