Autoimmune eye inflammation, also known as uveitis, is a serious issue. It affects thousands of people globally. It’s a top reason for vision loss in those under 40 and can cause permanent blindness if not treated. Our guide reveals the best ways to manage autoimmune eye inflammation. Discover proven treatments and essential tips for lasting relief.
It’s important to know how autoimmune diseases and eye inflammation are linked. Getting help from specialists quickly and using advanced treatments can help save your vision.
We’ll look into this condition in detail. We’ll cover its causes, symptoms, treatment options, and how to manage it.
Key Takeaways
- Autoimmune eye inflammation is a serious condition that can lead to vision loss.
- Uveitis is a common term for autoimmune eye inflammation.
- Prompt treatment is essential to prevent permanent blindness.
- Understanding the connection between autoimmune diseases and eye inflammation is key.
- Advanced therapeutic options are available for managing the condition.
Understanding Autoimmune Eye Inflammation
It’s important to understand autoimmune eye inflammation to manage it well. Autoimmune eye diseases, like uveitis, happen when the body attacks its own eye tissues. This leads to inflammation and can cause serious vision problems.
What is Uveitis?
Uveitis is a type of autoimmune eye inflammation that affects the uvea, the eye’s middle layer. It can happen at any age and may cause vision loss if not treated. The uvea includes the iris, ciliary body, and choroid, which get inflamed in uveitis.
The Uvea and Its Components
The uvea is key to the eye, providing blood and color. It has three main parts:
- The iris, which controls light entry.
- The ciliary body, which makes fluid for the lens and cornea.
- The choroid, a blood vessel layer between the sclera and retina.
Prevalence and Risk Factors
Uveitis can be caused by many things, but up to 70% of cases have no known cause. It can affect one or more parts of the eye. Uveitis is common worldwide, affecting many people.
Risk Factors | Description |
Autoimmune Diseases | Conditions like rheumatoid arthritis and lupus can increase the risk of developing uveitis. |
Infections | Certain infections can trigger uveitis in susceptible individuals. |
Genetic Predisposition | A family history of autoimmune diseases may increase the risk. |
Knowing the risk factors and how common uveitis is helps in managing it. Healthcare providers can create better treatment plans by understanding causes and related conditions.
Common Types of Autoimmune Eye Inflammation
Autoimmune eye inflammation, or uveitis, comes in many forms. Each type affects different parts of the eye, leading to various symptoms. Knowing these types is key to finding the right treatment.
Anterior Uveitis
Anterior uveitis hits the front of the eye, between the cornea and lens. It causes eye pain, redness, and light sensitivity. It’s often seen in people with conditions like ankylosing spondylitis.
Intermediate Uveitis
Intermediate uveitis affects the vitreous humor and the retina’s edge. Symptoms include floaters and blurry vision. It’s less tied to systemic diseases than anterior uveitis.
Posterior Uveitis
Posterior uveitis targets the eye’s back, including the choroid and retina. It can cause vision loss and light flashes. It’s often linked to conditions like sarcoidosis.
Panuveitis
Panuveitis is a severe form that affects all layers of the uvea. It brings a mix of symptoms from anterior, intermediate, and posterior uveitis. It needs thorough treatment to manage the widespread inflammation.
Type of Uveitis | Area Affected | Common Symptoms | Associated Autoimmune Conditions |
Anterior Uveitis | Front part of the eye | Eye pain, redness, light sensitivity | Ankylosing Spondylitis |
Intermediate Uveitis | Vitreous humor and peripheral retina | Floaters, blurred vision | Less commonly associated with systemic autoimmune diseases |
Posterior Uveitis | Back part of the eye, choroid, and retina | Vision loss, flashes of light | Sarcoidosis |
Panuveitis | All layers of the uvea | Varied, including pain, vision disturbances | Multiple systemic autoimmune conditions |
Knowing the different types of autoimmune eye inflammation is vital for treatment. Each type has unique traits and may be linked to various diseases. By identifying the specific type, doctors can create a better treatment plan. This helps manage the condition and lowers the risk of complications.
