Last Updated on December 4, 2025 by Ugurkan Demir
Learn what atherosclerotic calcification is and why calcium buildup in arteries affects heart health.
At Liv Hospital, we know how vital a healthy heart is. We focus on atherosclerotic calcification. This is when calcium builds up in the walls of arteries with atherosclerosis.
This buildup is a big sign of coronary artery disease. Knowing about it early is very important. It helps us manage and maybe even reverse the disease.
We employ cutting-edge, evidence-based methods to spot and handle these changes. This helps you stay on top of your heart health.
Key Takeaways
- Atherosclerotic calcification is a condition where calcium builds up in the arterial walls.
- It’s a significant indicator of coronary artery disease.
- Early detection is key to heart health management.
- Advanced diagnostic approaches can help identify the condition.
- Managing atherosclerotic calcification is essential for a healthy heart.
The Nature of Atherosclerotic Calcification
To understand atherosclerotic calcification, we must first know what it is. It’s when calcium builds up in the walls of arteries. This buildup is linked to atherosclerosis, a serious heart disease.
Definition and Basic Concepts
Atherosclerotic calcification occurs when calcium phosphate builds up in the arteries. It’s not just calcium settling there. It’s an active process involving many cells and molecules.
This buildup means the arteries are getting thicker and harder. This can make them less flexible and increase heart disease risk.
How It Differs from Normal Calcium Metabolism
Normal calcium helps our bones and muscles. But in atherosclerotic calcification, calcium goes to the wrong place. It builds up in the arteries instead of the bones.
This wrong placement is due to injury, inflammation, and repair in the arteries. It’s like bone formation happening in the wrong place. Many cells and molecules are involved in this process.
Knowing how atherosclerotic calcification differs from normal calcium is key. It helps us understand the disease better. It also shows why we need specific treatments for it.
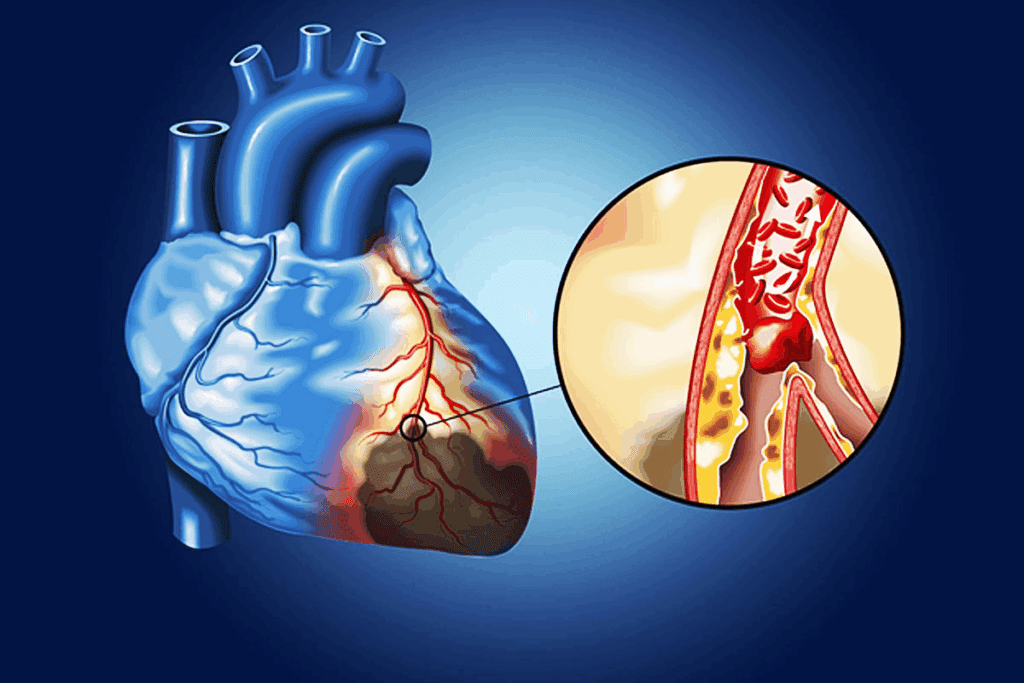
The Relationship Between Atherosclerosis and Calcification
