Autoimmune eye swelling, often seen as uveitis, is a big problem for eye health worldwide. It leads to about 30,000 new cases of legal blindness each year in the U.S.Our ultimate guide to autoimmune eye swelling reveals the top causes and proven strategies for effective management and relief.
Understanding this condition is key to managing it well. We’ll look at what causes it, its symptoms, and how to treat it. This guide is for patients and anyone looking for health information.
Key Takeaways
- Autoimmune eye swelling can lead to severe vision impairment if left untreated.
- Uveitis is a common manifestation of autoimmune eye disease.
- Early diagnosis and treatment are critical for preventing long-term damage.
- Liv Hospital’s patient-centered approach combines cutting-edge medical protocols with compassionate care.
- Effective management strategies can significantly improve patient outcomes.
Understanding Autoimmune Eye Swelling
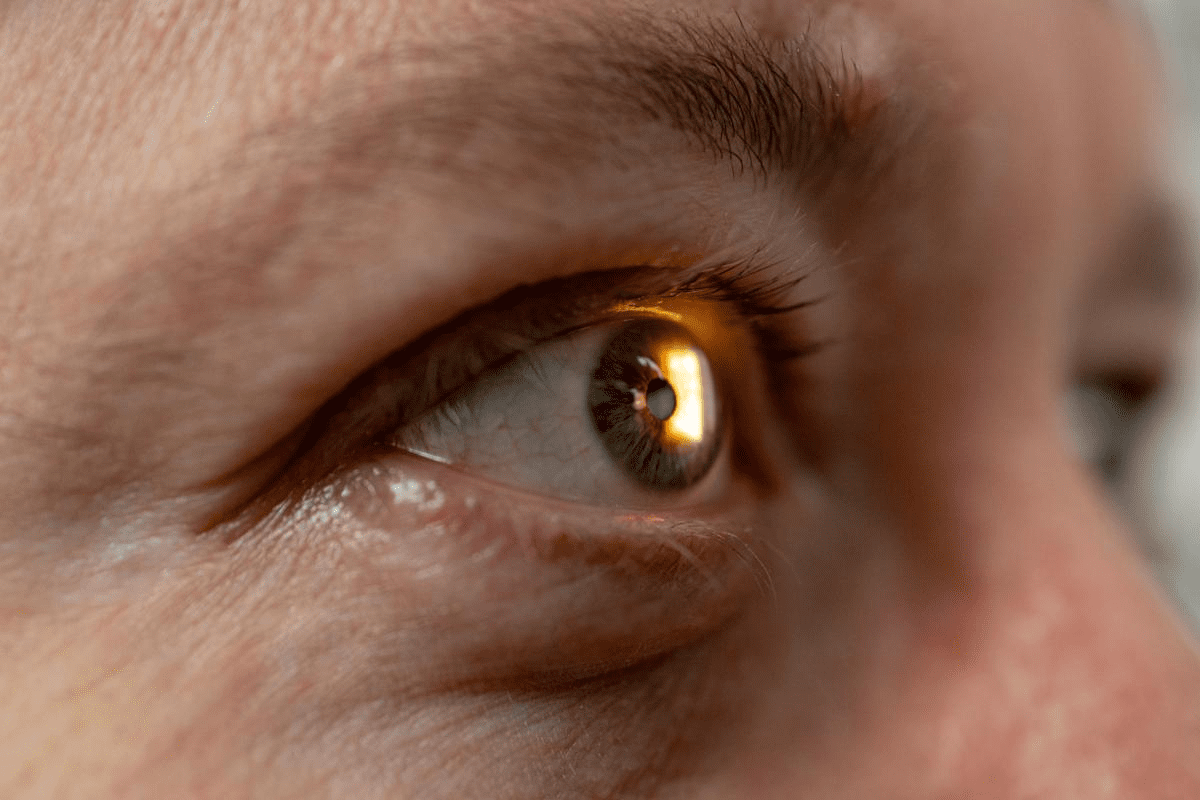
It’s important to know why autoimmune eye swelling happens. This condition occurs when the immune system mistakenly attacks healthy eye tissue. It mainly affects the uvea.
What Causes Autoimmune Eye Inflammation
Autoimmune eye inflammation is caused by a mix of genetic and environmental factors. In autoimmune diseases, the immune system can’t tell the difference between self and non-self. This leads to an attack on the body’s own tissues.
