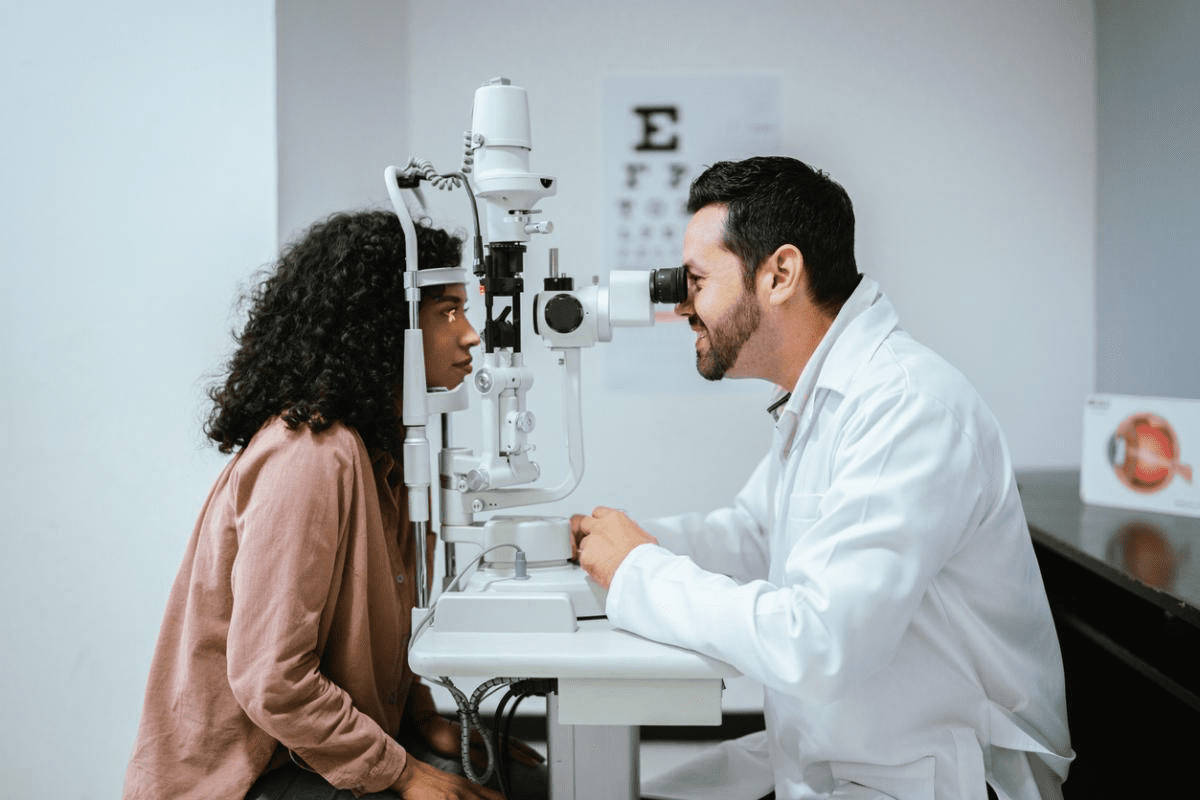
Your eyes are not just windows to the world; they are also indicators of your overall health. Autoimmune eye disorders happen when your body’s immune system attacks your eye tissues. This leads to various conditions that can harm your vision and eye health.Learn the 7 critical warning signs of autoimmune eye problems. Discover the causes and essential treatments you need to know now.
More than 80 types of autoimmune diseases can affect your eyes. These conditions can cause eye discomfort, inflammation, and even serious damage to the optic nerve, retina, and surrounding areas.
At Liv Hospital, we offer top-notch ophthalmology care and patient-focused treatment for autoimmune eye conditions. Our team is committed to giving you the best support and advanced medical treatments as an international patient.
Key Takeaways
- Autoimmune eye disorders are caused by the body’s immune system attacking eye tissues.
- Over 80 types of autoimmune diseases can affect the eyes.
- These conditions can lead to discomfort, inflammation, and vision-threatening damage.
- Liv Hospital offers world-class ophthalmology care for autoimmune eye conditions.
- Our team provides patient-centered care and advanced medical treatments.
What Are Autoimmune Eye Problems?
