Last Updated on November 20, 2025 by Ugurkan Demir
Feeling tired and weak for a long time might mean there’s something wrong. At Liv Hospital, we’ve noticed how anemia can happen when autoimmune diseases attack the body’s red blood cells. Discover 7 key autoimmune diseases that cause anemia. Learn about these serious conditions and the link between immunity and low blood count.
Anemia means not enough red blood cells or hemoglobin. Autoimmune diseases can cause this, leading to health problems. We’ll look at seven main conditions that can cause anemia, helping you understand the causes and effects.
Key Takeaways
- Autoimmune diseases can cause anemia by attacking the body’s red blood cells.
- Conditions like rheumatoid arthritis and Crohn’s disease can lead to anemia of inflammation.
- Understanding the link between autoimmune diseases and anemia is key to treatment.
- At Liv Hospital, we offer full care for patients with autoimmune diseases that cause anemia.
- Early diagnosis and treatment can greatly improve patient outcomes.
Understanding the Link Between Autoimmunity and Anemia
Autoimmune diseases can cause anemia in several ways. They can directly attack red blood cells or cause chronic inflammation. We will look at how these actions lead to anemia in people with autoimmune conditions.
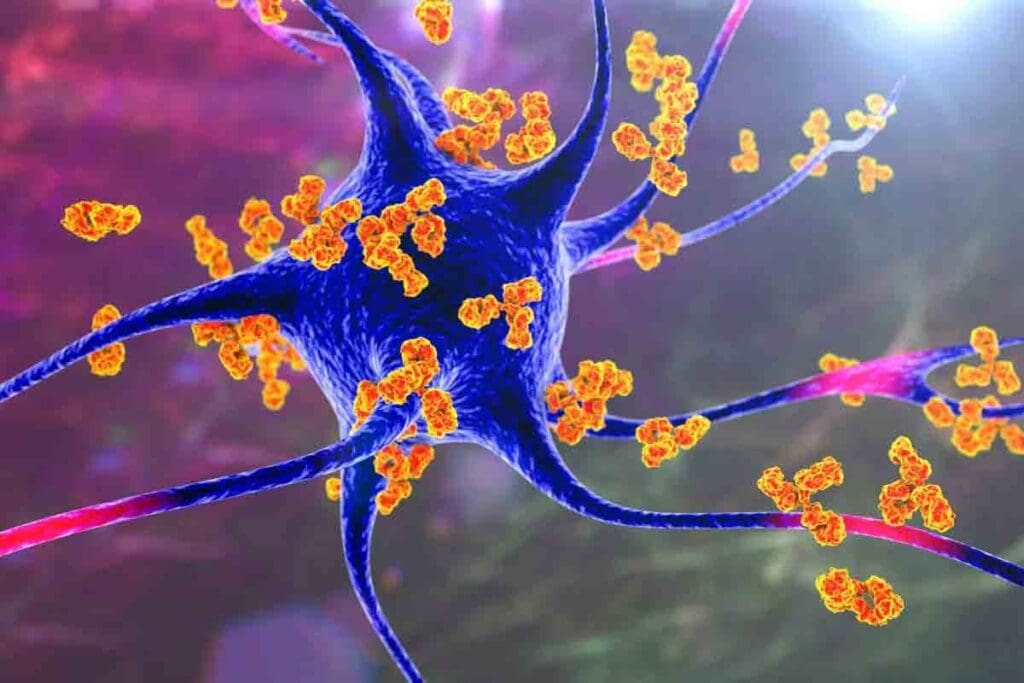
How Autoimmune Responses Target Red Blood Cells
In autoimmune hemolytic anemia (AIHA), the immune system makes antibodies against the body’s own red blood cells. This marks them for destruction. Factors like genetics, infections, and some medicines can trigger this response. As a result, red blood cells are destroyed faster than they can be made, causing anemia.
The immune system’s attack on red blood cells happens in different ways. It can produce autoantibodies that stick to red blood cells. This makes them more likely to be destroyed by the spleen. This shows how complex the relationship between the immune system and red blood cell production is.
The Impact of Chronic Inflammation on Blood Cell Production
Many autoimmune diseases cause chronic inflammation. This can harm blood cell production. Inflammatory cytokines can lower the production of erythropoietin, a hormone needed for red blood cells. This leads to anemia of chronic disease (ACD).
ACD is marked by a decrease in red blood cell production and a shortening of their lifespan. Chronic inflammation also makes iron hard to use for making red blood cells. This results in a functional iron deficiency, even with enough iron stores. This further adds to anemia.
