This condition can result in serious health complications.
A specific type of bloodstream infection is called bacteremia. It’s caused by bacteria. Knowing about these infections is key to getting the right treatment fast. In this article, we’ll look at the most common types of bloodstream infections. We’ll also cover their causes, symptoms, and how to treat them.
Key Takeaways
- Bloodstream infections are serious medical conditions that require prompt attention.
- Bacteremia is a type of bloodstream infection caused by bacteria.
- Understanding the causes and symptoms is key for effective management.
- Quick treatment can greatly improve a patient’s chances of recovery.
- Without proper care, bloodstream infections can become severe and even deadly.
Understanding Bloodstream Infections
Bloodstream infections, also known as bacteremia, happen when bacteria or fungi get into the blood. This condition can result in serious health complications. If not treated quickly, these infections can be deadly.
Definition and Basic Concepts
Bacteremia is defined as the presence of live bacteria in the blood.
Here are some important stats about bloodstream infections:
| Condition | Description | Mortality Rate |
| Bacteremia | Presence of bacteria in the blood | Variable, depending on the causative organism and patient factors |
| Sepsis | Systemic inflammatory response to infection | Significant, can range from 10% to over 50% depending on severity |
| Septic Shock | Severe sepsis with hypotension unresponsive to fluid resuscitation | High, often exceeding 50% |
Importance of Early Detection and Treatment
It’s vital to catch bloodstream infections early and treat them quickly. Waiting too long can let the infection get worse. This can lead to sepsis or septic shock. Prompt intervention with the right antibiotics and care can save lives.
“Early recognition and treatment of sepsis are critical. Delays in diagnosis and treatment can result in significant morbidity and mortality.”
” Surviving Sepsis Campaign Guidelines
Healthcare providers need to know the risks and signs of bloodstream infections. This knowledge helps them diagnose and treat these infections well. We’ll look into this more in the next sections.
Bacteremia: The Most Common Bloodstream Infection
Bacteremia is defined as the presence of live bacteria in the blood.
What is Bacteremia?
Bacteremia is defined as the presence of live bacteria in the blood. It can come from infections in the skin, lungs, or urinary tract. Bacteria can get into the blood through wounds, medical procedures, or the lymphatic system.
This condition can result in serious health complications.
Bacteremia vs. Sepsis: Key Differences
Bacteremia is defined as the presence of live bacteria in the blood.
The main difference is the body’s reaction. Bacteremia is about the bacteria, while sepsis is about the body’s extreme reaction. Knowing this helps doctors manage the condition better.
Bacteremia vs. Septicemia: Understanding the Terminology
Bacteremia is defined as the presence of live bacteria in the blood.
In medical practice, using these terms correctly helps doctors diagnose and treat patients better. Bacteremia can lead to septicemia and sepsis. Quick action can stop these conditions from getting worse.
Types of Bloodstream Infections
It’s important to know the different types of bloodstream infections. This knowledge helps doctors diagnose and treat them better. These infections can start from various places and last for different times.
Primary Bloodstream Infections
Primary bloodstream infections happen when a pathogen directly gets into the blood. This can be through intravenous catheters or other medical devices. These infections often happen in hospitals.
Secondary Bloodstream Infections
Secondary bloodstream infections start from another infection in the body. This could be in the urinary tract, lungs, or skin. Knowing where the infection started is key to treating it right.
Transient vs. Intermittent vs. Continuous Bacteremia
Bacteremia is defined as the presence of live bacteria in the blood.
Community-Acquired vs. Hospital-Acquired Infections
Bloodstream infections can also be divided by where they happen. Community-acquired bloodstream infections occur outside hospitals, often in people with certain risks. Hospital-acquired bloodstream infections happen in patients while they’re in the hospital, often due to medical devices or procedures.
Knowing these types helps doctors give the best care for each patient.