Recognizing the Symptoms and Warning Signs
The signs of autoimmune eye inflammation can be hard to spot at first. But it’s key to catch them early to manage them well. Autoimmune eye inflammation, like uveitis, can cause serious problems if not treated quickly.
Common Symptoms to Monitor
Knowing the common signs of autoimmune eye inflammation is important. These symptoms include:
- Eye pain or discomfort
- Redness of the eye
- Blurred vision
- Sensitivity to light
- Floaters in the visual field
Watching for these signs is important. They can show that an inflammatory condition is present.
When to Seek Immediate Medical Attention
Some symptoms need quick medical help. If you have:
- Sudden severe eye pain
- Significant vision loss
- Increased sensitivity to light
- Severe redness
you should get medical help right away. These signs might mean a serious inflammatory episode or another serious issue.
Silent Chronic Inflammation Management
Managing silent chronic inflammation is tough because it often doesn’t show obvious signs. But, regular checks and advanced tests can help spot and manage it well.
Symptom | Description | Action Required |
Eye Pain | Discomfort or pain in the eye | Monitor closely |
Redness | Red appearance of the eye | Seek medical help if severe |
Blurred Vision | Difficulty seeing clearly | Immediate medical attention if sudden |
Sensitivity to Light | Discomfort or pain when exposed to light | Monitor; seek help if increasing |
Floaters | Spots or floaters in the visual field | Monitor; seek help if new or increasing |
Autoimmune Diseases Associated with Eye Inflammation
It’s important to know how autoimmune diseases affect the eyes. These diseases happen when the body’s immune system attacks its own tissues. This can cause inflammation and damage in the eyes, like uveitis.
About 40% of uveitis cases are linked to systemic autoimmune diseases. We’ll look at how diseases like rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, and sarcoidosis impact eye health.
Rheumatoid Arthritis and Eye Health
Rheumatoid arthritis (RA) mainly affects the joints but can also harm the eyes. It can cause dry eye, scleritis, and uveitis. These conditions can be severe if not treated properly.
A study in Arthritis & Rheumatology stresses the need to check the eyes of RA patients. It says, “the prevalence of ocular manifestations in RA patients is significant, highlighting the importance of regular ophthalmologic evaluation.”
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) can affect many parts of the body, including the eyes. It can cause retinal vasculitis, optic neuritis, and secondary Sjögren’s syndrome. Managing SLE needs a team effort from rheumatologists and ophthalmologists.
“Lupus can affect any part of the body, including the eyes, making complete care essential for patients with this condition.”
— Medical Expert, Rheumatologist
Ankylosing Spondylitis
Ankylosing spondylitis (AS) mainly affects the spine but can also harm the eyes. It often causes uveitis. The inflammation from AS can lead to serious eye problems, making early diagnosis and treatment critical.
Autoimmune Disease | Ocular Manifestations | Prevalence |
Rheumatoid Arthritis | Dry eye, scleritis, uveitis | Common |
Systemic Lupus Erythematosus | Retinal vasculitis, optic neuritis | Moderate |
Ankylosing Spondylitis | Uveitis | Common |
Sarcoidosis | Uveitis, retinal vasculitis | Moderate |
Sarcoidosis and Ocular Manifestations
Sarcoidosis is a disease that can affect any organ, including the eyes. It can cause uveitis, retinal vasculitis, or conjunctivitis. Diagnosing sarcoidosis can be hard, needing a mix of clinical tests, imaging, and biopsies.
Managing autoimmune diseases that affect the eyes needs a team effort. By understanding these connections, doctors can provide better care, improving patient outcomes.
The Diagnostic Journey for Autoimmune Eye Inflammation
Diagnosing autoimmune eye inflammation is a detailed process. It starts with a thorough eye exam. This is followed by tests to find the cause and how severe the inflammation is.