The exact reasons for autoimmune eye inflammation are not fully known. But research shows that genetics, infections, and environmental triggers are key.
Key factors contributing to autoimmune eye inflammation include:
- Genetic predisposition
- Infections that trigger autoimmune responses
- Environmental factors such as exposure to certain chemicals or toxins
The Role of the Immune System in Eye Health
The immune system protects the eyes from infections and foreign invaders. But in autoimmune conditions, it attacks the eye tissues instead. This leads to inflammation and damage.
A balance is needed between immune protection and tolerance. In autoimmune eye diseases, this balance is lost. This can cause inflammation and vision loss if not treated.
Common Types of Autoimmune Eye Conditions
Several autoimmune conditions can affect the eyes. Uveitis, scleritis, and orbital inflammatory disease are examples. Uveitis is the most common, affecting the uvea, the middle layer of the eye.
Scleritis involves inflammation of the sclera, the white outer layer of the eye. Each condition needs specific treatment to prevent complications and save vision.
Common autoimmune eye conditions include:
- Uveitis
- Scleritis
- Orbital inflammatory disease
Recognizing the Signs and Symptoms
Spotting early signs of autoimmune eye inflammation is key to better treatment. Autoimmune eye diseases can cause eye discomfort and vision issues if not treated.
Early Warning Signs of Eye Inflammation
The first signs of autoimmune eye inflammation can be subtle. They often include redness, pain, and light sensitivity. Eye inflammation can also lead to blurred vision and discomfort, which can get worse if not treated.
Some people might feel their eyes are dry or gritty. This could be a sign of an autoimmune eye condition. It’s important to watch for these signs and see an eye doctor if they don’t go away or get worse.
Progression of Symptoms
As autoimmune eye disease gets worse, symptoms can get more severe. They might include:
- Severe eye pain
- Increased sensitivity to light
- Vision disturbances, such as blurred vision or double vision
- Redness and swelling of the eyes
Autoimmune eye conditions can lead to serious problems like uveitis, scleritis, or vision loss if not treated. Catching it early and treating it quickly is key to avoiding long-term damage.
“The key to managing autoimmune eye disease is early detection and treatment. By recognizing the signs and symptoms early, patients can receive timely interventions that significantly improve outcomes.”
Medical Expert, Ophthalmologist
Differentiating from Other Eye Conditions
It can be hard to tell autoimmune eye conditions from other eye diseases because symptoms can be similar. But, autoimmune eye diseases often have systemic symptoms or are linked to known autoimmune disorders.
Condition | Common Symptoms | Autoimmune Association |
Uveitis | Eye pain, sensitivity to light, blurred vision | Often associated with rheumatoid arthritis and other autoimmune diseases |
Scleritis | Severe eye pain, redness, sensitivity to light | Commonly linked with rheumatoid arthritis and lupus |
Dry Eye Syndrome | Dryness, grittiness, blurred vision | Can be associated with Sjögren’s syndrome, an autoimmune disorder |
Knowing the differences is important for accurate diagnosis and treatment. If you have persistent or severe eye symptoms, seeing an eye care professional is vital. They can give a thorough check-up and the right care.
The Connection Between Systemic Autoimmune Diseases and Eye Health
Autoimmune diseases can harm the eyes. These diseases happen when the body attacks its own tissues. This leads to inflammation and damage in the eyes and other parts of the body.
It’s important to know how these diseases affect the eyes. We’ll look at how rheumatoid arthritis, lupus, and autoimmune thyroid disease impact eye health.
Rheumatoid Arthritis and Ocular Manifestations
Rheumatoid arthritis (RA) mainly affects the joints but can also harm the eyes. Up to 25% of RA patients may face eye problems, like dry eye, scleritis, and uveitis.
Dry eye is common in RA patients. It happens when the lacrimal gland gets inflamed and doesn’t produce enough tears. Scleritis, an inflammation of the sclera, can cause severe pain and serious complications if not treated quickly.
Lupus and Its Effects on Vision
Systemic lupus erythematosus (SLE) can severely affect the eyes. Ocular manifestations occur in up to one-third of SLE patients and can range from mild dry eye to severe retinal vasculitis.