Prevalence and Statistics: 30-50% of Hospital Anemia Cases
Anemia is a big problem in hospitals, mainly in patients with chronic diseases. Studies show that anemia of chronic disease (ACD) makes up 30-50% of anemia cases in hospitals. The high rate of anemia in autoimmune disease patients highlights the need for better management.
| Condition | Prevalence of Anemia | Mechanism |
| Rheumatoid Arthritis | 30-60% | Chronic inflammation, ACD |
| Systemic Lupus Erythematosus | 20-50% | AIHA, ACD, bone marrow suppression |
| Inflammatory Bowel Disease | 20-70% | Blood loss, malabsorption, ACD |
It’s important to understand how anemia is linked to autoimmune diseases. By knowing the causes and effects, healthcare providers can create better treatment plans. This helps manage these conditions better and improves patient outcomes.
Anemia of Chronic Disease (ACD/AOCD): The Common Denominator

Chronic inflammation or immune activation can cause Anemia of Chronic Disease (ACD). This condition affects how red blood cells are made. We will look into ACD’s details, including its definition, medical terms, and how it develops.
What is Anemia of Chronic Disease?
Anemia of Chronic Disease (ACD) happens when the body makes fewer red blood cells due to long-term inflammation or immune issues. It’s often seen in people with conditions like rheumatoid arthritis and lupus. The anemia comes from the body’s fight against chronic disease, which messes with red blood cell production and regulation.
AOCD Medical Terminology and Abbreviations Explained
The terms around ACD can be tricky. AOCD means Anemia of Chronic Disease/Disorder, and it’s also called Anemia of Inflammation. Knowing these terms is key to diagnosing and treating ACD well.
Mechanisms of ACD Development
Several important mechanisms lead to ACD:
- Inflammation-induced cytokine production: Cytokines can slow down the production of red blood cells.
- Hepcidin upregulation: Hepcidin controls iron use, and too much of it means less iron for making red blood cells.
- Erythropoietin resistance: Long-term inflammation makes the body less responsive to erythropoietin, a hormone that helps make red blood cells.
Distinguishing ACD from Iron Deficiency Anemia
Telling ACD apart from iron deficiency anemia (IDA) is important for the right treatment. Both cause anemia, but they have different causes and treatments. The main differences are:
| Characteristics | ACD | IDA |
| Primary Cause | Chronic inflammation | Iron deficiency |
| Serum Iron | Normal or low | Low |
| Hepcidin Levels | Elevated | Low |
Knowing these differences helps in making the right diagnosis and treatment.
Autoimmune Hemolytic Anemia (AIHA): Direct Attack on Red Blood Cells
Autoimmune Hemolytic Anemia (AIHA) is a condition where the immune system attacks the body’s red blood cells. This leads to the early destruction of these cells, causing anemia. We will look into AIHA’s types, causes, diagnosis, and treatment options.
Differentiating Between Warm and Cold AIHA
AIHA is divided into two types based on when the autoantibodies are most active. These are warm AIHA and cold AIHA.
- Warm AIHA: This type occurs when autoantibodies bind to red blood cells at body temperature, causing their destruction.
- Cold AIHA: In this type, autoantibodies react with red blood cells at temperatures below normal body temperature, usually under 30°C.
Knowing the difference between warm and cold AIHA is key to choosing the right treatment.
Causes and Triggers of AIHA
The exact cause of AIHA varies, but it often involves genetics and environmental triggers. Some cases are linked to conditions like lymphoproliferative disorders, infections, or other autoimmune diseases.
| Cause/Trigger | Description |
| Lymphoproliferative Disorders | Conditions like lymphoma can lead to AIHA by disrupting normal immune function. |
| Infections | Certain infections can trigger AIHA, possibly through molecular mimicry. |
| Autoimmune Diseases | Diseases like systemic lupus erythematosus can increase the risk of developing AIHA. |
Diagnostic Approaches for AIHA
Diagnosing AIHA requires a mix of clinical evaluation, lab tests, and sometimes, specialized investigations.
Laboratory Tests:
- Direct Coombs test (Direct Antiglobulin Test)
- Indirect Coombs test (Indirect Antiglobulin Test)
- Complete Blood Count (CBC)
- Reticulocyte count
These tests confirm hemolytic anemia and identify antibodies or complement proteins on red blood cells.
Treatment Options and Prognosis
Treatment for AIHA varies based on the cause, severity, and type. Options include corticosteroids, immunosuppressive therapy, and splenectomy in severe cases.
Treatment Approaches:
- Corticosteroids as first-line treatment
- Immunosuppressive drugs for refractory cases
- Splenectomy for patients not responding to medical therapy
The prognosis varies. Some patients achieve complete remission, while others need ongoing management.
