Getting a correct diagnosis is key for good treatment, more so for diseases like arthritis. Studies show that using an arthritis confirming scan can lead to a more precise diagnosis, which in turn greatly improves treatment results.
Arthritis diagnosis uses many imaging methods to check for and identify arthritis types. Each scan is important for making treatment plans. In this article, we’ll look at the scans used for arthritis diagnosis and why they matter.
Diagnostic imaging is key in diagnosing and managing arthritis. It helps doctors see joint damage and inflammation. We use different imaging methods to accurately diagnose and treat this complex condition.
Arthritis includes over 100 conditions that affect joints and tissues. The main types are osteoarthritis (OA), rheumatoid arthritis (RA), and psoriatic arthritis (PsA). Each type needs its own diagnostic approach.
Osteoarthritis causes cartilage breakdown, leading to bone-on-bone contact and pain. Rheumatoid arthritis is an autoimmune disease that causes inflammation and can damage joints severely. Psoriatic arthritis is linked to psoriasis and causes joint inflammation and damage.
| Type of Arthritis | Primary Characteristics | Common Imaging Findings |
| Osteoarthritis (OA) | Cartilage degradation, joint space narrowing | Joint space narrowing, osteophytes, subchondral sclerosis |
| Rheumatoid Arthritis (RA) | Synovial inflammation, autoimmune | Synovitis, erosions, uniform joint space narrowing |
| Psoriatic Arthritis(PsA) | Inflammatory arthritis associated with psoriasis | Joint erosions, new bone formation, enthesitis |
Advanced imaging is needed for accurate arthritis diagnosis. Techniques like MRI and ultrasound show early joint and soft tissue changes. These are key for diagnosing inflammatory arthritis.
Advanced imaging helps not just in diagnosis but also in tracking disease activity and treatment response. For example, MRI can measure synovitis and bone marrow edema, showing disease severity.
Using these advanced imaging methods, we can start treatment early. This improves patient outcomes.
X-rays are a key tool for diagnosing arthritis. They show us how healthy joints are. We use X-rays first because they show important joint damage.
X-rays are great for showing bone and joint space changes. They help spot joint space narrowing and bone changes like erosions. This helps us understand how much damage there is.
Getting an X-ray is easy. X-rays use radiation to take pictures of joints. These pictures let us see if there’s arthritis and how bad it is.

Arthritis types show different things on X-rays. Osteoarthritis shows joint space narrowing and bone growth. Rheumatoid arthritis shows joint narrowing and bone loss.
| Arthritis Type | Characteristic X-Ray Findings |
| Osteoarthritis | Joint space narrowing, subchondral sclerosis, osteophytes |
| Rheumatoid Arthritis | Symmetric joint space narrowing, marginal erosions, periarticular osteopenia |
| Psoriatic Arthritis | Asymmetric joint involvement, erosions, fluffy periostitis |
X-rays are useful but have limits. They don’t catch early soft tissue changes. They also miss early bone and cartilage damage. So, we use other tests too.
Even with their limits, X-rays are key for diagnosing and tracking arthritis. Knowing their strengths and weaknesses helps us use them well in diagnosis.
Choosing the right tool to confirm arthritis is key. It helps in creating effective treatment plans. The choice depends on the symptoms, type of arthritis, and what needs to be seen. We’ll look at how different imaging methods work together for a full diagnosis.
The symptoms a patient shows guide the best imaging choice. For example, those with inflammatory arthritis might need Magnetic Resonance Imaging (MRI) or Ultrasound to see soft tissue changes. Those with osteoarthritis might need X-Rays or Computed Tomography (CT) scans to see bone and joint changes.
We look at the symptoms and findings to pick the right imaging. For instance, if a patient has joint pain and swelling, we might choose an imaging that spots early inflammation.
Each imaging method has its own strengths and weaknesses. MRI is great for catching early signs of inflammation. CT scans are better for seeing bone damage. Knowing these helps us make accurate diagnoses.
It’s important to understand how sensitive and specific each method is. This helps us confirm arthritis and rule out other causes.
No single method can show everything about arthritis. Instead, they work together to give a full picture. For example, X-Rays can show initial damage, but MRI or Ultrasound can show soft tissue details.