Autoimmune eye diseases are when the immune system attacks the eyes by mistake. This leads to vision problems. These diseases can harm different parts of the eye, causing various symptoms.
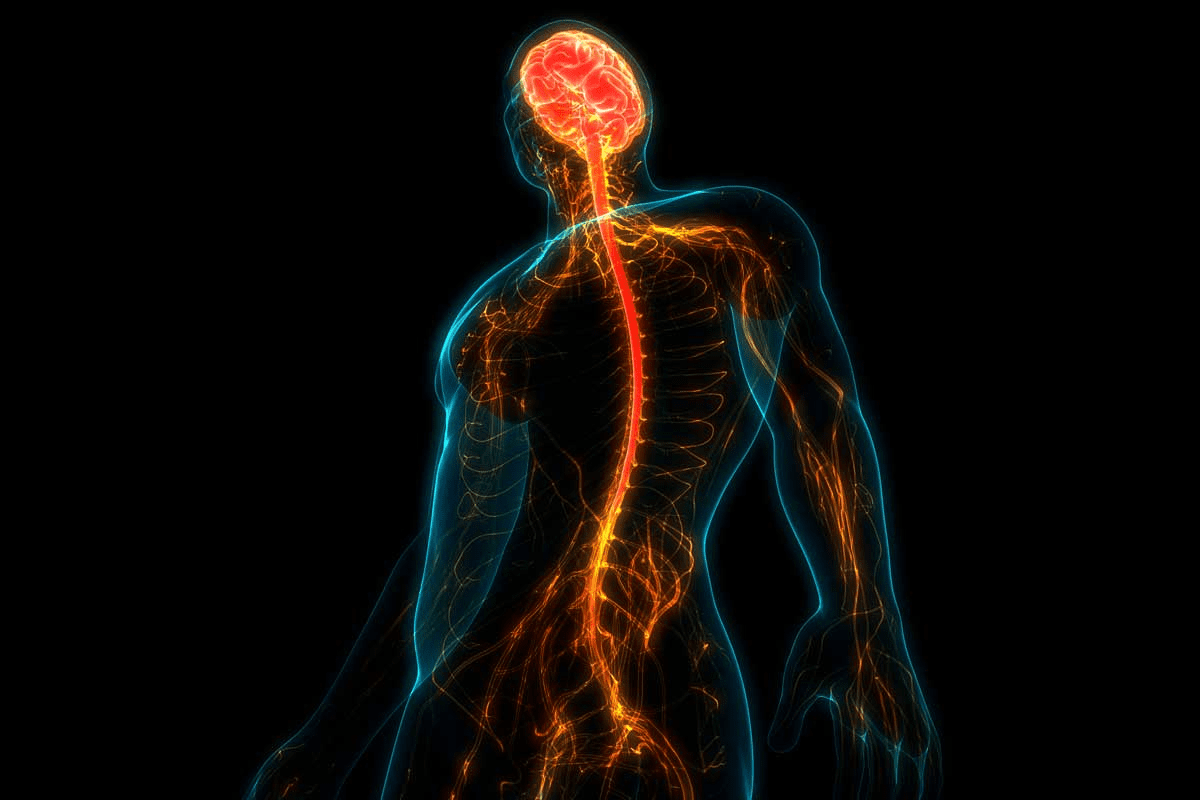
The Immune System’s Role in Eye Health
The immune system is key to keeping our eyes healthy. It fights off infections and diseases. But in autoimmune diseases, it attacks the eyes by mistake, causing inflammation and damage.
Key aspects of the immune system’s role in eye health include:
- Protecting the eyes from pathogens
- Regulating inflammation to prevent tissue damage
- Maintaining the integrity of eye tissues
When the immune system gets confused, it can cause autoimmune eye diseases like uveitis and scleritis. Knowing how this works is key to treating these diseases.
Statistics and Prevalence of Autoimmune Eye Disorders
Autoimmune eye diseases are a big cause of vision loss worldwide. Studies show that dry eye disease is very common, affecting millions globally.
Some key statistics on autoimmune eye disorders include:
- Dry eye disease affects about 30 million people in the United States.
- Uveitis causes about 10% of blindness in the United States.
- Conditions like rheumatoid arthritis and lupus raise the risk of eye problems.
These numbers show why we need to be aware of autoimmune eye diseases. Proper management can prevent vision loss and improve life for those affected.