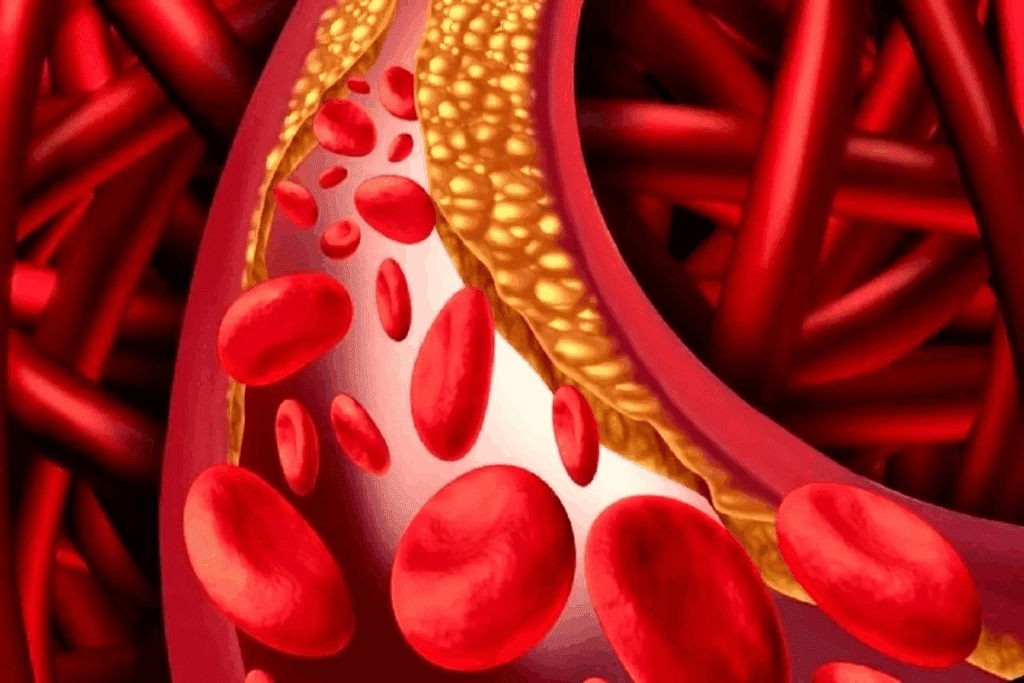
Atherosclerosis is when plaque builds up in the arteries over time. This buildup includes cholesterol and fatty substances. It narrows the arteries, reducing blood flow to important organs.
Plaque Formation and Progression
Plaque forms when lipids get into the arterial wall and cause inflammation. This attracts immune cells. Over time, the plaque grows and can become unstable.
Plaque progression is affected by hypertension, hyperlipidemia, and smoking. As it grows, it narrows the arteries, reducing blood flow.
When and Why Calcium Enters the Picture
Calcium deposits form in the plaque, making it more stable but rigid. This process is like bone formation. It’s influenced by osteogenic cells and calcium and phosphate levels.
Calcium in plaque is a key step in atherosclerotic calcification. It affects the plaque’s stability and the artery’s health.
Understanding Atherosclerotic Calcification as an Active Process
Atherosclerotic calcification is not just a passive event. It’s an active process with complex biological mechanisms. These mechanisms are similar to bone formation. This knowledge is key to understanding its impact on artery health.
The Biology of Arterial Calcification
Arterial calcification involves many cellular and molecular steps. Specific cells in the artery wall, like vascular smooth muscle cells, turn into bone cells. This leads to the buildup of calcium and phosphate minerals. It’s all about the balance of promoters and inhibitors, similar to bone mineralization.
For example, bone morphogenetic proteins (BMPs) and runt-related transcription factor 2 (Runx2) are important. They play roles in both bone formation and artery calcification. How these factors are regulated is key to preventing calcification.
Parallels to Bone Formation
Atherosclerotic calcification is similar to bone formation. Both involve the formation of hydroxyapatite crystals, a type of calcium phosphate. The cells and pathways involved in bone formation are also found in arterial calcification.
Grasping these similarities is vital for finding treatments. By studying bone biology, researchers can find ways to stop or reverse artery calcification.
