When the immune system attacks the healthy tissues of the eye, it can cause serious problems. Autoimmune disorders can affect any part of the eye. This can lead to symptoms like blurred vision, double vision, and sensitivity to light.The ultimate guide to autoimmune eye disease treatment. Discover proven strategies and new options to manage symptoms and protect vision.
At Liv Hospital, we know how important it is to diagnose and treat autoimmune eye conditions properly. Our team uses the latest treatment strategies and follows international best practices. We focus on our patients, combining ophthalmology and immunology to help them see better.
Key Takeaways
- Autoimmune disorders can cause serious eye complications.
- Symptoms include blurred vision, double vision, and sensitivity to light.
- Specialized diagnosis is key for effective treatment.
- Liv Hospital offers a patient-centered approach to treating autoimmune eye conditions.
- Combining ophthalmology and immunology expertise is key to successful treatment.
Understanding Autoimmune Eye Diseases
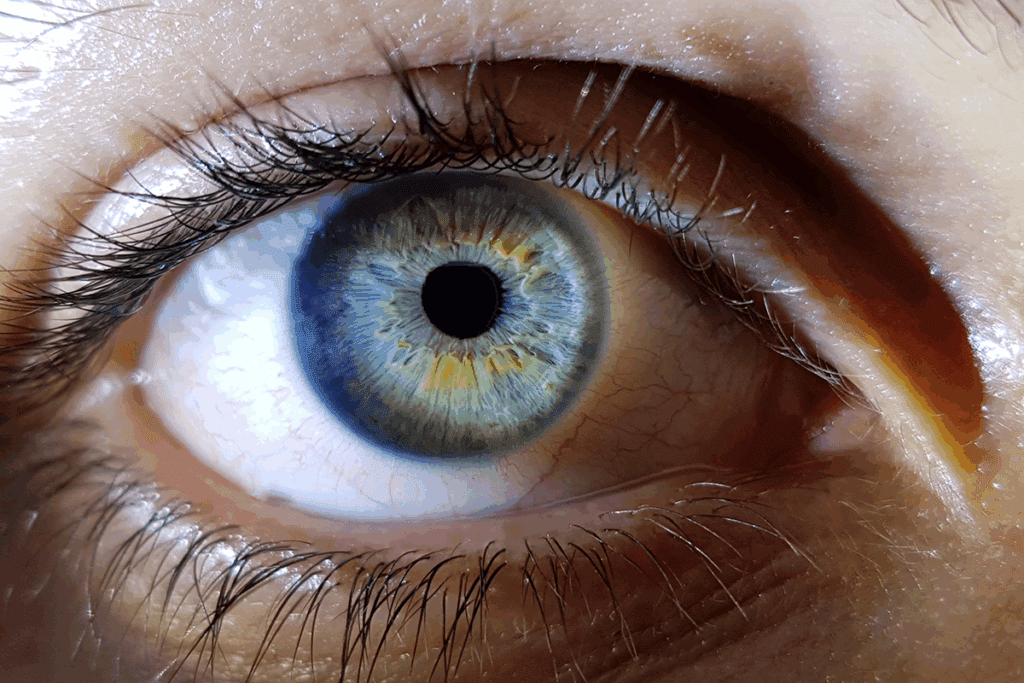
Autoimmune eye diseases are complex conditions where the immune system attacks the eyes by mistake. This can lead to inflammation and vision loss. These diseases can harm different parts of the eye, like the uvea, retina, and optic nerve.
Research shows that autoimmune diseases can affect every part of the eye. This causes inflammation and damage to the eye’s delicate structures. For example, autoimmune uveitis and dry eye disease linked to systemic autoimmune disorders show how the eyes can be affected.
What Causes the Immune System to Attack the Eyes?
The exact reason for autoimmune eye diseases is not known. It’s thought that genetics and environmental factors trigger the immune system’s wrong response. In these diseases, the immune system mistakes the body’s own tissues for foreign substances, attacking the eyes.
This wrong immune response can cause inflammation and damage to the eyes. This can lead to vision problems. Understanding the causes and how these diseases work is key to finding good treatments.
Prevalence and Impact on Vision
Autoimmune eye diseases are not common but can greatly affect vision and life quality. The frequency of these diseases varies by the specific disease and the group being studied. For example, autoimmune uveitis is a major cause of vision loss in young adults.
The effects of autoimmune eye diseases on vision can be serious. Complications include chronic inflammation, vision loss, and even blindness if not treated well. Early diagnosis and the right treatment are vital to avoid long-term damage and keep vision.