Common Symptoms of Autoimmune Eye Problems

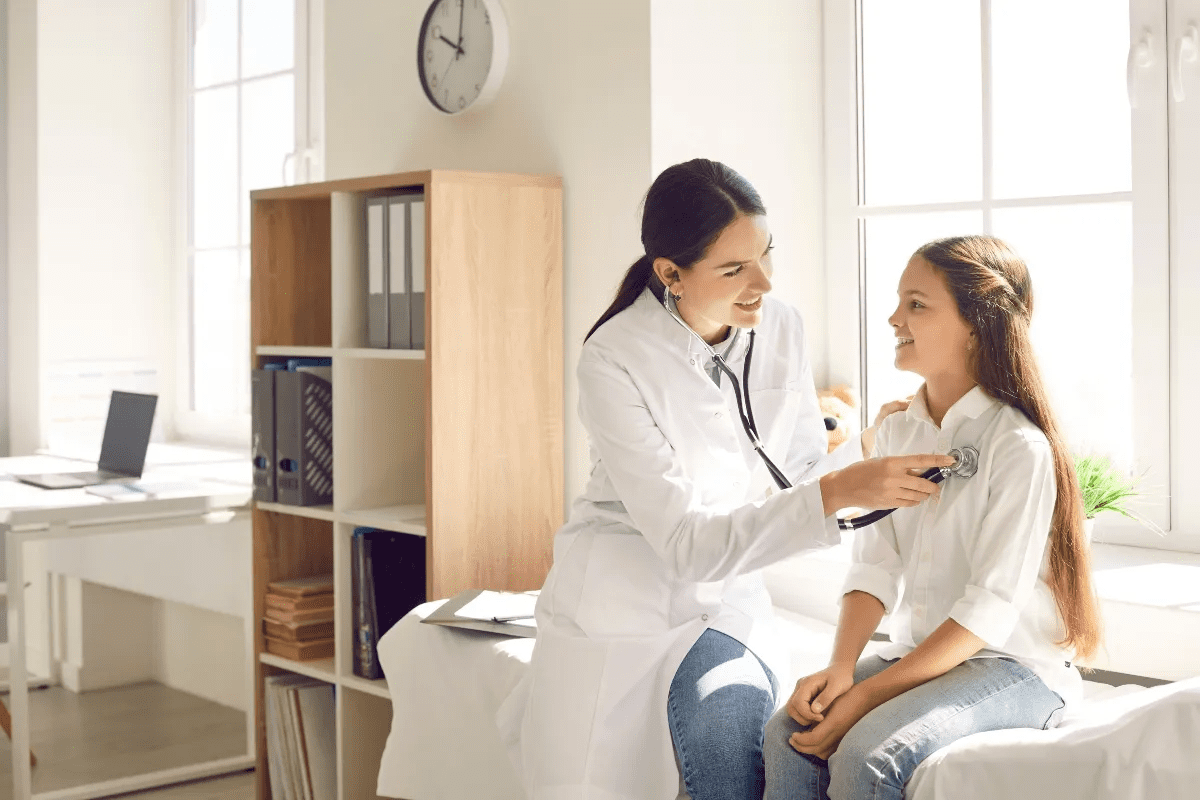
It’s important to know the signs of autoimmune eye problems early. These diseases can cause eye pain and vision issues. We’ll talk about the early signs and when to see a doctor.
Early Warning Signs to Watch For
Autoimmune eye diseases show different symptoms. These include dry or red eyes, feeling like something is in your eye, and sensitivity to light. They can even cause permanent vision loss. Look out for these signs:
- Dryness or irritation that doesn’t go away with eye drops.
- Redness or inflammation without a clear reason.
- Sensitivity to light (photophobia) or trouble in bright places.
- Eye pain or discomfort, worse when moving your eyes.
- Blurred vision or changes in how well you can see.
When to Seek Medical Attention
If you notice any of these symptoms, see a doctor right away. Early treatment can make a big difference. If you have:
- Staying symptoms or they get worse, despite trying treatments.
- Big changes in your vision or eye comfort.
- Symptoms that match other autoimmune diseases.
Acting fast can help manage symptoms and keep your vision. Understanding autoimmune eye problems and their treatments is key.
“Early detection and treatment of autoimmune eye diseases are key to keeping your vision and improving your life.”