Using multiple methods helps us understand the disease better. This way, we can create a treatment plan that fits the patient’s needs.
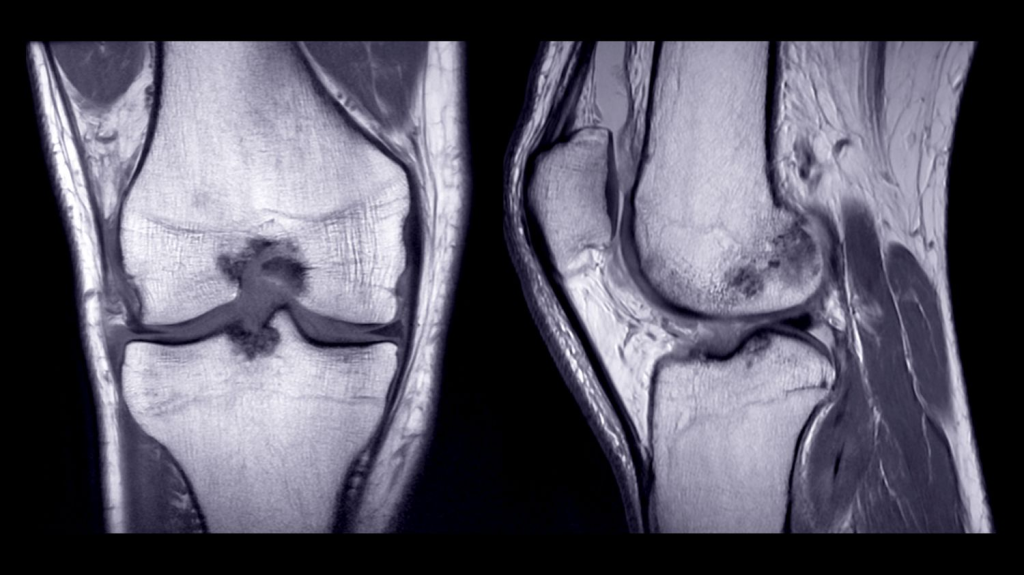
MRI has changed how we diagnose arthritis. It lets doctors see soft tissue problems clearly. This makes MRI key for checking inflammatory arthritis.
MRI spots early signs of arthritis well. It finds synovitis, joint effusion, and bone marrow edema early. These signs can lead to serious damage if not treated soon.
Using contrast agents in MRI makes inflammation easier to see. It highlights synovial enhancement, a sign of active inflammation. This helps doctors understand how active the disease is and how far it has spread.
There are MRI scoring systems to measure arthritis severity. The RAMRIS (Rheumatoid Arthritis Magnetic Resonance Imaging Scoring System) is one. It measures inflammation and damage, helping doctors decide on treatment.
Using MRI and its advanced methods helps us better diagnose and manage arthritis. It lets us tailor treatments to each patient, possibly changing the disease’s course.
Ultrasound technology has changed how we check for joint inflammation in arthritis patients. It lets us see what’s happening in joints in real time.
Ultrasound is great for finding active inflammation in arthritis. It uses Power Doppler to show blood flow changes. This helps us understand how active the disease is.
Power Doppler ultrasound helps us see how severe the inflammation is. It also shows how well treatments are working. It catches even small changes in blood flow, helping us track the disease’s progress.
Ultrasound is also good for guiding joint injections and other procedures. It makes these treatments more accurate. This can lead to better results for patients.
With ultrasound, we can place needles and medications exactly right. This lowers the chance of problems and makes treatments work better.
Ultrasound is easy to move around and is not very expensive. This makes it a good choice for diagnosing and managing arthritis. It’s cheaper than some other imaging methods and can be taken to different places.
A medical expert said, “Ultrasound is key in managing arthritis because it’s easy to use and shows what’s happening in real time.” Many studies support using ultrasound in rheumatology too.
“The use of ultrasound in rheumatology has transformed our ability to diagnose and manage arthritis, giving us a detailed look at joint inflammation.”
We keep using ultrasound to help our patients. We mix its benefits with other tools to get the best results.
Computed Tomography (CT) scans are key for checking complex joints. They give us detailed views of bones and joints. This is vital for spotting and treating arthritis.