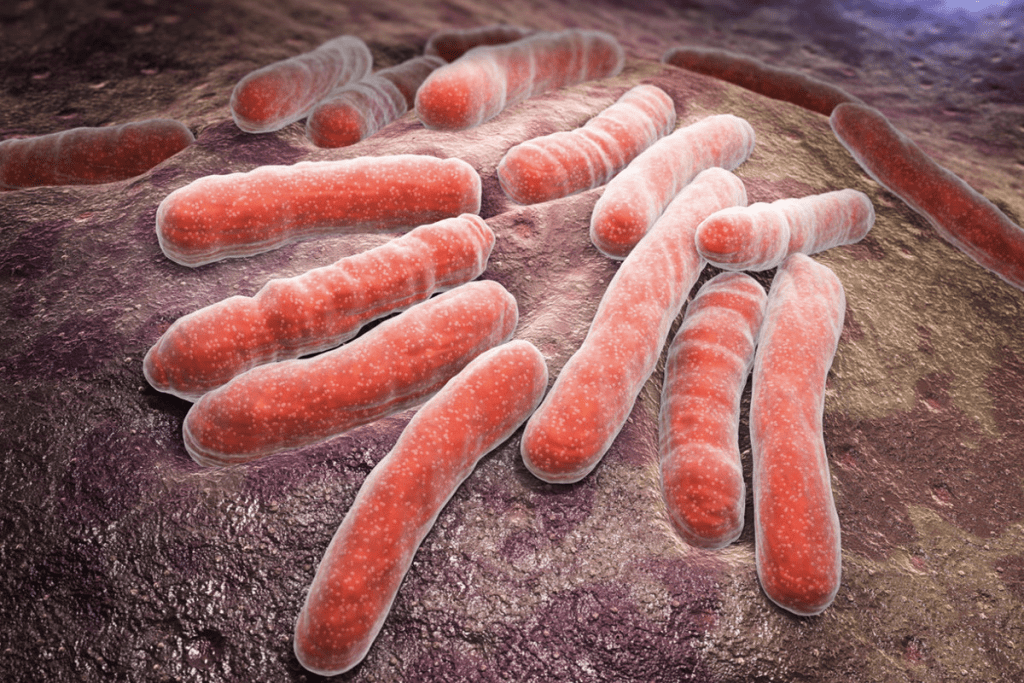
Common Bacterial Pathogens in Bloodstream Infections
It’s important to know the common bacteria causing bloodstream infections. Different bacteria can affect people in different ways. Some are more common in certain groups or places.
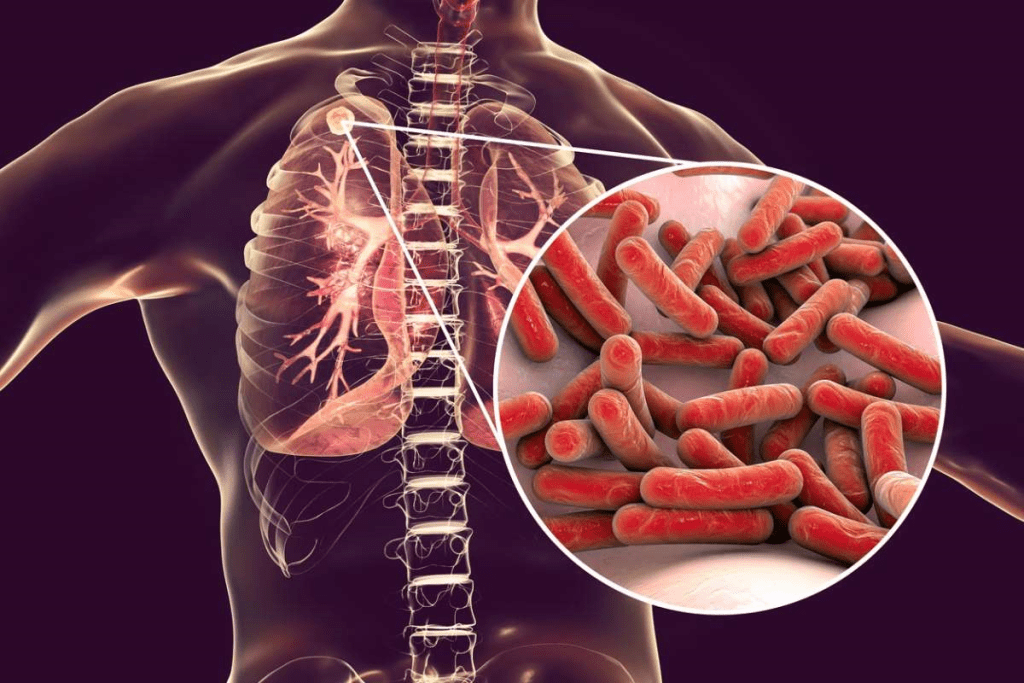
Staphylococcus Species
Staphylococcus aureus is a big problem in bloodstream infections. It can cause serious illness, mainly in those with weak immune systems or medical devices inside their body. MRSA, a type of Staphylococcus aureus, is hard to treat because it resists many antibiotics.
Streptococcus Species
Streptococcus pneumoniae and Streptococcus pyogenes are also common culprits. They can lead to mild to severe diseases, including sepsis.
Escherichia coli and Other Enterobacteriaceae
Escherichia coli (E. coli) and other Enterobacteriaceae are often found in healthcare settings. They can be hard to treat because they resist many antibiotics.
Pseudomonas and Other Non-Fermenters
Pseudomonas aeruginosa and other Gram-negative bacteria are known for causing severe infections. They are often resistant to many antibiotics, making treatment challenging.