— American Academy of Ophthalmology
1. Uveitis: Inflammation of the Eye’s Middle Layer
Uveitis is a serious eye condition that affects the middle layer of the eye. This layer, called the uvea, is key to the eye’s function. If it gets inflamed, it can cause serious vision problems.
Types of Uveitis
Uveitis is divided into types based on where in the uvea it occurs:
- Anterior Uveitis: This type affects the front part of the uvea, often linked to autoimmune diseases.
- Intermediate Uveitis: It impacts the ciliary body and the vitreous humor.
- Posterior Uveitis: This type affects the back part of the uvea, leading to serious vision issues.
- Panuveitis: It involves inflammation of all layers of the uvea.
Connection to Systemic Autoimmune Diseases
Uveitis is often connected to other autoimmune diseases. It happens in about 25 percent of people with ankylosing spondylitis and up to 37 percent with Reiter’s syndrome. Knowing this helps doctors care for patients better.
Autoimmune Disease | Prevalence of Uveitis |
Ankylosing Spondylitis | 25% |
Reiter’s Syndrome | Up to 37% |
Treatment Options and Prognosis
Treatment for uveitis aims to reduce inflammation and pain. It includes:
- Corticosteroids to lower inflammation.
- Immunosuppressive drugs for severe cases.
- Biologic agents targeting specific inflammatory pathways.
The outcome depends on the type and severity of uveitis, and the underlying disease. Early treatment is key to avoiding permanent vision loss.
2. Dry Eye Disease: Beyond Simple Irritation
Dry eye disease is more than just irritation. It often links with autoimmune diseases. It affects millions, causing discomfort and vision problems. We’ll look at its ties to diseases like Sjögren’s syndrome and rheumatoid arthritis, and how to manage it.
Sjögren’s Syndrome and Its Impact on Tear Production
Sjögren’s syndrome is a chronic autoimmune disease. It affects the glands that make tears and saliva. About 95% of people with Sjögren’s have dry eyes because they make fewer tears.
The inflammation from Sjögren’s damages the tear glands. This makes it hard for people with Sjögren’s to make tears. They often need a lot of help to manage their dry eye symptoms.
Rheumatoid Arthritis and Lupus-Related Dry Eye
Rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE or lupus) can also cause dry eyes. Studies show that 38-47% of people with RA have dry eye disease.
The inflammation from these diseases can hurt the eyes. This reduces tear production and causes dry eye symptoms. It’s important to manage these diseases to help with dry eye.
Management Strategies and Treatments
Managing dry eye disease requires a few steps. This includes changing your lifestyle, using medications, and sometimes procedures. Artificial tears and anti-inflammatory eye drops are common treatments.
For cases linked to autoimmune diseases, treating the disease itself is key. This might involve medicines to reduce inflammation and disease activity. This helps to ease dry eye symptoms.
3. Scleritis: Inflammation of the Eye’s Protective Outer Layer
Scleritis is an inflammatory condition of the sclera. It’s often linked to autoimmune diseases and can cause severe eye damage if not treated. The sclera protects the eye’s internal structures. When it gets inflamed, it can lead to discomfort and vision problems.
Differentiating Between Types of Scleritis
Scleritis can be classified into different types. These depend on the area of the sclera affected and the inflammation’s severity. The main types include:
- Anterior Scleritis: This is the most common form. It’s further divided into non-necrotizing and necrotizing types, with the latter being more severe.
- Posterior Scleritis: This type affects the back of the sclera. It can be harder to diagnose because of its location.
Associated Autoimmune Conditions
Scleritis is often linked to various autoimmune diseases. These include:
- Rheumatoid Arthritis: A common autoimmune condition that can lead to scleritis.
- Lupus: Systemic lupus erythematosus can also cause scleritis among its many symptoms.
- Wegener’s Granulomatosis: Now known as Granulomatosis with Polyangiitis, this condition can cause scleritis.
Experts say, “The association between scleritis and systemic autoimmune diseases highlights the need for a detailed diagnostic approach.” This emphasizes the importance of a multidisciplinary evaluation for effective management of scleritis.
Treatment Approaches and Complications
Treatment for scleritis focuses on addressing the underlying cause and reducing inflammation. Approaches include:
- Oral NSAIDs or corticosteroids to reduce inflammation.
- Immunosuppressive therapy for cases associated with autoimmune diseases.