Lupus can cause various eye problems, including:
- Dry eye syndrome
- Retinal vasculitis
- Optic neuritis
- Secondary Sjögren’s syndrome
Autoimmune Thyroid Disease and Eye Complications
Autoimmune thyroid disease, like Graves’ disease, can cause eye problems. Graves’ orbitopathy is a condition characterized by inflammation and swelling of the tissues around the eye, including the eyelids, eye socket, and lacrimal gland.
Autoimmune Disease | Ocular Manifestations | Prevalence |
Rheumatoid Arthritis | Dry eye, scleritis, uveitis | Up to 25% |
Systemic Lupus Erythematosus | Dry eye, retinal vasculitis, optic neuritis | Up to 33% |
Autoimmune Thyroid Disease (Graves’) | Graves’ orbitopathy, exophthalmos, diplopia | Varies |
Understanding the link between systemic autoimmune diseases and eye health is key. By recognizing the eye problems these diseases can cause, healthcare providers can help patients. This helps preserve vision and improve their quality of life.
Uveitis: A Common Form of Autoimmune Eye Swelling
Understanding uveitis is key to managing this serious eye condition. It’s an autoimmune disease that can harm your sight if not treated right. Uveitis affects the uvea, the eye’s middle layer, and can cause serious problems if not treated.
Types of Uveitis
There are different types of uveitis, each with its own causes and symptoms. The main types are:
- Anterior Uveitis: This type affects the front part of the uvea. It’s often linked to autoimmune diseases like ankylosing spondylitis.
- Intermediate Uveitis: This type affects the middle part of the uvea. It’s sometimes caused by conditions like multiple sclerosis.
- Posterior Uveitis: This type affects the back part of the uvea. It can be caused by infections or autoimmune diseases.
- Panuveitis: This is the most severe type. It affects all layers of the uvea, making it a serious condition.
Risk Factors for Developing Uveitis
Some factors can increase your risk of getting uveitis. These include:
- Autoimmune Diseases: Conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease can raise your risk.
- Genetic Predisposition: If your family has a history of autoimmune diseases, you might be more at risk.
- Infections: Some infections can trigger uveitis in certain cases.
- Eye Trauma: Injury to the eye can sometimes lead to uveitis.
Potential Complications if Left Untreated
If uveitis isn’t treated, it can lead to serious problems. These include:
- Vision Loss: Long-term inflammation can cause permanent eye damage.
- Cataract Formation: Uveitis can increase your risk of getting cataracts.
- Glaucoma: Inflammation can raise the pressure inside your eye.
- Retinal Detachment: Severe inflammation can cause the retina to detach from the eye’s back.
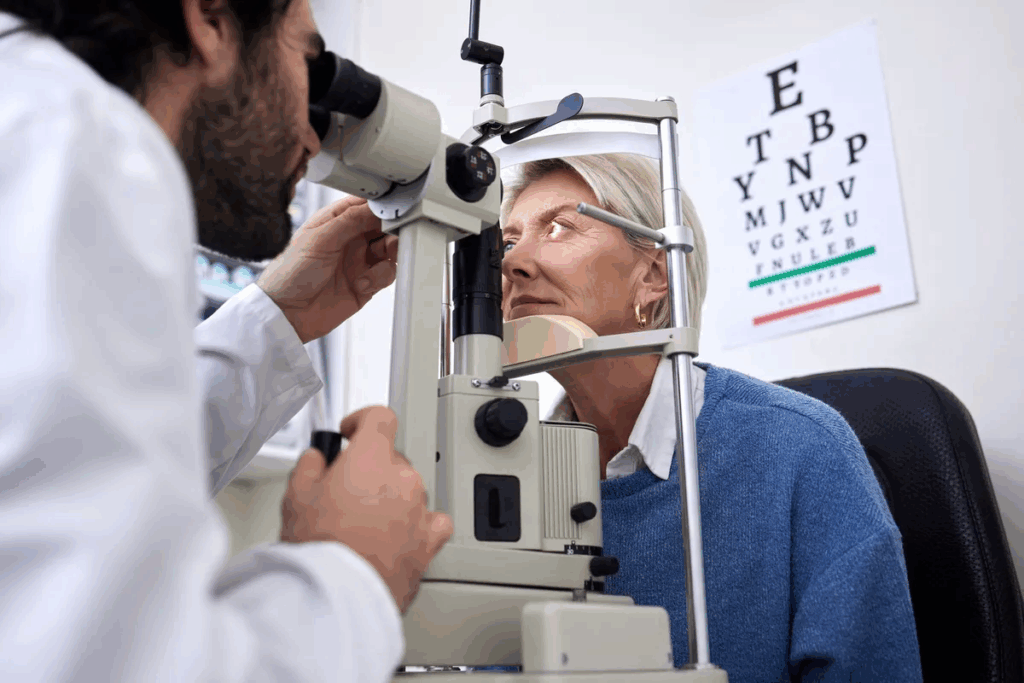
Getting early treatment is vital to avoid these complications and keep your vision. We suggest seeing an ophthalmologist or a specialist in autoimmune diseases for the best care.
