
Removing arteriovenous malformation (AVM) is a complex task. At Liv Hospital, we understand the concerns of those facing AVM diagnosis. We’re dedicated to giving top-notch care.
AVM surgery involves several methods, like microsurgical resection, endovascular embolization, and radiosurgery. Studies show endovascular embolization with Onyx is effective for cerebral AVMs. We find that complete resection leads to the best recovery rates, making it a top choice for some patients.
Key Takeaways
- AVM surgery includes microsurgical resection, endovascular embolization, and radiosurgery.
- Endovascular embolization using Onyx shows promising results in treating cerebral AVMs.
- Complete resection offers high one-year recovery rates.
- Liv Hospital provides a patient-centered, multidisciplinary approach.
- Advanced medical protocols shape treatment outcomes worldwide.
Understanding Arteriovenous Malformations (AVMs)
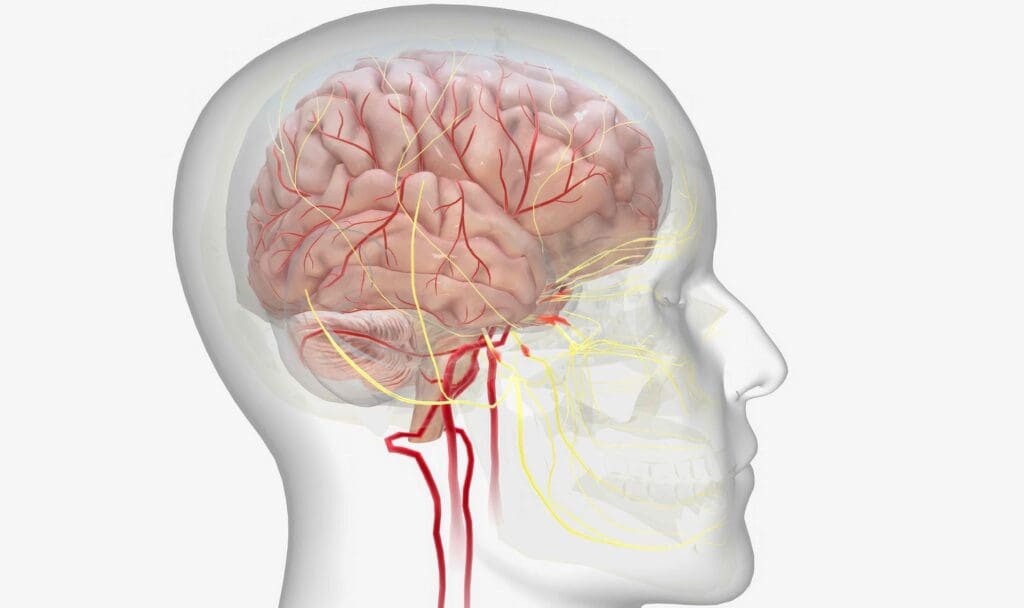
It’s important to understand arteriovenous malformations to know about brain vascular health. Arteriovenous malformations, or AVMs, are abnormal blood vessel formations in the brain. They can cause many neurological problems.
What Are Brain AVMs?
Brain AVMs are complex vascular anomalies. They have direct arteriovenous shunting without a capillary bed. This means blood goes straight from arteries to veins, skipping the capillary network.
These malformations can appear anywhere in the brain and differ in size and complexity. The exact cause of AVMs is not known, but they are thought to be present at birth.
How AVMs Affect Brain Function
AVMs can disrupt brain function in several ways. The abnormal blood flow can cause steal phenomenon. This means areas around the AVM don’t get enough blood, leading to neurological deficits.
AVMs can also cause mass effect. This happens when the malformation presses on nearby brain structures. Symptoms include headaches, seizures, or focal neurological deficits, depending on the AVM’s location.
Common Symptoms of Brain AVMs
The symptoms of brain AVMs vary widely. They depend on the size, location, and whether the AVM has ruptured. Common symptoms include:
- Seizures
- Headaches, often described as migraines
- Neurological deficits, such as weakness or numbness in parts of the body
- Hearing or vision problems
- Difficulty with speech or understanding language
In some cases, AVMs may not show symptoms until they rupture. This can lead to a hemorrhagic stroke. It’s a medical emergency with symptoms like sudden severe headache, nausea, vomiting, and loss of consciousness or focal neurological deficits.