- Surgical intervention in severe cases or to address complications.
If left untreated, scleritis can lead to serious complications. These include perforation of the globe or vision loss. So, prompt and effective treatment is key.
4. Optic Neuritis: When Autoimmunity Attacks the Optic Nerve
The optic nerve is key for our vision. Optic neuritis, an inflammatory condition, can harm it. This shows how the immune system and eye health are connected.
Multiple Sclerosis and Optic Neuritis Relationship
Optic neuritis is closely tied to multiple sclerosis (MS), a chronic autoimmune disease. Many with optic neuritis will get MS. “The presence of optic neuritis often indicates a high risk of developing multiple sclerosis,” says recent research. We’ll dive deeper into this connection and its effects on patients.
Symptoms and Diagnostic Methods
Symptoms of optic neuritis include sudden vision loss and eye pain. A detailed eye exam, visual field tests, and MRI scans are used to diagnose it. These help check the optic nerve and rule out other issues.
Diagnostic Approaches:
- Visual acuity testing
- Visual field testing
- MRI scans
- Ophthalmoscopy
Treatment Protocols and Vision Prognosis
Treatment for optic neuritis often includes corticosteroids to reduce inflammation. In some cases, IVIG or plasma exchange may be used. The chance of vision recovery varies. Many see big improvements, but some may face lasting vision problems.
Dr. [Last Name] says, “Early treatment is key for better outcomes in optic neuritis. It shows the need for quick medical care.”
Dealing with optic neuritis and its link to MS can be tough. Our team is dedicated to giving full care and support to those facing these challenges.
5. Thyroid Eye Disease: Graves’ Disease and Ocular Manifestations
Thyroid eye disease shows how thyroid health affects our eyes. It’s common in people with Graves’ disease. This condition affects the tissues around the eye, like the eyelids and lacrimal gland.
Pathophysiology and Autoimmune Mechanism
Thyroid eye disease happens when immune cells attack the orbital tissues. This leads to swelling and inflammation. The swelling can push the eyes out, causing exophthalmos.
The disease is caused by autoantibodies targeting the thyroid and orbital tissues. These autoantibodies activate immune cells and release inflammatory cytokines.
Clinical Presentation and Progression
Thyroid eye disease shows different symptoms in different people. Symptoms include bulging eyes, redness, and swelling. In severe cases, it can cause vision loss.
The disease can progress unpredictably. Some people have mild symptoms, while others face severe issues.
Medical and Surgical Management Options
Managing thyroid eye disease requires a team effort. Doctors, endocrinologists, and ophthalmologists work together. Medical management uses corticosteroids and immunosuppressive therapy.
In severe cases, surgical intervention is needed. This can include orbital decompression surgery to treat exophthalmos.
Up to 50 percent of Graves’ disease patients get thyroid eye disease. Knowing how to treat it is key. Healthcare providers can offer better care by understanding the disease well.
6. Retinal Vasculitis: Blood Vessel Inflammation in Behçet’s Disease
Behçet’s disease and retinal vasculitis have a complex relationship. This condition affects about 70 percent of patients with eye symptoms. It’s important to understand and manage it well.
Understanding Behçet’s Disease and Eye Involvement
Behçet’s disease is a complex autoimmune disorder. It can affect many parts of the body, including the eyes. Retinal vasculitis is a serious eye problem that can lead to vision loss if not treated.
- Ocular inflammation is a hallmark of Behçet’s disease, often presenting as retinal vasculitis.
- The condition can lead to significant visual impairment if not promptly treated.
- Understanding the autoimmune mechanisms behind Behçet’s disease is key for effective management.
Diagnostic Challenges and Approaches
Diagnosing retinal vasculitis in Behçet’s disease is challenging. We use clinical evaluation, imaging studies, and lab tests to diagnose. Fluorescein angiography is a key tool for assessing retinal vascular involvement.
- Clinical examination to identify signs of uveitis or retinal vasculitis.
- Imaging techniques such as fluorescein angiography and optical coherence tomography (OCT).
- Laboratory tests to rule out other causes of retinal vasculitis.
Treatment Strategies and Visual Outcomes
Treating retinal vasculitis in Behçet’s disease requires a multi-faceted approach. We use corticosteroids and immunosuppressive agents as first-line treatments. Biologic therapies are also emerging as valuable options for refractory cases.