Diagnostic Process for Autoimmune Eye Conditions
Understanding how to diagnose autoimmune eye conditions is key to managing them well. This process involves several steps to find the cause and how far the disease has spread.
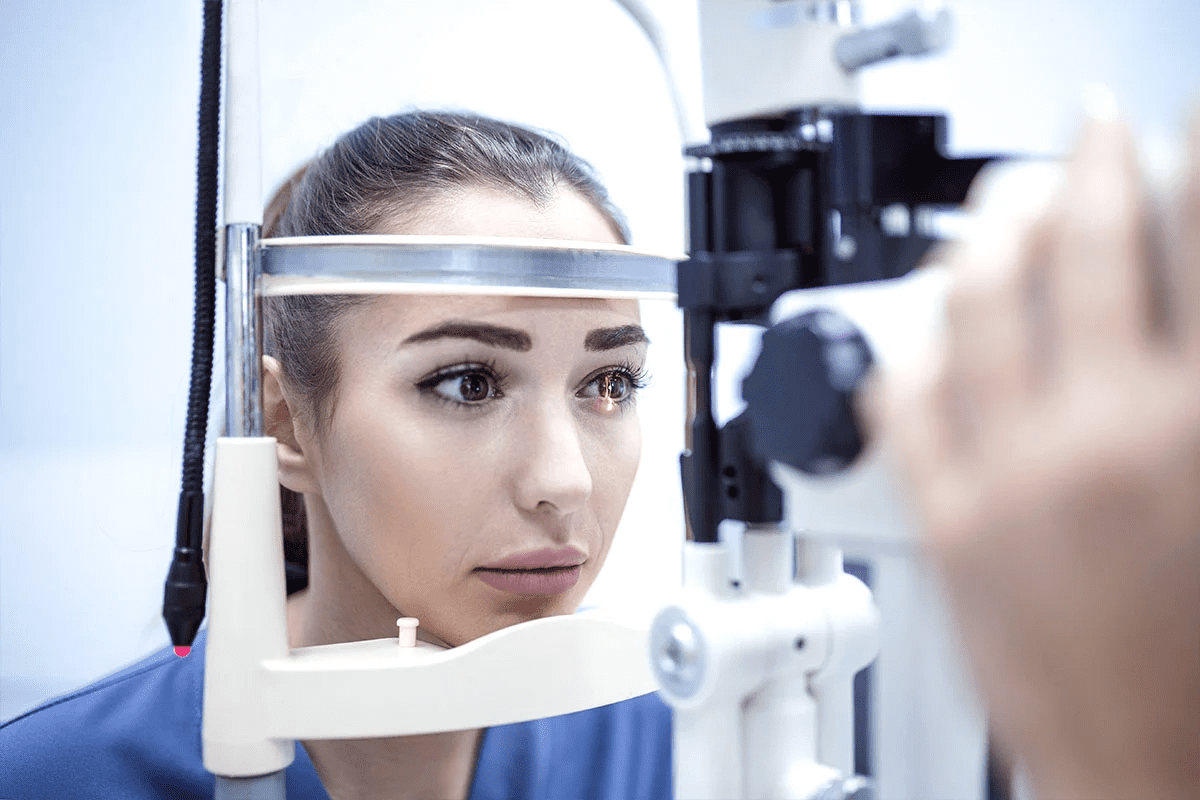
Initial Eye Examination
The first step is a detailed eye check. An ophthalmologist looks for signs of inflammation or swelling in the eyes. They use tests like visual acuity and slit-lamp exams to see how the eyes are doing.