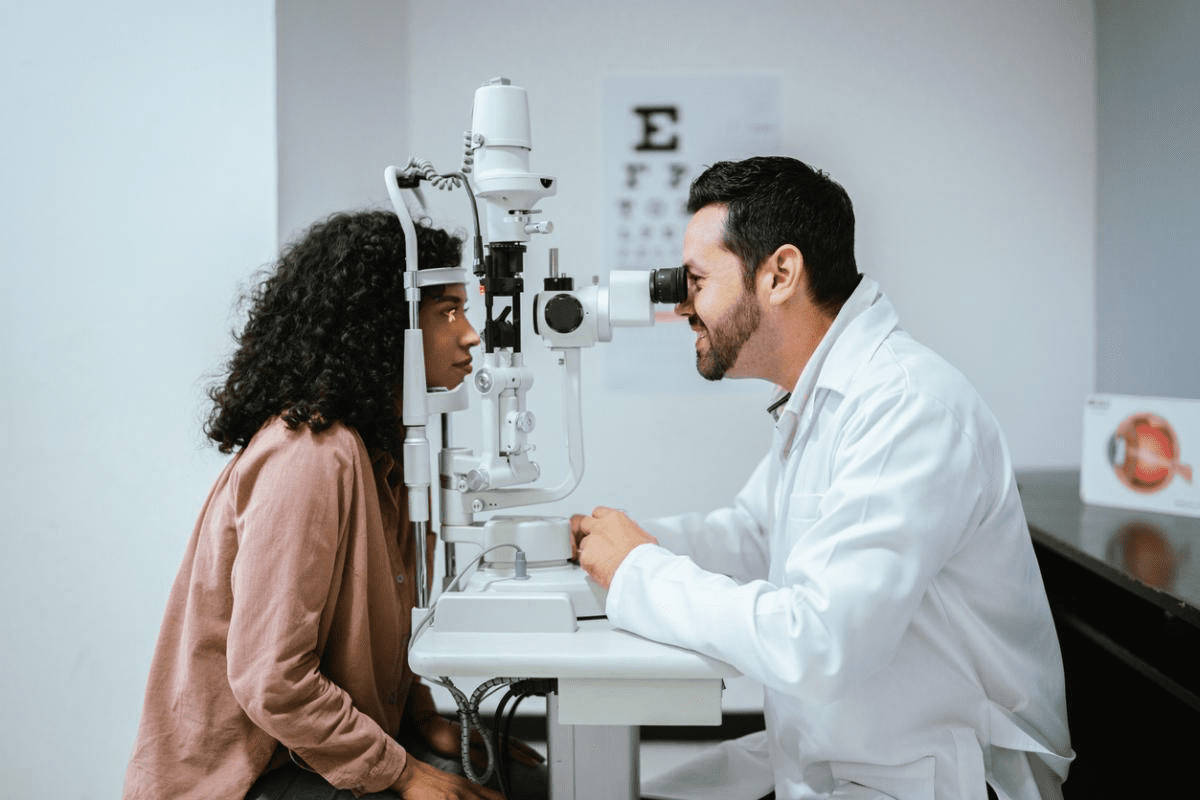
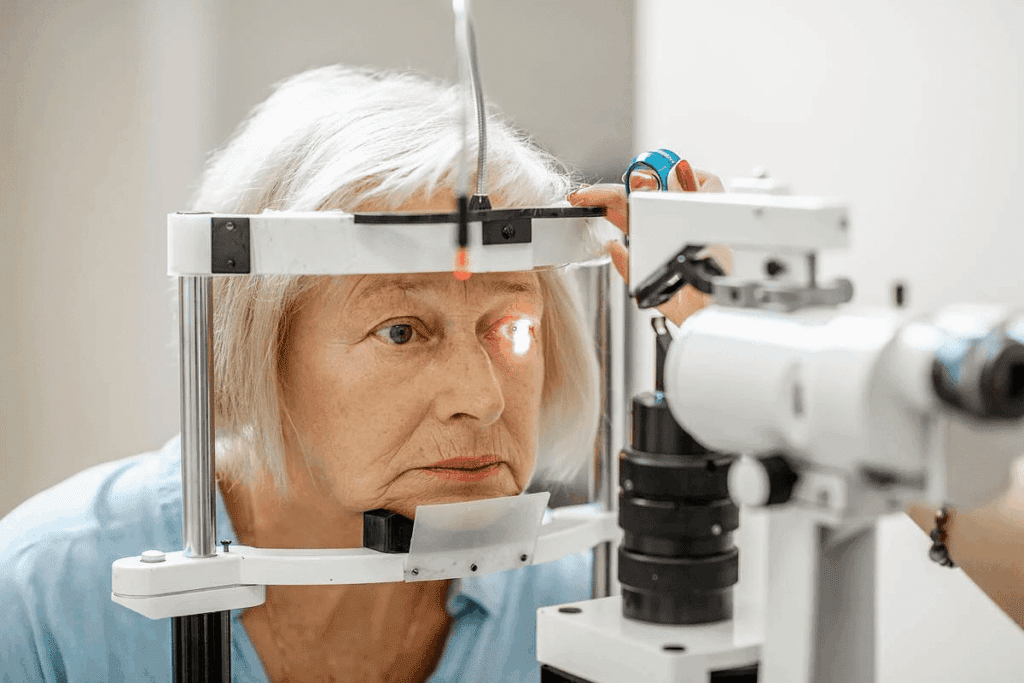
Initial Eye Examination Process
The first step is a detailed eye exam. This includes:
- Visual acuity testing to check vision sharpness
- Tonometry to measure eye pressure
- Slit-lamp examination to look at the front of the eye
- Ophthalmoscopy to check the back of the eye
Essential Laboratory Tests
Laboratory tests are key in diagnosing autoimmune eye inflammation. They include:
Test | Purpose |
Blood tests | To check for signs of infection or inflammation |
Complete Blood Count (CBC) | To evaluate overall health and detect a range of disorders |
Erythrocyte Sedimentation Rate (ESR) | To measure inflammation levels |
C-reactive Protein (CRP) | To assess systemic inflammation |
Advanced Imaging Studies
Advanced imaging is needed to fully understand autoimmune eye inflammation. These include:
- Optical Coherence Tomography (OCT) to see retinal layers
- Fluorescein angiography to check for vascular issues
- Ultrasound biomicroscopy (UBM) for detailed anterior segment images
The Multidisciplinary Diagnostic Approach
Diagnosing autoimmune eye inflammation needs a team effort. Ophthalmologists, rheumatologists, and others work together. This ensures a complete diagnosis and the best treatment plan.
Medical Treatment Options and Protocols
Treatment for autoimmune eye inflammation has grown, giving patients many options to manage their condition. The right treatment depends on how severe the inflammation is, the cause, and the patient’s health.
Corticosteroid Therapy Administration
Corticosteroids are key in treating autoimmune eye inflammation, like uveitis. They can be given locally (eye drops or injections) or systemically (oral or IV). Local treatment is often chosen for mild to moderate cases to avoid side effects.
Local corticosteroid administration includes eye drops, periocular injections, or intravitreal injections. Eye drops are used for anterior uveitis. Injections are for more severe or posterior segment inflammation.
Immunosuppressive Medication Management
For long-term treatment or severe inflammation not helped by corticosteroids, immunosuppressive meds are used. These meds reduce the immune system’s abnormal response, lowering inflammation.
Managing immunosuppressive therapy is important. It includes regular checks of blood counts and liver function to avoid side effects.
Biologic Agents and Their Application
Biologic agents are a new treatment for autoimmune eye inflammation. They target specific parts of the immune response, giving a more precise treatment than traditional meds.
Biologics are effective in managing uveitis linked to autoimmune diseases. They are used for patients who haven’t responded to other treatments or have severe disease.
Local vs. Systemic Treatment Considerations
Choosing between local and systemic treatment depends on several factors. These include the inflammation’s severity and location, the patient’s health, and the risk of side effects.