- Corticosteroids to rapidly control inflammation.
- Immunosuppressive drugs to maintain long-term control.
- Biologic agents for patients who do not respond to conventional therapy.
By understanding the complexities of retinal vasculitis in Behçet’s disease and using a detailed treatment plan, we can improve visual outcomes and quality of life for affected patients.
7. Episcleritis: Inflammation of the Episcleral Tissue
The episclera is a layer between the sclera and conjunctiva. It can get inflamed, causing episcleritis. This condition has its own symptoms and is linked to autoimmune diseases.
Distinguishing from Scleritis and Other Eye Conditions
Episcleritis is often mixed up with scleritis, a more serious condition. But, episcleritis has milder symptoms and doesn’t go as deep into the eye. The main differences are:
- Mild to moderate eye discomfort
- Redness and inflammation
- Possible nodules or areas of inflammation
Scleritis, on the other hand, can cause more pain, vision issues, and serious problems. Getting a correct diagnosis from an eye doctor is very important.
Connection to Rheumatoid Arthritis and Other Autoimmune Diseases
Rheumatoid arthritis is linked to episcleritis. Lupus and gout can also be connected. The inflammation in episcleritis might show the body’s fight against itself.
Treatment Options and Recurrence Management
Managing episcleritis often includes:
- Topical corticosteroids to reduce inflammation
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief
- Treatment of the underlying autoimmune condition, if present
When it’s tied to rheumatoid arthritis or other autoimmune diseases, treating the whole body is key. It can come back, so regular check-ups with an eye specialist are a must.
Dealing with episcleritis is tough, but knowing about it and its ties to other diseases helps. This way, we can take better care of our eye health.
Diagnosis and Treatment Approaches for Autoimmune Eye Problems
Autoimmune eye diseases need a detailed diagnostic process. This process involves insights from different medical fields. Accurate diagnosis is key to creating an effective treatment plan.
The Multidisciplinary Diagnostic Process
Diagnosing autoimmune eye problems requires a thorough evaluation. This includes looking at the patient’s history, physical exam, and specialized tests. A team of doctors, like ophthalmologists and rheumatologists, work together to diagnose these complex conditions.
The diagnostic process typically involves:
- Detailed patient history to identify symptoms and triggers
- Comprehensive eye examination to assess visual acuity and eye health
- Imaging tests such as optical coherence tomography (OCT) or fluorescein angiography
- Laboratory tests to detect inflammatory markers or autoimmune antibodies
Diagnostic Test | Purpose |
Optical Coherence Tomography (OCT) | High-resolution imaging of retinal layers |
Fluorescein Angiography | Assessment of retinal vasculature and leakage |
Blood Tests for Inflammatory Markers | Detection of systemic inflammation |
Conventional Treatments: Corticosteroids and Immunosuppressants
Conventional treatments for autoimmune eye diseases include corticosteroids and immunosuppressants. Corticosteroids help reduce inflammation but can have side effects with long-term use.
“Corticosteroids remain a cornerstone in the treatment of autoimmune eye diseases, providing rapid control of inflammation. But, their long-term use is limited by side effects.”
Immunosuppressants are used to lower the dose of corticosteroids needed. They help manage chronic inflammation. Common immunosuppressants include methotrexate, azathioprine, and cyclosporine.
Emerging Therapies: Biologics and Targeted Treatments
Biologic therapies have changed how we treat autoimmune eye diseases. Biologics like TNF-alpha inhibitors and interleukin inhibitors target inflammation directly.
These therapies show promise in reducing inflammation and improving patient outcomes. Ongoing research aims to find new targets and strategies for treatment.
Living With Autoimmune Eye Conditions: Lifestyle Considerations
Living with autoimmune eye conditions can be tough. But, making lifestyle changes can really help. It’s not just about medical treatment. It’s also about daily habits and choices.
Diet and Nutrition Impact on Symptoms
Eating right is key to managing these conditions. Nutrients like omega-3s, vitamins A, C, and E, and antioxidants fight inflammation and keep eyes healthy. Foods full of these include leafy greens, fatty fish, nuts, and seeds.
Adding anti-inflammatory foods to your diet can ease symptoms. For example, turmeric has curcumin, which fights inflammation. Ginger also helps reduce inflammation and boosts health.