Systemic Lupus Erythematosus (SLE) and Anemia
SLE, or Systemic Lupus Erythematosus, affects many parts of the body. It can cause anemia in several ways. This chronic autoimmune disease often leads to anemia, a common complication.
Multiple Mechanisms of Anemia in Lupus
Anemia in SLE patients comes from different causes. These include autoimmune hemolytic anemia, chronic inflammation, and bone marrow suppression. Knowing these causes helps in managing the condition better.
Autoimmune Hemolytic Anemia (AIHA) happens when the immune system attacks the body’s red blood cells. In SLE, AIHA can cause severe anemia.
Hemolytic Anemia in SLE Patients
Hemolytic anemia occurs when red blood cells are destroyed too quickly. In SLE, autoantibodies against red blood cells can cause this. A direct Coombs test is used to diagnose it.
| Diagnostic Criteria | Description |
| Direct Coombs Test | Detects antibodies or complement proteins attached to red blood cells. |
| Hemoglobin Levels | Low hemoglobin indicates anemia. |
| Reticulocyte Count | An elevated count suggests a bone marrow response to anemia. |
Bone Marrow Suppression in Lupus
SLE can also lead to anemia by suppressing the bone marrow. This makes it hard for the body to make blood cells. This can happen because of the disease itself or because of treatments like immunosuppressive drugs.
Managing Anemia in Lupus Patients
Managing anemia in SLE patients needs a detailed plan. This includes treating lupus, managing hemolytic anemia, and addressing bone marrow suppression. Treatment might include corticosteroids, immunosuppressive therapy, and sometimes blood transfusions.
Understanding how SLE and anemia are connected helps doctors create better treatment plans. This can improve patient outcomes.
Rheumatoid Arthritis: How It Leads to Chronic Anemia
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that can cause anemia. This happens because of the inflammation it causes throughout the body. We will look at how RA and anemia are connected, focusing on the reasons and how to manage them.
Inflammatory Pathways in RA-Associated Anemia
Anemia in RA is mainly caused by ongoing inflammation. Inflammatory cytokines like TNF-alpha and IL-6 are key players. They can:
- Reduce the production of erythropoietin, a hormone needed for red blood cells.
- Affect iron levels, making less iron available for making red blood cells.
- Stop the growth of cells that make red blood cells.
This complex process leads to anemia of chronic disease (ACD). ACD is a type of anemia seen in people with long-term inflammation.
Impact of RA Medications on Blood Cell Production
RA medications are vital for controlling the disease. Yet, some can affect how blood cells are made. For example:
- DMARDs (Disease-Modifying Antirheumatic Drugs) like methotrexate can slow down bone marrow, leading to anemia.
- Biologic agents that target TNF-alpha can help anemia by reducing inflammation. But they can also affect blood cell counts differently.
It’s important to keep an eye on blood cell counts in RA patients, even more so when starting or changing medications.
Monitoring and Managing Anemia in RA Patients
Managing anemia in RA patients needs a detailed plan:
- Regular checks of hemoglobin levels and inflammation markers.
- Improving RA control with the right medication.
- Iron supplements or agents that help make red blood cells when needed.
“The goal is to improve not just joint symptoms but the overall quality of life for these patients.”
Understanding the link between RA and anemia helps healthcare providers create better treatment plans. These plans address both conditions, improving patient outcomes.
Inflammatory Bowel Disease and Anemia Connection
IBD, which includes Crohn’s disease and ulcerative colitis, is linked to anemia. This is due to inflammation, blood loss, and poor nutrient absorption. We will look into how these conditions differ in causing anemia and how it is treated.
Crohn’s Disease vs. Ulcerative Colitis: Anemia Profiles
Crohn’s disease and ulcerative colitis are both IBD, but they affect the body differently. Crohn’s disease can hit any part of the gut, causing more nutrient issues. On the other hand, ulcerative colitis mainly affects the colon’s lining.
Studies show that Crohn’s disease patients are more likely to get anemia. This is because it affects more areas of the gut. We will dive into the specific anemia types each condition can cause.
- Crohn’s disease often leads to iron deficiency anemia due to chronic blood loss and malabsorption.
- Ulcerative colitis also results in iron deficiency anemia, mainly from blood loss.
- Both conditions can cause anemia of chronic disease due to ongoing inflammation.
Blood Loss and Malabsorption Factors
Blood loss and poor nutrient absorption are big reasons for anemia in IBD patients. Chronic bleeding in the gut lowers iron levels, causing anemia. Also, the inflammation in IBD can lead to anemia of chronic disease.