Treatment Approach | Indications | Potential Side Effects |
Local Corticosteroids | Mild to moderate uveitis, anterior uveitis | Cataract formation, increased intraocular pressure |
Systemic Corticosteroids | Severe uveitis, posterior or panuveitis | Osteoporosis, diabetes, weight gain |
Immunosuppressive Medications | Chronic or severe uveitis, failure of corticosteroids | Bone marrow suppression, increased infection risk |
Biologic Agents | Severe or refractory uveitis, associated autoimmune diseases | Increased infection risk, possible infusion reactions |
Knowing the different medical treatments for autoimmune eye inflammation is key to effective management. Healthcare providers consider the condition’s severity, cause, and patient’s health to tailor treatment plans.
Surgical Interventions for Severe Cases
For those with severe autoimmune eye inflammation, surgery might be needed. This is to stop complications and keep vision. When usual treatments don’t work, surgery becomes key.
Vitrectomy Procedure and Recovery
A vitrectomy removes the vitreous gel from the eye. It’s done for issues like vitreous opacification or retinal detachment from uveitis autoimmune. The surgery makes small cuts to remove the gel and debris.
After a vitrectomy, careful care is needed. This includes eye drops to fight inflammation. Patients are watched for any signs of problems or inflammation coming back.
Implantable Steroid Devices
Implantable steroid devices release corticosteroids directly to the eye. They’re great for chronic uveitis not helped by other treatments. These implants cut down on systemic meds and their side effects.
Cataract Surgery Special Considerations
Cataract surgery for those with uveitis autoimmune needs careful planning. It’s important to control inflammation before surgery to avoid problems. The choice of lens and when to do the surgery are also key.
After surgery, watch for signs of inflammation or issues. Use anti-inflammatory meds as needed.
Post-Surgical Care Requirements
Good post-surgical care is vital for success. This means regular check-ups, taking meds as told, and watching for any signs of trouble. Knowing about surgery and care helps patients make better choices.
Creating Your Healthcare Team
Building a healthcare team is key to managing autoimmune eye disease symptoms well. Autoimmune eye inflammation needs a team effort. This involves many medical specialists working together for the best results.
The Essential Role of Ophthalmologists
Ophthalmologists are vital in diagnosing and treating autoimmune eye disorders. They do detailed eye exams, find the right treatment, and make a plan for each patient.
Seeing an ophthalmologist often is important. It helps keep track of the condition, changes treatments if needed, and handles any problems.
Working Effectively with Rheumatologists
Rheumatologists play a big role in managing the whole body’s health when dealing with autoimmune disease eyesight issues. Working together, ophthalmologists and rheumatologists tackle both eye and body problems.
This team effort helps make treatment plans better. It might mean using less corticosteroids and avoiding long-term inflammation problems.
Additional Specialists to Consider
Other specialists might join the team based on the patient’s needs and health. These include:
- Primary care physicians, who manage overall health and coordinate care.
- Immunologists, who help with immune system treatments.
- Physical therapists, who help with movement and strength, like in arthritis.
Strategies for Coordinating Your Care
Good teamwork is essential for managing autoimmune eye disease symptoms. Here are some ways to do it:
- Keep a detailed medical history that everyone can see.
- Have regular meetings or consultations to talk about patient progress.
- Use patient portals or shared health records to keep everyone updated.
By working together and using a diverse team, patients with autoimmune eye inflammation can get better health and a better life.
Daily Management Strategies for Autoimmune Eye Inflammation
Living with autoimmune eye inflammation means you need to manage your eye health every day. To manage uveitis well, you need to treat it medically and make lifestyle changes.
Anti-Inflammatory Dietary Approaches
Your diet is key in fighting autoimmune eye inflammation. Eating foods that fight inflammation is important. Include fruits, vegetables, and omega-3 fatty acids in your diet.
Stay away from foods that can make inflammation worse. Avoid processed foods, sugary snacks, and foods with a lot of saturated fats. Adding anti-inflammatory herbs and spices like turmeric and ginger to your meals can also help.