Common Types of Autoimmune Eye Diseases

Autoimmune eye diseases happen when the immune system attacks the eyes. This can cause serious eye problems and affect vision.
Autoimmune Uveitis
Autoimmune uveitis is a major cause of vision loss and blindness. It involves inflammation of the uvea, the eye’s middle layer. This inflammation can damage the eye’s delicate parts.
Treatment approaches for this condition include reducing inflammation and controlling the immune system. Doctors often use corticosteroids and immunosuppressive drugs.
Dry Eye Disease in Autoimmune Conditions
Dry eye disease is common in people with autoimmune diseases. It affects 30 to 50 percent of those with autoimmune thyroid disease.
Dry eye disease can greatly reduce a patient’s quality of life. Symptoms include dryness, irritation, and vision problems. Treatment involves artificial tears, anti-inflammatory drugs, and other methods to improve eye health.
Ocular Manifestations of Systemic Autoimmune Diseases
Systemic autoimmune diseases like Sjögren’s syndrome and lupus can harm the eyes. They can cause dry eye, uveitis, and retinal vasculitis.
It’s important to understand how these diseases affect the eyes. A team of ophthalmologists, rheumatologists, and other specialists is needed for effective care.
Recognizing Symptoms and Getting Diagnosed
Autoimmune eye diseases show unique symptoms. Recognizing them early can lead to better results. We’ll look at common symptoms, diagnostic tests, and why early detection is key.
Common Symptoms of Autoimmune Eye Conditions
Symptoms include blurred vision, double vision, sensitivity to light, and eye pain. These can greatly affect daily life. It’s important to see a doctor if these symptoms last or get worse.
Autoimmune eye diseases can also cause dryness, redness, and feeling like something is in your eye. Spotting these symptoms early can help manage the condition better.
Diagnostic Tests and Procedures
Diagnosing these diseases involves a detailed eye exam and various tests. These include checking tear production, tear quality, and looking at the cornea and conjunctiva.
- Tests to assess tear production and quality
- Examination of the cornea and conjunctiva
- Imaging tests to evaluate the retina and other internal eye structures
These tests help doctors figure out the specific disease and the best treatment.
The Importance of Early Detection
Early detection is vital to prevent vision loss and manage symptoms. Early treatment can reduce complications.
Regular eye exams are essential, even more so for those with autoimmune disorders. Conditions like lupus can harm the eyes, so regular checks are important.
Comprehensive Autoimmune Eye Disease Treatment Approaches
Managing autoimmune eye diseases well means more than just treating symptoms. We also focus on the underlying immune issues and how they affect overall health.
Treatment Goals and Considerations
Our main goals in treating these diseases are to control the immune response, lessen symptoms, and protect vision. We look at the disease type, its severity, and the patient’s health. Treatments include eye drops, medicines that suppress the immune system, and biologic agents. These can be used alone or together for the best results.
The right treatment depends on many factors. These include the disease’s severity, any other autoimmune conditions, and how the patient has reacted to treatments before. Starting treatment early is key to avoid vision loss and improve outcomes.
Multidisciplinary Care Team
Effective management of autoimmune eye diseases needs a team effort. This team includes eye doctors, rheumatologists, immunologists, and others. They work together to create a detailed treatment plan. The benefits of this team approach are:
- Coordinated care for both eye and body issues
- Access to a wide range of treatments and expertise
- Improved patient results through teamwork
Creating a Personalized Treatment Plan
Every patient with autoimmune eye disease is different. Their treatment plan should reflect this. We tailor plans based on the patient’s condition, medical history, and personal needs.
A tailored plan might include:
Treatment Modality | Description | Potential Benefits |
Topical Corticosteroids | Eye drops or ointments that reduce inflammation | Rapid reduction of ocular inflammation |
Systemic Immunosuppressants | Medications that suppress the immune system | Control of systemic autoimmune response |
Biologic Agents | Targeted therapies that modulate specific immune pathways | Precise control of autoimmune response with potentially fewer side effects |
By taking a detailed and personalized approach, we can better help patients with autoimmune eye diseases. This improves their outcomes and quality of life.
Topical Treatments for Autoimmune Eye Conditions
Topical treatments are key in managing autoimmune eye conditions. They reduce inflammation and ease symptoms. These treatments are applied directly to the eye, providing targeted relief and minimizing systemic side effects.
Corticosteroid Eye Drops
Corticosteroid eye drops are a common treatment for autoimmune eye conditions. They are effective in reducing inflammation and swelling. But, long-term use can lead to side effects such as increased intraocular pressure and cataract formation.