CT scans show detailed bone architecture. This is key for seeing how much damage arthritis has caused. They show small changes in bones, helping us figure out the type and how bad the arthritis is.
Seeing bones in detail helps doctors track arthritis and plan treatments. It’s very helpful for joints that are hard to see with other methods.
CT arthrography uses contrast to see cartilage and soft tissues better. It’s great for spotting cartilage damage that’s hard to see on other scans.
This method helps us understand how much cartilage is lost and soft tissue injuries. It’s key for making a good treatment plan. It’s very useful for finding cartilage problems or injuries.
CT scans are also great for the spine and pelvis. These areas need detailed scans to diagnose and treat conditions like ankylosing spondylitis.
| Region | Common Arthritis Types | CT Scan Benefits |
| Spine | Ankylosing Spondylitis, Spondylitis | Detailed visualization of bone fusion and syndesmophytes |
| Pelvis | Sacroiliitis, Osteoarthritis | Assessment of sacroiliac joint inflammation and damage |
CT scans help us understand the extent of disease in the spine and pelvis. They let us see how well treatments are working. This is very important for managing these complex conditions.
Nuclear medicine bone scans are key in finding active inflammation in arthritis. They help spot areas where bone activity is up, showing signs of inflammatory arthritis.
We inject a small amount of technetium-99m (Tc-99m) into the patient’s blood. This radiopharmaceutical goes to areas with high bone turnover, like arthritis spots. Then, a gamma camera takes images of the skeleton, showing where Tc-99m is most.
Key Steps in Technetium-99m Bone Scintigraphy:
Nuclear medicine bone scans can look at the whole skeleton at once. This is great for diagnosing and managing systemic arthritis, like rheumatoid arthritis.
Experts say, “Bone scintigraphy is good at spotting early bone changes, even before regular X-rays can.”
This whole-body assessment helps us see how much disease is present and how well treatment is working.
Bone scans can tell arthritis apart from other bone issues by showing specific activity patterns. For example, osteoarthritis shows up in certain spots, while rheumatoid arthritis is more spread out and symmetrical.
| Condition | Typical Bone Scan Pattern |
| Osteoarthritis | Localized areas of increased uptake |
| Rheumatoid Arthritis | Symmetrical and widespread uptake |
| Paget’s Disease | Intense, localized uptake |
By looking at Tc-99m uptake patterns, we can understand what’s happening in the bones and joints. This info is key for making the right treatment plan.
Advanced nuclear imaging has greatly improved arthritis diagnosis. These new methods give detailed views and functional info about the disease. This helps doctors diagnose and manage arthritis more accurately. We’ll look at SPECT and PET scans, and how they work together, in arthritis assessment.
SPECT scans are a big step forward in nuclear medicine. They show the body’s metabolic processes in 3D. For arthritis, SPECT scans spot inflammation and bone changes. This is great for seeing complex joints and catching early disease signs.
These 3D images help doctors understand arthritis better. They’re key for making treatment plans and tracking the disease’s progress.
PET imaging is a powerful tool for arthritis. It uses special radiotracers to show metabolic activity in joints. For example, FDG PET scans find high glucose uptake, which means inflammation.
PET scans can spot inflammation early, even before structural changes show up. This early detection is vital for starting treatment quickly and preventing joint damage.
Hybrid imaging, like PET-CT and SPECT-CT, combines nuclear medicine with CT scans. This mix offers big benefits for arthritis assessment.
| Hybrid Imaging Modality | Benefits in Arthritis Assessment |
| PET-CT | Combines metabolic activity info with precise anatomy, making it easier to find inflammation and structural changes. |
| SPECT-CT | Shows detailed 3D metabolic processes in complex joints, helping assess disease extent and severity. |
Hybrid imaging has greatly improved arthritis diagnosis and treatment. It gives a full picture of the disease, helping doctors create better treatment plans.
DEXA scans have greatly improved how we manage arthritis. DEXA, or Dual-Energy X-ray Absorptiometry, is a key tool for checking bone health in arthritis patients.
We use DEXA scans to measure bone mineral density. This is vital for knowing the bone health of patients with inflammatory arthritis. It helps us create treatment plans that focus on bone health.