Stress Management and Eye Health
Stress can make autoimmune eye conditions worse. So, managing stress is important for eye health. Meditation, yoga, and deep breathing can help lower stress. Exercise is also key for stress relief and overall health.
Getting good sleep is also critical. Poor sleep can make stress and symptoms worse. A calm bedtime routine and avoiding screens before bed can help you sleep better.
Support Resources and Patient Communities
Dealing with an autoimmune eye condition can feel lonely. But, connecting with others who understand can offer support and advice. Joining patient support groups, online or in-person, is very helpful.
Also, using resources from organizations focused on autoimmune diseases and eye health is valuable. These groups share the latest treatments and lifestyle tips.
Conclusion
We’ve looked at many autoimmune eye problems, like uveitis and dry eye disease. We also talked about scleritis, optic neuritis, and thyroid eye disease. These issues show how the immune system can affect our eyes.
It’s important to know the symptoms, causes, and treatments for these eye diseases. Getting the right diagnosis and treatment can really help people live better lives.
Diagnosing and treating these conditions often needs a team effort. Doctors use things like corticosteroids and new treatments like biologics. This helps manage the diseases better.
In short, dealing with autoimmune eye problems needs a careful and detailed approach. By understanding these issues, we can help those who are affected.
FAQ
What are autoimmune eye problems?
Autoimmune eye problems happen when the immune system attacks the eyes by mistake. This leads to inflammation and damage. These issues can be linked to various autoimmune diseases that affect the eyes.
What are the common symptoms of autoimmune eye problems?
Symptoms include redness, pain, and blurred vision. You might also feel dryness, sensitivity to light, and see floaters. Early signs can be mild discomfort or irritation, which can get worse if not treated.
What is uveitis, and how is it related to autoimmune diseases?
Uveitis is inflammation in the eye’s middle layer. It can be caused by diseases like ankylosing spondylitis and Reiter’s syndrome. Treatment includes corticosteroids and immunosuppressants to fight inflammation and protect vision.
How does dry eye disease relate to autoimmune conditions like Sjögren’s syndrome?
Dry eye disease often goes hand in hand with Sjögren’s syndrome. This autoimmune condition affects tear production. Treatment includes artificial tears, punctal plugs, and medications to boost tear production.
What is scleritis, and how is it treated?
Scleritis is inflammation of the eye’s outer layer. It can be caused by diseases like rheumatoid arthritis. Treatment involves NSAIDs, corticosteroids, and immunosuppressants to reduce inflammation and prevent complications.
What is the relationship between optic neuritis and multiple sclerosis?
Optic neuritis is inflammation of the optic nerve. It can be a sign of multiple sclerosis. Treatment includes corticosteroids to reduce inflammation. The vision prognosis depends on the underlying condition.
How is thyroid eye disease related to Graves’ disease?
Thyroid eye disease is linked to Graves’ disease, a thyroid disorder. Management includes medications to reduce inflammation. Surgery, like orbital decompression, may also be needed to alleviate symptoms.
What is retinal vasculitis, and how is it connected to Behçet’s disease?
Retinal vasculitis is inflammation of the retina’s blood vessels. It can be caused by Behçet’s disease, a rare autoimmune disorder. Treatment includes corticosteroids, immunosuppressants, and biologics to fight inflammation and prevent vision loss.
How is episcleritis different from scleritis?
Episcleritis is inflammation of the episcleral tissue, a layer on top of the sclera. It’s usually less severe than scleritis. Treatment includes NSAIDs or corticosteroids. Managing recurrence involves monitoring and adjusting treatment as needed.
What lifestyle changes can help manage autoimmune eye conditions?
Making lifestyle changes can help. Eat a balanced diet, manage stress, and exercise regularly. Support groups and patient communities offer valuable guidance and connection.
What are the emerging treatment approaches for autoimmune eye problems?
New treatments include biologics and targeted therapies. They aim to reduce inflammation and control the immune system. These treatments offer hope for patients with autoimmune eye conditions.
How are autoimmune eye problems diagnosed?
Diagnosis involves a team effort. It includes clinical exams, imaging tests, and lab tests to find underlying conditions. A thorough diagnostic process is key for effective treatment.
References
National Center for Biotechnology Information. Autoimmune Eye Disorders: Symptoms, Causes, and Treatment. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8593335/