When Is AV Malformation Surgery Necessary?

We look at several key factors to decide if AVM surgery is needed. These include symptoms, the risk of rupture, and the patient’s health.
AVM surgery is usually needed for those with symptoms or a high risk of bleeding. Symptomatic AVMs need quick attention because they can cause a lot of pain or harm to the brain.
Symptomatic AVMs
Symptomatic AVMs show symptoms like seizures, headaches, or brain problems. Surgery is often needed to fix these issues and stop more problems.
Ruptured AVMs
A ruptured AVM is a serious emergency. Surgery is usually needed right away to fix the damage and stop more bleeding.
High Bleeding Risk Assessment
It’s important to check the risk of bleeding to decide on surgery. We look at the AVM’s size, location, and how it drains blood to judge this risk.
| Risk Factor | Description | Surgical Consideration |
|---|---|---|
| AVM Size | Larger AVMs are associated with higher risks | Surgery often recommended for larger AVMs |
| AVM Location | Location in critical brain areas affects surgical risk | Surgical approach tailored to AVM location |
| Venous Drainage | Abnormal venous drainage increases rupture risk | Surgery considered to improve venous drainage |
Patient Selection Criteria
We carefully choose who needs AVM surgery. We look at the patient’s health, the AVM’s details, and the surgery’s risks and benefits. We also consider age, other health issues, and what the patient wants.
By carefully looking at these things, we can figure out if surgery is needed. Then, we create a treatment plan that fits the patient’s needs.
Types of AV Malformation Surgery Procedures
Arteriovenous malformations (AVMs) can be treated in several ways. Each method has its own benefits and is chosen based on the AVM’s size, location, and the patient’s health.
Microsurgical Resection
Microsurgical resection is a common and effective way to remove AVMs. This method involves removing the AVM under a microscope. It’s often used for AVMs that are easy to reach, giving a good chance of removing it all in one go.
For AVMs that are close to the surface and easy to get to, we often choose microsurgical resection. The process starts with opening the skull, then carefully removing the malformation.
Endovascular Embolization
Endovascular embolization is a less invasive method to treat AVMs. It blocks the arteries that feed the AVM. A catheter is used to deliver materials that stop blood flow to the AVM.
Embolization can be used alone or with other treatments like surgery or radiosurgery. It helps shrink the AVM and lowers the risk of surgery.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is a non-surgical treatment that uses radiation to shrink the AVM over time. It’s great for AVMs in hard-to-reach places in the brain.
The goal of SRS is to slowly close off the AVM. This can take years, and the patient may face bleeding risks during this time.
Combined Approaches
At times, a mix of treatments is used for the best results. For example, embolization might be done first to shrink a big AVM before surgery or radiosurgery.
Treatment plans are made for each patient. They consider the AVM’s details and the patient’s health.
The Complete Guide to Microsurgical Resection
Microsurgical resection is a top treatment for arteriovenous malformations (AVMs). It has a high cure rate if the AVM is completely removed. This method uses advanced tools and techniques for precise AVM removal.
Surgical Approach and Techniques
The success of microsurgical resection depends on several factors. These include the AVM’s size and location, and the patient’s health. Advanced imaging techniques are key in planning the surgery. They help neurosurgeons see the AVM’s details and its relation to the brain.
We use these imaging methods to plan the best surgery for our patients.
Complete vs. Partial Resection
The main goal is to remove the AVM completely. Complete removal leads to a higher cure rate and less risk of bleeding. But, sometimes, only part of the AVM can be removed. This is when the AVM is hard to reach or close to important brain areas.
Duration and Hospital Stay
The time needed for microsurgical resection varies. It depends on how complex the case is. Patients usually stay in the hospital for a few days to a week or more, based on their recovery.
“The length of hospital stay is influenced by factors such as the patient’s pre-operative condition and the presence of any post-operative complications.”
Success Rates for Complete Resection
Research shows that microsurgical resection can have high success rates for removing AVMs completely. This is true when experienced neurosurgeons perform the surgery.