Why Atherosclerotic Calcification Matters for Heart Health
Atherosclerotic calcification is key to heart health. Calcium in artery plaques shows how severe atherosclerosis is. It also affects how well arteries work.
Impact on Arterial Function
Calcified arteries become stiffer. This makes it hard for arteries to expand and contract. The heart must work harder to pump blood, leading to hypertension and more strain on the heart.
Relationship to Blood Flow Restriction
More calcification means narrower arteries. This limits blood flow to important organs. Symptoms like chest pain (angina) and shortness of breath can occur.
Implications for Cardiovascular Events
Calcification levels predict future heart problems. People with higher calcium scores face higher risks of heart attacks and strokes. So, it’s vital to manage and watch calcification to prevent these issues.
Detecting and Measuring Atherosclerotic Calcification
Imaging is key in finding and measuring atherosclerotic calcification. New imaging methods have changed the game. They help doctors diagnose and track calcification more accurately.
Imaging Techniques
Many imaging methods help spot and measure atherosclerotic calcification. Noncontrast, electrocardiographic (ECG)-gated cardiac electron beam computed tomography (EBCT) or multislice detector computed tomography (MDCT) are common. These technologies give clear pictures of the coronary arteries, showing calcium deposits.
Computed Tomography (CT) scans are great at showing calcification because they’re very sensitive to calcium. The Agatston score, from CT scans, is a key measure of coronary artery calcification. It helps doctors understand how severe the calcification is and the risk of heart disease.
- EBCT and MDCT: These CT scans give detailed images of the heart and its vessels, important for finding calcification.
- Agatston Score: A number that shows how much calcium is in the coronary arteries, helping to figure out risk.
Interpreting Calcification Findings
Understanding imaging results is important for dealing with atherosclerotic calcification. The amount and presence of calcification show how severe atherosclerosis is and the risk of heart problems.
A higher Agatston score means more calcification and a higher risk of heart events. Doctors use this info to plan the best prevention and treatment plans for each patient.
- A low Agatston score (1-100) means little atherosclerosis and lower heart risk.
- A moderate score (101-400) shows a moderate risk, needing lifestyle changes and possibly medicine.
- A high score (>400) means a lot of calcification and a big risk of heart problems, needing strong risk management.
By accurately finding and understanding atherosclerotic calcification, doctors can manage heart risk better and improve patient results.
Risk Factors for Developing Arterial Calcification
It’s important to know the risk factors for arterial calcification to prevent and manage it. This condition is influenced by many factors. These can be divided into non-modifiable and modifiable risk factors.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Advanced age: The risk of arterial calcification increases with age.
- Male gender: Men are generally at higher risk than women.
- Genetic predisposition: Family history can play a significant role.
A study found that “the presence of calcification in the coronary arteries is a marker of atherosclerotic plaque burden and is associated with increased risk of cardiovascular events.” This shows why knowing non-modifiable risk factors is key.
Modifiable Risk Factors
Modifiable risk factors, by contrast, can be changed through lifestyle or medical interventions. These include:
| Risk Factor | Description |
| Diabetes | Increases the risk due to associated metabolic dysregulation. |
| Hypertension | High blood pressure can accelerate arterial calcification. |
| Dyslipidemia | Abnormal levels of lipids in the blood contribute to calcification. |
| Cigarette smoking | Smoking is a significant risk factor due to its impact on vascular health. |
| Hyperphosphatemia | Elevated phosphate levels can contribute to calcification. |
Controlling these modifiable risk factors is key to preventing arterial calcification. A clinical guideline stresses, “lifestyle modifications and control of risk factors are essential for the prevention of cardiovascular disease.”
By tackling both non-modifiable and modifiable risk factors, we can create effective prevention and management strategies for arterial calcification.
Prevention Strategies for Atherosclerotic Calcification
To prevent atherosclerotic calcification, we need a complete plan. This includes eating right, exercising, and managing health issues. By doing this, we can lower the risk of getting calcified atherosclerotic plaques.
Dietary Approaches
Eating well is key to stopping atherosclerotic calcification. Foods like fruits, vegetables, and whole grains are good. Avoid too much saturated fat, cholesterol, and sodium.