To reduce these risks, corticosteroid eye drops are used in a tapering dose regimen. This starts with a higher frequency and gradually reduces as the inflammation comes under control. Regular monitoring by an ophthalmologist is essential to manage any side effects.
Immunomodulators: Cyclosporine and Tacrolimus
Immunomodulators like cyclosporine and tacrolimus are another class of topical treatments for autoimmune eye conditions. These medications modify the immune response, reducing inflammation without the broad effects of corticosteroids.
Cyclosporine eye drops are useful in treating dry eye associated with autoimmune conditions like Sjögren’s syndrome. Tacrolimus, though less commonly used topically for eye conditions, has shown promise in managing severe ocular inflammation.
Medication | Primary Use | Common Side Effects |
Corticosteroid Eye Drops | Reducing inflammation | Increased intraocular pressure, cataract formation |
Cyclosporine Eye Drops | Treating dry eye, reducing inflammation | Local irritation, burning sensation |
Tacrolimus | Managing severe ocular inflammation | Local irritation, possible systemic absorption |
Artificial Tears and Lubricants
Artificial tears and lubricants are essential for managing dry eye symptoms associated with autoimmune conditions. They moisturize the ocular surface, reduce discomfort, and improve vision clarity.
There are various types of artificial tears available, including preservative-free options for sensitive eyes. Patients may need to try different products to find the one that works best for their condition.
“The use of artificial tears is a cornerstone in the management of dry eye syndrome, providing symptomatic relief and helping to maintain the integrity of the ocular surface.”
— Ophthalmology Guidelines
We recommend using artificial tears regularly, specially in dry environments or during activities that exacerbate dry eye symptoms. In some cases, punctal plugs may be used in conjunction with artificial tears to conserve tears and reduce symptoms further.
Systemic Medications and Therapies
Systemic medications are key in fighting autoimmune eye diseases. They tackle the immune system’s wrong actions. This helps reduce eye inflammation and damage.
Oral Corticosteroids
Oral corticosteroids are vital for treating autoimmune eye diseases, mainly during flare-ups. They calm down the immune system, cutting down inflammation. Prednisone is a common one. But, long-term use can lead to serious side effects like osteoporosis and diabetes.
Immunosuppressants: Methotrexate and Azathioprine
For long-term care, methotrexate and azathioprine are used. They are gentler on the immune system than corticosteroids. This makes them safer for long-term use, helping with conditions like autoimmune uveitis.
Medication | Mechanism of Action | Common Side Effects |
Methotrexate | Inhibits DNA synthesis, reducing immune cell proliferation | Liver toxicity, nausea, fatigue |
Azathioprine | Interferes with DNA synthesis, suppressing immune response | Nausea, vomiting, increased infection risk |
Biologic Agents: Rituximab
Rituximab targets B cells in the immune system. It’s used to treat autoimmune diseases, including eye conditions. By reducing B cells, it lessens the autoimmune attack and inflammation.
Emerging Therapies and Clinical Trials
New treatments for autoimmune eye diseases are being explored. This includes biologic agents and small molecule inhibitors. Janus kinase (JAK) inhibitors are showing promise in treating autoimmune diseases.
As research grows, patients with autoimmune eye diseases get more chances to try new treatments. These could be safer and more effective than current options.
Lifestyle Modifications and Self-Care Strategies
Making lifestyle changes can greatly improve life with autoimmune eye diseases. By focusing on diet, managing triggers, protecting your eyes, and adapting to vision changes, you can manage your condition better.
Dietary Considerations for Autoimmune Conditions
Eating a diet full of omega-3 fatty acids, antioxidants, and vitamins can help fight inflammation and keep your eyes healthy. Foods like leafy greens, fatty fish, and nuts are great choices. Drinking plenty of water is also key.
Some foods might make your symptoms worse. Keeping a food diary can help you find out which ones. This way, you can make changes to your diet that work best for you.
Managing Environmental Triggers
Things like dry air, UV rays, and smoke can irritate your eyes and make autoimmune eye conditions worse. Using humidifiers, wearing sunglasses with UV protection, and avoiding smoke can help.
Eye Protection and Hygiene
Good eye hygiene is essential for those with autoimmune eye diseases. This means gently cleaning your eyelids, not rubbing your eyes, and using warm compresses to remove debris.
It’s also important to protect your eyes from injury. Wearing protective eyewear during activities that could harm your eyes is a simple but effective step.
Coping with Vision Changes
Autoimmune eye diseases can lead to big changes in your vision, affecting your daily life. Adapting to these changes might mean using assistive devices, changing your routine, and getting support from healthcare professionals and support groups.