Laboratory Tests and Imaging
After the eye check, more tests are done. Blood tests look for signs of autoimmune activity. Imaging like OCT or fluorescein angiography gives detailed eye pictures, helping to pinpoint the condition.
Some lab tests include:
- Complete Blood Count (CBC) to check for inflammation or infection
- Erythrocyte Sedimentation Rate (ESR) or C-Reactive Protein (CRP) to measure inflammation
- Tests for specific autoantibodies linked to autoimmune diseases
Working with Specialists: Ophthalmologists and Rheumatologists
Diagnosing and treating autoimmune eye conditions often needs teamwork. Ophthalmologists focus on eye disorders, while rheumatologists know about autoimmune diseases. Together, they understand the condition fully and create a treatment plan.
Specialist | Role in Diagnosis | Role in Treatment |
Ophthalmologist | Does eye exams and finds eye-related problems | Takes care of eye symptoms and issues |
Rheumatologist | Finds systemic autoimmune diseases | Treats the main autoimmune condition |
By working together, these experts make sure patients get the best care for their autoimmune eye conditions. They address both eye symptoms and the disease itself.
Medical Treatment Options for Autoimmune Eye Swelling
There are many ways to treat autoimmune eye swelling. We aim to reduce inflammation and keep your vision clear. Let’s look at the different treatments available and how they help manage the condition.
Corticosteroid Therapies
Corticosteroids are key in treating autoimmune eye swelling, mainly for sudden inflammation. They calm down the immune system’s wrong response, which helps lessen swelling and pain. Eye drops are often the first treatment for uveitis.
But, using corticosteroids for a long time can cause problems like cataracts or glaucoma. So, we watch patients closely to avoid these issues.
Immunosuppressive Medications
For long-term care or severe cases, immunosuppressive medications are effective. These drugs slow down the immune system, preventing it from attacking the eyes.
These medications can be used alone or with corticosteroids. This helps lower steroid doses and their side effects. We keep a close eye on patients on these drugs because they can weaken the body’s defense against infections.
Biologic Agents
Biologic agents are a newer type of treatment that targets specific parts of the immune response. They’re great for severe or hard-to-treat cases that haven’t responded to usual treatments.
Biologics offer a more precise treatment with fewer side effects than traditional immunosuppressants. But, their use must be carefully thought out because of possible risks like infections or other immune problems.
In summary, treating autoimmune eye swelling requires a personalized approach. We use various treatments to get the best results. We work with patients to find the right treatment plan for their specific situation.
Managing Dry Eye Disease in Autoimmune Conditions
Dry eye disease often affects people with autoimmune conditions. It needs a detailed management plan. This plan should include treatments to ease symptoms and protect eye health.
Artificial Tears and Lubricants
Artificial tears and lubricants are often the first treatment for dry eye. They moisturize the eyes, lessen discomfort, and clear vision. It’s best to use tears without preservatives to avoid irritation.
Key Considerations for Artificial Tears:
- Preservative-free options to reduce irritation risk
- Frequency of application based on symptom severity
- Compatibility with contact lenses if applicable
Prescription Eye Drops for Inflammation
When dry eye disease causes a lot of inflammation, prescription drops are needed. These drops can lessen inflammation and aid in healing. Cyclosporine and lifitegrast are examples of these medications.
Medication | Mechanism of Action | Common Side Effects |
Cyclosporine | Anti-inflammatory | Eye irritation, redness |
Lifitegrast | Lymphocyte function-associated antigen 1 antagonist | Dysgeusia, eye irritation |
Punctal Plugs and Other Procedures
For severe dry eye disease, punctal plugs might be suggested. These small devices block tear ducts, keeping tears on the eye’s surface.
Other procedures include:
- Restasis or other prescription eye drops
- Tear duct cauterization in severe cases
- Moisture goggles or other protective eyewear
Understanding treatment options and working with healthcare providers can help manage dry eye disease. This improves the quality of life for those with autoimmune conditions.
Lifestyle Modifications to Reduce Eye Inflammation
Changing our lifestyle can help manage eye inflammation from autoimmune diseases. Making smart choices can greatly improve our eye health and overall health.