Food Group | Beneficial Foods | Foods to Avoid |
Fruits | Berries, citrus fruits | Fruits high in sugar |
Vegetables | Leafy greens, cruciferous vegetables | Nightshades (for some individuals) |
Proteins | Fatty fish (rich in omega-3) | Processed meats |
Effective Stress Management Techniques
Stress can make autoimmune eye inflammation worse. So, managing stress is very important. Try meditation, deep breathing, and yoga to reduce stress.
“Mindfulness practices can significantly reduce the impact of stress on the body, promoting overall well-being and potentially reducing inflammation.” – Medical Expert, Stress Management Expert
Also, regular exercise, enough sleep, and hobbies can help manage stress.
Safe Exercise Recommendations
Exercise is good for your health, but choose safe activities if you have autoimmune eye inflammation. Low-impact exercises like walking, swimming, and cycling are best.
Always talk to your doctor before starting any new exercise, to make sure it’s safe for your eyes.
Optimizing Sleep for Eye Health
Good sleep is essential for eye health. Poor sleep can make inflammation worse and worsen uveitis symptoms. Try to sleep well by keeping a regular sleep schedule and creating a sleep-friendly environment.
- Avoid screens before bedtime
- Keep the bedroom cool and dark
- Avoid stimulating activities before bedtime
By following these daily strategies, you can better manage autoimmune eye inflammation and improve your life quality.
Conclusion
Managing autoimmune eye inflammation needs a team effort. We’ve looked at what causes it and how to treat it. Uveitis, a common eye disease, requires medical treatment, lifestyle changes, and a healthcare team.
Understanding uveitis helps people manage their treatment better. Treatment options include steroids, immunosuppressants, and biologics. A team of doctors, including eye and rheumatology specialists, is key to managing it.
Being proactive and informed can help those with autoimmune eye inflammation. It can reduce complications and improve life quality. A team effort is vital to support those with this condition effectively.
FAQ
What is autoimmune eye inflammation?
Autoimmune eye inflammation, also known as uveitis, is a serious condition. It happens when the immune system attacks the uvea, the middle layer of the eye. This leads to inflammation and can cause severe complications.
What are the different types of uveitis?
There are several types of uveitis. These include anterior, intermediate, posterior, and panuveitis. Each type affects different parts of the uvea and needs a specific treatment.
What are the common symptoms of autoimmune eye inflammation?
Symptoms can include eye pain, redness, sensitivity to light, blurred vision, and floaters. These symptoms vary based on the type and severity of the condition.
How is autoimmune eye inflammation diagnosed?
Diagnosis involves a detailed eye examination. It also includes laboratory tests to find underlying autoimmune diseases. Advanced imaging studies like optical coherence tomography (OCT) help assess the inflammation.
What are the treatment options for autoimmune eye inflammation?
Treatment options include corticosteroid therapy and immunosuppressive medication. Biologic agents and surgical interventions like vitrectomy or implantable steroid devices may also be used in severe cases.
Can lifestyle changes help manage autoimmune eye inflammation?
Yes, making lifestyle changes can help. Adopting an anti-inflammatory diet, managing stress, exercising safely, and getting enough sleep can support eye health and overall well-being.
What is the role of ophthalmologists and rheumatologists in managing autoimmune eye inflammation?
Ophthalmologists are key in diagnosing and treating uveitis. Rheumatologists help manage underlying autoimmune diseases. Working together, they provide essential care.
Are there any specific autoimmune diseases associated with eye inflammation?
Yes, certain autoimmune diseases increase the risk of uveitis. These include rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, and sarcoidosis.
What are the potentially serious complications of untreated autoimmune eye inflammation?
Untreated uveitis can lead to serious complications. These include vision loss, cataract formation, glaucoma, and retinal detachment. Prompt and effective management is critical.
How can I coordinate my care for autoimmune eye inflammation?
Coordinating care involves working with a team of healthcare professionals. This includes ophthalmologists, rheumatologists, and other specialists. Together, they create a treatment plan tailored to your needs.
References
National Center for Biotechnology Information. Managing Autoimmune Uveitis: Preventing Vision Loss. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16182531/