Lifestyle Modification | Benefit |
Increased Omega-3 Intake | Reduces inflammation |
UV-Protective Sunglasses | Protects eyes from UV radiation |
Humidifier Use | Reduces dry air irritation |
Navigating Treatment Costs and Insurance Coverage
Understanding treatment costs and insurance is key to managing autoimmune eye disease. The cost of treatment can be high. Knowing your insurance options is vital to get the care you need.
Understanding Insurance Coverage for Specialty Medications
Many treatments for autoimmune eye diseases are specialty medications. These can be expensive. But, knowing your insurance can help with costs. Check your insurance plan’s formulary to see if your meds are covered.
Some plans need prior approval or have special rules. To get the most from your insurance, we suggest:
- Reviewing your insurance plan’s formulary and coverage policies.
- Discussing coverage with your healthcare provider or a patient advocate.
- Exploring alternative treatment options if necessary.
Patient Assistance Programs
Patient assistance programs (PAPs) help patients afford medications. Many drug companies offer PAPs for autoimmune eye disease treatments. These programs can offer big financial help or even free meds to those who qualify.
To get into PAPs, you must meet income rules and show your financial situation. We advise working with your doctor or a patient advocate to find and apply for PAPs.
Advocating for Your Care
Being an advocate for your care is important when dealing with costs and insurance. This means understanding your insurance, talking with your doctor, and getting help when you need it. Don’t be shy about asking questions or seeking clarity on your care or coverage.
By staying informed and proactive, you can handle the financial side of treatment. We’re here to support you every step of the way.
Conclusion
Treating autoimmune eye disease needs a mix of treatments and lifestyle changes. We’ve looked into the causes, symptoms, and how to diagnose these diseases. A detailed care plan is key to managing them well.
A team of doctors is important for a treatment plan that fits each patient. This plan might include eye drops, pills, and changes in daily life. With a full care approach, patients can handle their condition better and live a fuller life.
We at our institution aim to give top-notch healthcare to international patients. Our team works hard to treat autoimmune eye diseases in a way that meets each patient’s needs. We combine the latest medical treatments with care that supports patients, helping them get the best results.
FAQ
What are autoimmune eye diseases?
Autoimmune eye diseases happen when the immune system attacks the eyes by mistake. This leads to inflammation and damage. Examples include autoimmune uveitis and dry eye disease linked to autoimmune conditions.
How does the immune system affect the eyes in autoimmune diseases?
In autoimmune eye diseases, the immune system’s wrong response causes inflammation and damage. This can lead to vision problems and other issues. Understanding this is key to finding effective treatments.
What are the common symptoms of autoimmune eye diseases?
Symptoms vary but often include redness, pain, blurred vision, dryness, and light sensitivity. Spotting these symptoms early is important for quick diagnosis and treatment.
How are autoimmune eye diseases diagnosed?
Diagnosis involves a detailed eye exam, looking at your medical history, and tests like OCT and fluorescein angiography. Blood tests also check for specific autoimmune markers.
What treatment options are available for autoimmune eye diseases?
Treatments include eye drops, artificial tears, and systemic medications. The right treatment depends on the condition and its severity.
Can lifestyle changes help manage autoimmune eye diseases?
Yes, making dietary changes, managing triggers, and protecting your eyes can help manage symptoms. These changes support your eye health.
How can I navigate the costs associated with treating autoimmune eye diseases?
Understanding insurance, looking into patient assistance programs, and talking to your healthcare provider can help with costs. It’s also good to discuss financial aspects with your doctor.
Are there any emerging therapies for autoimmune eye diseases?
Yes, research is ongoing, exploring new treatments like biologic agents. These new therapies offer hope for better outcomes for patients.
How can a multidisciplinary care team help in managing autoimmune eye diseases?
A team of healthcare professionals, including ophthalmologists and rheumatologists, work together. They create a personalized treatment plan, ensuring complete care for autoimmune eye diseases.
What is the importance of early detection in autoimmune eye diseases?
Early detection is key for timely treatment, which can prevent severe vision loss. Regular eye exams are vital, even more so for those with autoimmune conditions.
Can autoimmune diseases like lupus and Sjögren’s syndrome affect the eyes?
Yes, diseases like lupus and Sjögren’s syndrome can cause eye problems, including dry eye and uveitis. This highlights the need for thorough eye care when managing these diseases.
References
National Center for Biotechnology Information. Treating Autoimmune Eye Disease: A Concise Guide. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4181827/