Inflammatory arthritis, like rheumatoid arthritis, can lower bone mineral density. This raises the risk of osteoporosis and fractures. DEXA scans help us spot bone loss early and manage it.
Key benefits of DEXA scans in assessing BMD include:
Experts say early action in inflammatory arthritis can greatly improve outcomes. It helps avoid bone-related problems.
“The use of DEXA scans has revolutionized the way we manage arthritis by providing a clear picture of bone health.”
Glucocorticoids are used to treat inflammatory arthritis. But long-term use can cause osteoporosis. DEXA scans help us see how glucocorticoid therapy affects bone density.
Regular monitoring with DEXA scans allows for:
By adding DEXA scans to the management plan, we offer full care. It tackles both arthritis and bone-related issues.
Arthritis is not just one disease; it has many forms. Each type needs its own imaging plan. Doctors must pick the best imaging tools for each case.
Osteoarthritis (OA) causes cartilage to break down and bones to change. Imaging is key to see these changes. X-rays show joint narrowing and bone growths.
Magnetic Resonance Imaging (MRI) is better for soft tissues. It shows cartilage loss and bone issues, giving a full view of the joint.
Ultrasound also helps with OA, looking at inflammation and fluid in the joint. The right imaging tool depends on the disease’s stage and what the doctor needs to see.
Rheumatoid arthritis (RA) is an autoimmune disease that harms joints. Finding it early and tracking its activity are key to managing it. Ultrasound and MRI spot early signs of inflammation and damage.
Power Doppler ultrasound is great for seeing active inflammation. MRI gives detailed views of bones and soft tissues. It helps see how much disease is present and how well treatments are working.
Psoriatic arthritis (PsA) and gout need special imaging plans. For PsA, MRI and ultrasound check for enthesitis. In gout, imaging finds crystal deposits and damage.
Dual-energy CT is best for finding urate crystals in gout. The right imaging tool for other conditions depends on the disease and the joints affected. We look at how well the imaging works and if it helps with treatment.
Diagnosing arthritis takes a detailed approach. We use clinical evaluation, lab results, and imaging to get a clear picture. This ensures patients get the right treatment.
When symptoms point to arthritis, we start with a detailed check-up. We look at the patient’s medical history and do a physical exam. This helps us figure out the type of arthritis and what tests to run next.
Key components of the initial clinical assessment include:
Labs are key in diagnosing arthritis. They check for inflammation and autoimmune markers. We match these lab results with imaging to confirm the diagnosis and see how severe it is.
Common laboratory tests used in arthritis diagnosis include:
Imaging like X-rays, ultrasound, MRI, and CT scans show joint damage and inflammation. By linking lab results with imaging, we get a precise diagnosis and create a tailored treatment plan.
While X-rays are first, we use advanced imaging for a closer look. We do this when the diagnosis is tricky, when joints are complex, or when checking how well treatment is working.
Advanced imaging modalities, such as MRI and CT scans, offer:
By combining clinical checks, lab tests, and imaging, we can accurately diagnose arthritis. This way, we offer personalized care to our patients.
Early detection of arthritis is key to managing the disease well. It allows for timely action and better results for patients. Finding arthritis early helps prevent lasting damage and improves patients’ lives.
Advanced imaging is vital in spotting early signs of arthritis. Tools like MRI and ultrasound can find inflammation and joint damage before symptoms show. This lets doctors start treatment early, which can stop the disease from getting worse.
MRI can see synovitis and bone marrow edema, signs of early arthritis. Finding these early means we can act before damage is permanent.
The therapeutic window of opportunity is the time between arthritis symptoms and permanent damage. Early action can change the disease’s path. Advanced imaging helps find patients in this window for timely treatment.
Research shows early treatment can lead to less joint damage and better function. So, using advanced imaging for early detection is key in managing arthritis.
Imaging helps not just in early detection but also in risk stratification. It lets doctors see how much damage and inflammation there is. This helps sort patients by risk of disease getting worse. It guides treatment, making sure high-risk patients get the most help.
We use imaging to make treatment plans that fit each patient’s needs. This approach improves outcomes and reduces unnecessary treatments.
Managing arthritis well means keeping a close eye on how the disease is doing and how treatments work. We use top-notch imaging to see how the disease is moving and if treatments are helping.