Dietary Considerations
What we eat is key in fighting eye inflammation. Eating foods that fight inflammation is important. Foods rich in omega-3 fatty acids, like salmon and flaxseeds, are great. Also, eating lots of fruits and veggies, which are full of antioxidants, helps protect our eyes.
It’s also vital to avoid foods that can make inflammation worse. Some people find that dairy or gluten makes their symptoms worse. Keeping a food diary can help spot any foods that trigger eye inflammation.
Stress Management Techniques
Stress can make eye inflammation from autoimmune diseases worse. It’s important to find ways to manage stress. Mindfulness practices, like meditation and yoga, can help lower stress and improve health.
- Deep breathing exercises
- Progressive muscle relaxation
- Regular physical activity
These methods not only help with stress but also boost overall health. This can help lessen the severity of autoimmune eye issues.
Environmental Adjustments
Our surroundings can greatly affect our eye health. Making a few changes can help reduce eye inflammation. For example, using a humidifier keeps the air moist, which helps with dry eyes. Wearing sunglasses with UV protection also protects our eyes from harmful rays.
It’s also important to make our workspace better for our eyes. Following the 20-20-20 rule—looking away from screens every 20 minutes—can prevent eye strain.
Natural and Complementary Approaches
Medical treatments are key, but natural methods can also help eye health in autoimmune conditions. These methods can ease symptoms and lessen the impact of autoimmune eye problems.
Omega-3 Fatty Acids and Eye Health
Omega-3 fatty acids, like EPA and DHA, fight inflammation. They are good for people with autoimmune eye issues. You can find them in fatty fish, flaxseeds, and walnuts.
Nutritional Benefits of Omega-3 Fatty Acids:
- Reduce inflammation in the eyes
- Support overall eye health
- May improve dry eye symptoms
Anti-inflammatory Herbs and Supplements
Some herbs and supplements can fight inflammation in autoimmune eye issues. Turmeric, ginger, and green tea extracts are examples.
Herb/Supplement | Potential Benefits |
Turmeric (Curcumin) | Strong anti-inflammatory properties |
Ginger | Anti-inflammatory effects, antioxidant properties |
Green Tea Extracts | Antioxidant and anti-inflammatory benefits |
The Role of Antioxidants
Antioxidants protect the eyes from damage. Vitamins C and E, lutein, and zeaxanthin are key antioxidants for eye health.
Eating foods rich in antioxidants is good for your eyes. Leafy greens, berries, nuts, and citrus fruits are full of antioxidants.
Coping with Vision Changes and Eye Discomfort
Living with autoimmune eye conditions can be tough, with vision changes and discomfort. It’s key to tackle both the practical and emotional sides of coping with these issues.
Pain Management Strategies
Managing pain from autoimmune eye conditions is vital for a good quality of life. A mix of medical treatments and lifestyle changes can help. For example, warm compresses can ease eye strain and discomfort.
Medicines like corticosteroids or immunosuppressives can also control inflammation and pain.
” Pain is a significant symptom that can greatly impact a person’s daily activities and overall well-being,” says Medical Expert, an ophthalmologist specializing in autoimmune eye diseases. “A multi-faceted approach to pain management is often the most effective way to provide relief.”
Adaptive Tools for Vision Impairment
Adaptive tools and technologies can greatly help those with vision loss from autoimmune eye conditions. These tools include simple magnifying glasses to advanced digital devices that read out text or describe environments.
- Magnifying software for computers and smartphones
- Audiobooks and e-books with adjustable font sizes
- Specialized lighting for reading and other activities
Using these tools daily can help people stay independent and enjoy their activities.
Emotional Support Resources
Dealing with the emotional side of vision changes and eye discomfort is just as important as the physical symptoms. Support groups, counseling, and online resources offer emotional support and practical advice.
Seeking support is a sign of strength, not weakness. Connecting with others who get it can be very empowering and make you feel less alone.
In conclusion, coping with vision changes and eye discomfort needs a full approach. This includes medical treatment, adaptive tools, and emotional support.
When to Seek Emergency Medical Care
For those with autoimmune eye conditions, knowing when to get help fast is key. It can save your vision. These diseases can cause serious problems if not treated right.
Serious Complications Warning Signs
Some symptoms mean you need to go to the emergency room. These include:
- Sudden vision loss: If you lose vision suddenly or a lot in one or both eyes.
- Severe eye pain: Pain that’s too much or makes you feel sick to your stomach.