Malabsorption is a big deal, more so in Crohn’s disease. The small intestine’s involvement can block the absorption of iron, vitamin B12, and folate. We will explore how these factors contribute to anemia.
Treatment Approaches for IBD-Related Anemia
Treating anemia in IBD patients involves several steps. First, we tackle the root cause of anemia, whether it’s iron deficiency, vitamin deficiency, or chronic disease anemia. Iron supplements are key for iron deficiency anemia. Vitamin B12 and folate supplements are used when needed.
Managing the underlying IBD with anti-inflammatory drugs can also help with anemia. We will discuss the different treatment options and their impact on patient care.
- Iron supplementation for iron deficiency anemia.
- Vitamin B12 and folate supplements for deficiencies.
- Addressing the underlying IBD through anti-inflammatory medications.
- In some cases, erythropoiesis-stimulating agents may be considered.
Autoimmune Diseases That Cause Anemia: Celiac Disease and Pernicious Anemia
Celiac disease and pernicious anemia are autoimmune disorders that can cause anemia. Celiac disease happens when the body reacts to gluten, making it hard to absorb nutrients. Pernicious anemia occurs when the body attacks the intrinsic factor needed for vitamin B12 absorption. Both diseases show how complex autoimmunity and anemia are linked.
Celiac Disease: Mechanism of Nutrient Malabsorption
Celiac disease is caused by an immune reaction to gluten. This reaction damages the small intestine, making it hard to absorb nutrients. Nutrients like iron, folate, and vitamin B12 are key for making red blood cells. Without them, anemia can occur.
Pernicious Anemia: Autoimmune Attack on Intrinsic Factor
Pernicious anemia happens when the body attacks the stomach’s parietal cells or the intrinsic factor they make. An intrinsic factor is needed for vitamin B12 absorption. Without it, vitamin B12 deficiency leads to megaloblastic anemia. This shows how autoimmunity directly affects the blood system.
Diagnostic Challenges and Solutions
Diagnosing celiac disease and pernicious anemia can be tough. Their symptoms are similar to other conditions. For celiac disease, tests like tissue transglutaminase antibody and intestinal biopsy are used. For pernicious anemia, tests include vitamin B12 levels and intrinsic factor antibody. Early diagnosis is key to avoiding serious problems.
Dietary Interventions and Supplementation
Managing celiac disease means following a strict gluten-free diet. This diet helps heal the intestine and improve nutrient absorption. For pernicious anemia, vitamin B12 supplements are needed, often given as injections or tablets. It’s important to watch for other deficiencies and anemia in both cases.
| Disease Characteristics | Celiac Disease | Pernicious Anemia |
| Autoimmune Target | Small intestine (response to gluten) | Gastric parietal cells or intrinsic factor |
| Nutritional Deficiency | Multiple (iron, folate, vitamin B12) | Vitamin B12 |
| Diagnostic Approach | Serology, intestinal biopsy | Vitamin B12 levels, intrinsic factor antibody |
| Management | Gluten-free diet | Vitamin B12 supplementation |
Chronic Infections and Autoimmune-Like Anemia
Chronic infections like endocarditis, tuberculosis, and HIV can cause anemia. This happens because these infections cause long-term inflammation and immune system activation. These effects harm the production of red blood cells.
Endocarditis and Anemia
Endocarditis is an infection of the heart’s inner lining. It can cause anemia because of the ongoing inflammation. This inflammation leads to the production of cytokines, which slow down the production of red blood cells.
Studies have found that people with endocarditis often have anemia. This is a big warning sign for serious health problems and death.
Tuberculosis-Associated Anemia
Tuberculosis (TB) is another chronic infection that can cause anemia. The reasons for TB-related anemia are complex. They include ongoing inflammation, poor nutrition, and damage to the bone marrow.
Research shows that anemia in TB patients means a worse outcome and longer recovery times.
HIV and Autoimmune Hematologic Complications
HIV infection can also lead to anemia. The reasons include immune system activation, ongoing inflammation, and direct harm to the bone marrow by the virus.
Anemia in HIV patients is linked to the disease getting worse and a higher risk of death.
To understand how these chronic infections cause anemia, let’s look at some data:
| Infection | Mechanism of Anemia | Prevalence of Anemia |
| Endocarditis | Chronic inflammation, cytokine-mediated suppression | 40-60% |
| Tuberculosis | Chronic inflammation, malnutrition, and bone marrow suppression | 30-50% |
| HIV | Immune activation, chronic inflammation, and bone marrow effects | 20-40% |
The table shows that chronic infections play a big role in causing anemia. It’s important to understand these causes to manage anemia in patients with chronic infections.