Standard scoring systems are key for checking how the disease is getting worse or better. They help us measure how bad the joint inflammation and damage are. For example, the Rheumatoid Arthritis Magnetic Resonance Imaging Scoring (RAMRIS) system is often used for rheumatoid arthritis.
| Scoring System | Application | Key Features |
| RAMRIS | Rheumatoid Arthritis | Assesses synovitis, bone edema, and erosions |
| OMERACT | Osteoarthritis | Evaluates cartilage loss and bone spurs |
| PsAMRIS | Psoriatic Arthritis | Measures synovitis, enthesitis, and bone proliferation |
Imaging biomarkers are vital for seeing if treatments are working. We use different imaging methods to check for changes in the disease and joint damage over time. For instance, contrast-enhanced MRI can show how much less inflammation there is after treatment.
Finding the best time for follow-up imaging is important for seeing how treatments are doing. We usually plan follow-ups at times when we can see meaningful changes in the disease. For many, this means imaging every 6 to 12 months, based on how severe their condition is and their treatment.
By watching disease activity and treatment response closely with advanced imaging, we can make smart choices about changing treatment plans. This helps us get the best results for our patients.
Imaging for arthritis is a delicate balance. We need to make sure it’s accurate and safe for patients. As we learn more about arthritis, keeping patients safe is key.
Radiation is a big concern in arthritis imaging. X-rays and CT scans use radiation, but MRI and ultrasound don’t. We must think about the risks and benefits of each.
“The risk of radiation-induced harm is a significant consideration, particular for younger patients and those requiring repeated imaging,” says a leading expert in rheumatology imaging. This is important because many arthritis patients are young and need ongoing care.
Contrast media is another safety issue. While safe for most, it can cause problems for some. We must watch for risks and take steps to prevent them. This includes checking kidney function and being ready for emergencies.
Imaging pregnant or pediatric patients requires extra care. For pregnant women, we try to avoid radiation and use ultrasound or MRI instead. For kids, we balance the need for images with the risks of radiation or sedation.
Key Considerations for Pregnant Patients:
Key Considerations for Pediatric Patients:
By focusing on safety, we can give our patients the imaging they need without risking their health. As we continue to improve in treating arthritis, keeping patients safe will always be our top priority.
Accurate diagnosis and monitoring of arthritis use many imaging methods. Each has its own strengths and weaknesses. New technology is making it easier to diagnose and manage arthritis better.
The future of arthritis diagnosis is bright. New imaging tech is getting better at finding arthritis early. This means we can manage the disease more effectively.
Using different imaging techniques together can improve patient care. As technology advances, it will be key in diagnosing and monitoring arthritis.
The best scan for arthritis depends on the type and symptoms. We use X-rays, MRI, ultrasound, CT scans, and nuclear medicine bone scans. Each helps in diagnosing and managing arthritis.
MRI is great for soft tissue evaluation. It helps spot synovitis, effusions, and bone marrow edema in inflammatory arthritis. Contrast-enhanced MRI shows inflammatory changes better.
Ultrasound is good for dynamic joint inflammation assessment. It detects active inflammation with power Doppler. It also guides joint injections and procedures.
Yes, CT scans are good for complex joint structures and bone architecture. CT arthrography is great for cartilage assessment. It’s useful in diagnosing arthritis, mainly in the axial skeleton.
Nuclear medicine bone scans use technetium-99m bone scintigraphy. They detect active inflammation and whole-body involvement in arthritis. They help differentiate arthritis from other bone disorders.
DEXA scans are key in assessing bone mineral density in inflammatory arthritis patients. They monitor the risk of osteoporosis from glucocorticoids. This is part of managing arthritis comprehensively.
Imaging modalities show distinct characteristics of each arthritis type. This helps guide treatment plans. It’s important for differentiating osteoarthritis, rheumatoid arthritis, and psoriatic arthritis.
Safety includes radiation exposure, contrast media reactions, and special considerations for pregnancy and children. These are important factors to consider.
Follow-up imaging timing varies based on arthritis type, activity, and treatment response. Standardized scoring and biomarkers help evaluate disease progression and treatment success.
Yes, advanced imaging can spot pre-clinical disease markers. This offers a chance for early intervention and preventing joint damage.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us