- Increased sensitivity to light: Light sensitivity that’s really bad and gets in the way of daily life.
- Eye redness and swelling: Big redness, swelling, or discharge from your eye.
Navigating Flare-Ups
Handling flare-ups well is key to avoiding big problems. Here’s what we recommend:
- Monitoring symptoms closely: Keep track of your symptoms to spot patterns.
- Adhering to treatment plans: Stick to what your doctor says to manage flare-ups.
- Seeking timely medical intervention: Call your doctor right away if your symptoms get worse a lot.
Effective Communication with Healthcare Providers
Talking clearly with your healthcare team is important. Here’s how:
- Being prepared for appointments: Bring a list of your symptoms, questions, and worries.
- Asking questions: It’s okay to ask about your condition, treatment, and what to expect.
- Reporting changes: Tell your doctor if your symptoms or condition change.
Knowing the warning signs and how to handle flare-ups helps manage autoimmune eye disease. It also ensures you get emergency care when needed.
Conclusion: Living Well with Autoimmune Eye Conditions
Managing autoimmune eye conditions well helps patients keep a good quality of life. We’ve looked at many parts of autoimmune eye swelling. This includes knowing its causes, spotting its symptoms, and the treatments out there.
Dealing with autoimmune eye disease needs a full plan. This plan includes medical care, changing your lifestyle, and getting support. By knowing your condition and working with doctors, you can handle your symptoms and avoid serious problems.
Managing autoimmune eye disease is more than just treating symptoms. It’s about taking care of your whole health. This means eating right, managing stress, and making changes in your environment to lessen eye swelling.
We stress the need for a team of healthcare experts. This team should include eye doctors and rheumatologists. By being involved in your care, you can live a happy and meaningful life with autoimmune eye disease.
FAQ
What is autoimmune eye swelling?
Autoimmune eye swelling is when the eyes get inflamed and swell. This happens because the body’s immune system mistakenly attacks the eye tissues.
What are the common symptoms of autoimmune eye inflammation?
Symptoms include eye redness, pain, and blurred vision. You might also feel sensitive to light and see swelling around your eyes. If it gets worse, it could even cause vision loss.
How is uveitis related to autoimmune diseases?
Uveitis is a type of eye inflammation that affects the middle layer of the eye. It’s often linked to diseases like rheumatoid arthritis and lupus.
What are the treatment options for autoimmune eye swelling?
Doctors use corticosteroids, immunosuppressive drugs, and biologic agents to treat it. The right treatment depends on how severe it is and what’s causing it.
Can lifestyle changes help manage autoimmune eye conditions?
Yes, making changes like eating right, managing stress, and avoiding certain triggers can help. These changes can reduce inflammation and ease symptoms.
How is dry eye disease managed in autoimmune conditions?
Dry eye is treated with artificial tears and eye drops. Sometimes, doctors use procedures like punctal plugs to help keep tears in the eyes.
Are there any natural approaches to managing autoimmune eye inflammation?
Omega-3 fatty acids, certain herbs, and antioxidants might help. But, always talk to a doctor before using them, as they should be part of a medical treatment plan.
When should I seek emergency medical care for my autoimmune eye condition?
Go to the emergency room if you suddenly lose vision, have severe eye pain, or feel very sensitive to light. These are signs of serious problems.
How can I cope with vision changes due to autoimmune eye conditions?
Use adaptive tools, find ways to manage pain, and get emotional support. These can help you deal with vision changes and discomfort from autoimmune eye conditions.
What is the role of specialists like ophthalmologists and rheumatologists in managing autoimmune eye diseases?
Ophthalmologists and rheumatologists work together to treat autoimmune eye diseases. They provide care that addresses both eye symptoms and the underlying disease.
Can autoimmune eye disease be cured?
While some autoimmune eye diseases can be managed well, a “cure” is rare. Treatment aims to control symptoms and prevent complications.
How do systemic autoimmune diseases affect eye health?
Diseases like rheumatoid arthritis, lupus, and autoimmune thyroid disease can harm the eyes. They can cause inflammation, dry eye, and vision problems. Managing these diseases is key to protecting eye health.
References
National Center for Biotechnology Information. Managing Autoimmune Uveitis: A Guide to Reduce Eye Swelling. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750361/