Diagnosis and Treatment Approaches for Autoimmune Anemias
Understanding autoimmune anemias is key to their diagnosis and treatment. These conditions, like Autoimmune Hemolytic Anemia (AIHA), are complex. They require a detailed medical plan.
Laboratory Tests and Diagnostic Markers
Lab tests are the first step in diagnosing autoimmune anemia. The Direct Coombs Test is vital. It finds antibodies or proteins attached to red blood cells. Other tests include:
- Complete Blood Count (CBC) to check anemia severity
- Reticulocyte count to see bone marrow activity
- Lactate Dehydrogenase (LDH) levels to measure hemolysis
- Bilirubin levels are used to check red blood cell breakdown
These tests help doctors figure out the type of anemia. They guide further treatment.
Immunosuppressive Therapies
Immunosuppressive therapies are key in treating autoimmune anemias. They aim to stop the immune system from attacking red blood cells. Common treatments include:
- Corticosteroids, like prednisone, are used to lower antibody production
- Immunosuppressive drugs like azathioprine or cyclophosphamide are used for severe cases
These treatments work well but need close monitoring for side effects.
Targeted Biological Treatments
Targeted biological treatments offer a precise way to manage autoimmune anemias. Rituximab, a monoclonal antibody, targets B-cells. It helps by reducing antibody production.
Supportive Care and Blood Transfusions
Supportive care, including blood transfusions, is vital for severe anemia. Transfusions increase red blood cells and improve oxygen delivery. But they should be used carefully to avoid iron overload and other issues.
A detailed treatment plan is essential. It combines different approaches for the best results.
Conclusion: Living with Chronic Anemia in Autoimmune Conditions
Chronic anemia is a big problem for people with autoimmune diseases. It really affects their quality. We’ve talked about how different types of anemia are linked to diseases like lupus, rheumatoid arthritis, and inflammatory bowel disease.
Managing anemia means more than just treating it. It’s about understanding the connection between autoimmunity and anemia. By focusing on the root cause and using the right treatments, doctors can help patients live better lives.
Dealing with chronic anemia in autoimmune diseases needs a team effort. It involves medicine, lifestyle changes, and teaching patients. A caring approach helps people with these complex conditions live better and manage their health more effectively.
FAQ
What is Anemia of Chronic Disease (ACD/AOCD)?
Anemia of Chronic Disease (ACD/AOCD) happens when long-term inflammation causes anemia. It often comes with chronic infections, autoimmune diseases, and cancer.
How do autoimmune diseases cause anemia?
Autoimmune diseases can lead to anemia in several ways. This includes chronic inflammation, autoimmune hemolytic anemia, and bone marrow suppression.
What is the difference between ACD/AOCD and iron deficiency anemia?
ACD/AOCD is caused by long-term inflammation. Iron deficiency anemia is due to not enough iron. Tests can tell them apart.
What is Autoimmune Hemolytic Anemia (AIHA)?
Autoimmune Hemolytic Anemia (AIHA) occurs when the immune system attacks and destroys red blood cells. This leads to anemia.
How is AIHA diagnosed and treated?
AIHA is found through lab tests, like the direct Coombs test. Treatment includes immunosuppressive therapies, corticosteroids, and sometimes blood transfusions.
Can Rheumatoid Arthritis (RA) cause anemia?
Yes, Rheumatoid Arthritis (RA) can cause anemia. This is because chronic inflammation affects red blood cell production.
How is anemia managed in patients with Systemic Lupus Erythematosus (SLE)?
Anemia in SLE patients is treated with a mix of treatments. This includes corticosteroids, immunosuppressive therapies, and erythropoietin-stimulating agents.
Is anemia a common complication of Inflammatory Bowel Disease (IBD)?
Yes, anemia is common in Inflammatory Bowel Disease (IBD). This includes Crohn’s disease and ulcerative colitis. It’s due to chronic blood loss, malabsorption, and inflammation.
Can celiac disease and pernicious anemia cause anemia?
Yes, celiac disease can cause anemia due to poor nutrient absorption. Pernicious anemia is an autoimmune condition that leads to vitamin B12 deficiency.
How are chronic infections related to anemia?
Chronic infections, like tuberculosis and HIV, can cause anemia. This is through chronic inflammation, bone marrow suppression, and autoimmune responses.
What are the treatment options for autoimmune anemias?
Treatment for autoimmune anemias includes immunosuppressive therapies and targeted biological treatments. Supportive care, like blood transfusions, is also used.
References:
- Zanella, A., & Barcellini, W. (2014). Treatment of Autoimmune Hemolytic Anemia. Current Hematologic Malignancy Reports, 9(3), 198-205. https://pubmed.ncbi.nlm.nih.gov/25066517/