The success of microsurgical resection also depends on the surgical team’s skill and the quality of care after surgery.
Endovascular Embolization: A Minimally Invasive Option
Endovascular embolization is becoming more popular for treating AVMs. It’s less invasive and works well for some cases. This method uses a catheter to reach the AVM through blood vessels. Then, it blocks the malformation with special materials.
Mechanism of Embolization
This method stops blood flow to the AVM. This reduces the chance of it rupturing and helps ease symptoms. We use different materials, like Onyx or n-BCA, to block the AVM. The choice depends on the AVM’s details and the doctor’s experience.
Indications for Embolization
Embolization is best for AVMs hard to reach surgically or at high risk of bleeding. It can also shrink the AVM before surgery, making it safer. We look at the AVM’s size, location, and blood flow when deciding if embolization is right.
Limitations of the Procedure
Embolization has its limits. Success depends on the AVM’s structure and the doctor’s skill. Sometimes, it can’t fully close the AVM. In these cases, other treatments like surgery or radiosurgery might be needed.
Recovery After Embolization
Recovery from embolization is usually faster than surgery. Most patients go home in a few days. But, recovery time can vary. We watch patients closely after the procedure and give them detailed care instructions.
| Procedure | Recovery Time | Success Rate |
|---|---|---|
| Endovascular Embolization | 2-5 days | 60-80% |
| Microsurgical Resection | 1-2 weeks | 80-95% |
| Stereotactic Radiosurgery | 1-3 days | 50-80% |
Radiosurgery for AVM Treatment
Radiosurgery is a key method for treating AVMs. It uses advanced technology to get the best results. We use it as a big part of our treatment plan for Arteriovenous Malformations.
Gamma Knife and Other Radiosurgical Methods
Gamma Knife radiosurgery is a precise radiation therapy. It targets the malformation without harming the brain. Other methods, like LINAC, work in a similar way. They help treat AVMs that are hard to reach or can’t be operated on.
The Obliteration Process
The goal of radiosurgery is to close the malformation. It does this by making new tissue in the affected vessels. This process is planned carefully to target the AVM nidus.
Over time, the vessels change and eventually close. This reduces the risk of bleeding.
Timeframe for Results
The effects of radiosurgery take years to show. Most AVMs start to close or disappear in 2-3 years. We use imaging to check on the progress and see if more treatment is needed.
Ideal Candidates for Radiosurgery
Not every AVM patient is right for radiosurgery. We look at the size, location, and type of AVM, and the patient’s health. It’s best for smaller AVMs in hard-to-reach places.
We choose the best treatment for each patient. This way, we can offer a plan that meets their specific needs and improves their chances of success.
Risks and Complications of AVM Surgery
It’s important for patients and doctors to know about AVM surgery risks. This surgery can save lives but comes with possible complications.
Procedure-Specific Risks
Each AVM surgery method has its own risks. For example, microsurgical resection might harm nearby brain tissue. Endovascular embolization could have issues with the catheter site. Stereotactic radiosurgery might show effects later, not right away.
Hemorrhage and Infection Risks
AVM surgery also risks hemorrhage and infection. These can happen during or after surgery. Keeping a close eye on patients and using clean techniques helps lower these risks.
Neurological Complications
Neurological problems like stroke, seizures, or brain function loss can happen. The chance of these issues depends on the AVM’s location and the surgery method. Knowing these risks helps patients make better choices.
Risk Mitigation Strategies
To lessen AVM surgery risks, a multidisciplinary approach is key. A team of experts creates a treatment plan tailored to each patient. Using advanced imaging and intraoperative monitoring also helps reduce complications.
Understanding and managing AVM surgery risks can improve patient results. Healthcare teams play a big role in this.
The Multidisciplinary Approach to Cerebral AVM Surgery
Managing cerebral arteriovenous malformations (AVMs) needs a team effort. A group of experts is key for the best care in AVM surgery.
Team Composition and Expertise
A team for AVMs includes neurosurgeons, neuroradiologists, and radiation oncologists. Neurosurgeons are vital for surgery. Neuroradiologists help with diagnosis and treatment. Radiation oncologists plan and do radiosurgery.