Some foods are better than others for preventing atherosclerotic calcification. These include:
- Omega-3 fatty acids: In fatty fish, they fight inflammation.
- Antioxidants: In berries and leafy greens, they fight oxidative stress.
- Fiber: In whole grains and legumes, it lowers cholesterol.
Physical Activity Recommendations
Exercise is vital for stopping atherosclerotic calcification. It boosts heart health, lowers blood pressure, and keeps weight in check.
We suggest 150 minutes of moderate exercise, 75 minutes of vigorous exercise, or a mix of both each week.
| Activity Type | Intensity | Frequency |
| Aerobic Exercise | Moderate | At least 150 minutes/week |
| Aerobic Exercise | Vigorous | At least 75 minutes/week |
| Resistance Training | Moderate to High | 2-3 times/week |
Managing Underlying Conditions
It’s important to manage health issues to prevent atherosclerotic calcification. This means controlling blood pressure, diabetes, and cholesterol. Use lifestyle changes and medicine if needed.
Keeping these conditions in check can greatly lower the risk of heart problems linked to atherosclerotic calcification.
By eating well, exercising regularly, and managing health, we can stop or slow atherosclerotic calcification.
Treatment Options for Existing Calcification
Dealing with existing calcification requires a detailed plan. This plan includes both medicine and more direct treatments. We will look at the ways to handle atherosclerotic calcification.
Pharmaceutical Interventions
Medicine is key in fighting atherosclerotic calcification. Statins help lower cholesterol and slow down calcification. Antihypertensive medications also help by controlling blood pressure.
Other drugs, like bisphosphonates and denosumab, are being studied for their effects on calcification. But their success is not yet confirmed.
Surgical and Interventional Procedures
For severe cases, surgery or direct treatments are needed. Percutaneous coronary intervention (PCI) with stents is often used to open blocked arteries.
In some cases, coronary artery bypass grafting (CABG) is suggested. The choice depends on the calcification’s extent, location, and the patient’s health.
We will keep an eye on new treatments for atherosclerotic calcification. Our goal is to give the best care to those affected.
Conclusion
Understanding atherosclerotic calcification is key to keeping your heart healthy. This condition raises the risk of heart problems. Knowing about it helps us see why we need to prevent and manage it.
To prevent it, we need to eat right, exercise often, and handle health issues. If you already have it, there are treatments like medicines and surgery. Taking action early can lower your heart disease risk.
Atherosclerotic calcification is a serious issue that needs focus and care. By learning about it and taking steps to prevent it, we can greatly improve our heart health.
FAQ
What is atherosclerotic calcification?
Atherosclerotic calcification is when calcium builds up in the artery walls. It’s linked to atherosclerosis, a condition where plaque builds up in arteries.
How does atherosclerotic calcification differ from normal calcium metabolism?
Atherosclerotic calcification is different from normal calcium use. It’s when calcium builds up in artery walls, unlike normal calcium use in the body.
What is the relationship between atherosclerosis and calcification?
Atherosclerosis and calcification are closely related. Atherosclerosis can lead to artery hardening, which increases the risk of heart problems.
Is atherosclerotic calcification an active or passive process?
Atherosclerotic calcification is an active process. It involves complex biological mechanisms, similar to bone formation.
How is atherosclerotic calcification detected and measured?
Imaging techniques like CT scans can detect and measure atherosclerotic calcification. They show how much calcium is in artery walls.
What are the risk factors for developing arterial calcification?
Risk factors include age, high blood pressure, diabetes, high cholesterol, and smoking. These can be changed or not changed.
Can atherosclerotic calcification be prevented?
Yes, it can be prevented. Eating right, staying active, and managing health conditions like high blood pressure and diabetes help.
What are the treatment options for existing atherosclerotic calcification?
Treatments include medicines like statins and bisphosphonates. Surgery or procedures like angioplasty and stenting are also options.
Why is it important to manage atherosclerotic calcification?
Managing it is key to preventing heart attacks and strokes. It helps slow down atherosclerosis and keeps arteries healthy.
References
Medical News Today. (2022). Arteries: Function, anatomy, and types. https://www.medicalnewstoday.com/articles/arteries