Each team member’s skills are important for choosing the right treatment. Working together helps find the best plan for each patient.
Collaborative Decision-Making
Teamwork is key in AVM care. The team looks at all treatment options together. This includes surgery, embolization, and radiosurgery.
This way, every part of the patient’s situation is considered. It leads to a treatment plan that fits the patient’s needs.
Benefits of Specialized AVM Teams
AVM teams bring many benefits. They improve patient results and lower risks. The team’s knowledge makes diagnosis and treatment better.
Also, a team can handle any problems that come up. This makes care smoother and safer.
Case Management Protocols
Good case management is important for AVM patients. It means clear communication and a plan for treatment and follow-up.
By following these steps, the team can give top-notch care. This is true from the start of treatment to after it’s done.
Recovery After Brain AVM Removal
Recovering from AVM surgery takes time and involves several stages. From the first days after surgery to ongoing check-ups, each step is important. Knowing what to expect can help patients and their families prepare for the journey ahead.
Immediate Post-Operative Care
Right after surgery, it’s key to prevent problems and ensure a smooth recovery. Patients usually stay in the ICU for 24-48 hours. Medical teams keep a close eye on their vital signs and watch for any signs of bleeding or complications.
Key aspects of immediate post-operative care include:
- Close monitoring of blood pressure and other vital signs
- Neurological assessments to check for any deficits or changes
- Pain management to keep the patient comfortable
- Prevention of deep vein thrombosis (DVT) through the use of compression stockings or anticoagulant medications
Rehabilitation Process
Rehabilitation after AVM surgery is customized for each patient. It may involve a team of healthcare professionals. The goal is to help patients regain lost functions and become independent again.
The rehabilitation process may include:
- Physical therapy to improve strength, balance, and mobility
- Occupational therapy to help with daily activities and tasks
- Speech therapy if there are issues with speech or swallowing
- Cognitive rehabilitation to address any memory or concentration problems
Long-term Follow-up Requirements
Long-term follow-up is vital after AVM surgery. It helps monitor for complications and ensures the AVM is gone. Regular imaging studies, like MRI or angiography, are used to check for any remaining AVM.
| Follow-up Timeline | Imaging Study | Purpose |
|---|---|---|
| 1-3 months post-op | MRI or CT scan | Baseline assessment of post-surgical changes |
| 6-12 months post-op | Angiography or MRI | Check for residual AVM |
| 1-2 years post-op | MRI or Angiography | Confirm complete obliteration of AVM |
AVM Rupture Recovery Timeline
Recovering from an AVM rupture is more complex and takes longer. The first phase focuses on managing the hemorrhage’s effects. The second phase is rehabilitation to address neurological deficits.
The recovery timeline for AVM rupture typically involves:
- Acute care in the ICU for hemorrhage management
- Subacute rehabilitation to address neurological deficits
- Long-term follow-up to monitor for any complications or recurrence
Choosing the Best Hospital for AVM Treatment
Finding the best hospital for AVM treatment is a big task. It requires looking at many important factors. Patients need to find a place that offers top-notch care for arteriovenous malformation.
Essential Facility Qualifications
When looking at hospitals for AVM treatment, check their qualifications.
It’s also key to see if the hospital has a strong neurosurgery department. They should have a team ready to handle AVMs. This team should include neurosurgeons, radiologists, and support staff up-to-date with AVM treatment.
Evaluating Surgical Team Experience
The skill of the surgical team matters a lot. Look for hospitals with neurosurgeons who have done many AVM surgeries. Ask how many AVM surgeries they do each year to see their experience.
Also, check if the hospital works well with different specialties. A team that works together can give a better treatment plan for you.
Treatment Protocols and Technology
Modern technology and treatment plans are key for AVM care. Hospitals with the latest equipment show they care about giving the best care.
Learn about the hospital’s AVM treatment plans. They should offer options like microsurgical resection and radiosurgery. A hospital that can tailor treatment to you is likely to give the best results.
Questions to Ask Your AVM Specialist
When talking to AVM specialists, have questions ready. This ensures you get the care you need. Some important questions include:
- What experience do you have with AVM treatment?
- What treatment options do you recommend for my specific condition?
- What are the possible risks and complications of the treatment you suggest?
- How will you and your team take care of me before, during, and after treatment?
By asking these questions, you can understand your treatment options better. This helps you know what to expect from the hospital and its staff.
| Criteria | Description | Importance Level |
|---|---|---|
| Accreditation | Recognition by reputable accrediting bodies | High |
| Surgical Team Experience | Number of AVM procedures performed annually | High |
| Treatment Protocols | Availability of various AVM treatment options | High |
| Technology and Equipment | Use of latest medical technology for diagnosis and treatment | High |
Choosing the right hospital for AVM treatment is a big decision. It involves looking at many factors like qualifications, team experience, and treatment plans. By doing your homework and asking the right questions, you can get the best care for your AVM.
Conclusion: Advances in AVM Treatment and Future Directions
Advances in AVM treatment have greatly improved patient outcomes. Ongoing research and new technologies promise even more progress. We now focus on personalized treatment plans, using the latest in avm surgery and arteriovenous malformation repair.
The field of AVM treatment is changing fast. We’re working to make treatments more effective and safe. By improving our understanding of AVMs, we’re developing more precise treatments. We’re using new imaging and surgical techniques to help.
We expect new technologies and treatment strategies to improve patient care even more. Our goal is to keep leading in avm treatment advances. This way, patients get the best care and support.
As we learn more about AVMs, we’re committed to applying this knowledge in treatment. This dedication drives us to improve AVM treatment worldwide. We aim to enhance the lives of patients everywhere.
What is an arteriovenous malformation (AVM) in the brain?
An AVM is a tangled mess of blood vessels in the brain. It can mess up blood flow. This might cause symptoms or problems.
What are the common symptoms of brain AVMs?
Symptoms include headaches, seizures, and neurological issues. Sometimes, people might have a stroke or hemorrhage. Others might not show symptoms until a doctor finds the AVM.
When is surgery necessary for treating an AVM?
Surgery is needed for ruptured AVMs, those causing big symptoms, or at high bleeding risk. The decision to operate depends on the AVM’s size, location, and the patient’s health.
What are the different types of AVM surgery procedures?
There are microsurgical resection, endovascular embolization, and stereotactic radiosurgery. Sometimes, a mix of these is used for the best results.
What is microsurgical resection for AVM removal?
Microsurgical resection is a surgery where the neurosurgeon removes the AVM. It’s used for AVMs that are risky to bleed.
How does endovascular embolization work for AVM treatment?
Endovascular embolization is a minimally invasive method. It uses a catheter to block blood flow to the AVM. This reduces its size and risk.
What is stereotactic radiosurgery, and how is it used for AVMs?
Stereotactic radiosurgery is a non-invasive treatment. It uses focused radiation to shrink the AVM over time. It’s good for hard-to-reach AVMs.
What are the possible risks and complications of AVM surgery?
Risks include hemorrhage, infection, and neurological problems. There can also be complications from the procedure, like radiation exposure in radiosurgery.
How is recovery managed after AVM removal surgery?
Recovery starts with post-operative care in a monitored setting. Then, there’s a rehabilitation process tailored to the individual. Long-term follow-up is also important to watch for any issues.
What factors should be considered when choosing a hospital for AVM treatment?
Look at the hospital’s qualifications and the surgical team’s experience. Also, check if they have the latest treatment technologies and good AVM management protocols.
What is the role of a multidisciplinary team in AVM surgery?
A multidisciplinary team is key in AVM surgery. They include neurosurgeons, neuroradiologists, and radiation oncologists. They work together for a complete treatment plan.
How long does it take to recover from AVM rupture?
Recovery time varies based on the hemorrhage’s severity, the person’s health, and the treatment. Rehabilitation is often needed, and recovery can take weeks to months or even longer.
What are the benefits of having AVM repair surgery?
Surgery can lower the risk of future bleeding, ease symptoms, and improve life quality. It removes or shrinks the malformation.
REFERENCES
- American Academy of Neurology. DOI 10.1212/WNL.0000000000213818. Retrieved from https://www.neurology.org/doi/10.1212/WNL.0000000000213818 siidon.guttmann.com