Fungal and Viral Bloodstream Infections
Bacterial infections are a big worry in bloodstream infections. But, fungal and viral pathogens are also important, mainly for people with weak immune systems. These infections can be hard to spot and treat, needing a careful approach.
Candida and Other Fungal Pathogens
Fungal bloodstream infections, or fungemia, are serious, hitting hospitalized patients or those with catheters hard. Candida species are the top cause, making up most cases. Other fungi like Aspergillus and Histoplasma can also cause infections, but they’re rarer.
To find fungal infections, doctors use blood cultures and sometimes PCR or antigen tests. Treatment usually means antifungal meds, picked based on the fungus and the patient’s health.
Viral Causes of Bloodstream Infections
Viral bloodstream infections are less common but just as serious. Viruses like HIV, CMV, and EBV can harm people with weak immune systems a lot. Doctors use PCR or serological tests to diagnose these infections.
Managing viral infections means antiviral meds and sometimes just helping the patient get better. The right treatment depends on the virus and how strong the patient’s immune system is.
In short, fungal and viral bloodstream infections are big worries, mainly for those with weak immune systems. Spotting them early and treating them right is key to better health.
Risk Factors for Developing Bloodstream Infections
Bloodstream infections can happen in hospitals and in the community. Knowing what increases the risk is key to stopping them.
Hospital-Acquired Risk Factors
Hospitals see a lot of bloodstream infections. This is because of devices like central venous catheters and urinary catheters. Patients with these devices are at a higher risk because bacteria can grow on them.
Long hospital stays and surgeries also raise the risk. Patients on chemotherapy or with weakened immune systems are even more at risk.
Community-Acquired Risk Factors
Outside of hospitals, people can get bloodstream infections too. Underlying health conditions like diabetes and cancer make it more likely.
Being older or younger, and lifestyle choices like intravenous drug use, also increase the risk. Poor dental hygiene and infections can cause infections in the community.
Knowing these risks helps us fight bloodstream infections. This improves health outcomes in hospitals and the community.
Clinical Manifestations of Bacteremia
It’s key for doctors to know the signs of bacteremia to treat it well. This condition can show up in many ways. Its symptoms can be hard to spot because they’re not always clear.
Common Symptoms
Symptoms of bacteremia can vary among individuals. Many people get fever, chills, and rigors. Others might feel fatigue, malaise, or confusion. This is more common in older or weakened people.
Symptoms of bacteremia can vary among individuals.
Knowing when bacteremia might turn into sepsis is very important. Sepsis is a serious condition that can be deadly. Look for hypotension, tachycardia, tachypnea, and less urine. Blood tests showing high lactate, many white blood cells, or few white blood cells also point to sepsis.
| Symptoms/Signs | Description |
| Fever | Elevated body temperature, often accompanied by chills |
| Hypotension | Low blood pressure, indicating possible shock |
| Tachycardia | Rapid heart rate, a sign of stress or infection |
| Tachypnea | Rapid breathing rate, showing respiratory trouble |
| Confusion/Altered Mental Status | A vague symptom, common in older or weakened people |
| Elevated Lactate Levels | A lab finding showing poor blood flow to tissues |
Diagnosis of Bloodstream Infections
Diagnosing bloodstream infections takes a mix of doctor’s checks and lab tests. We use many steps to find the cause and choose the right treatment.
Blood Cultures and Interpretation
Blood cultures are key for spotting bloodstream infections. We take blood from patients thought to have infections and grow it in labs. The steps are:
- Getting blood from different spots to catch the infection.
- Using special bottles for growing different kinds of germs.
- Keeping the cultures warm for 5-7 days, or using newer methods.
Reading blood culture results needs careful thought. We tell true infections from false ones by looking at the germ, how many times it shows up, and the patient’s symptoms.
Laboratory Markers of Infection
Lab tests help with diagnosing and treating infections too. These include:
| Laboratory Marker | Description | Clinical Utility |
| C-reactive Protein (CRP) | An acute-phase reactant that increases in response to inflammation and infection. | Helps in assessing the severity of infection and monitoring response to treatment. |
| Procalcitonin (PCT) | A biomarker that is elevated in bacterial infections. | Assists in differentiating bacterial from viral infections and guiding antibiotic therapy. |
| White Blood Cell Count (WBC) | A measure of the body’s immune response. | Can indicate the presence of infection, though it’s not specific. |
Advanced Diagnostic Techniques
New ways to diagnose infections are getting better and faster. These include:
- Molecular diagnostics, like PCR, for quick germ identification.
- Mass spectrometry, for identifying germs by their proteins.
- Microarray technology, for finding many germs at once.
These new methods could lead to quicker diagnosis and better treatment. But, we must use them wisely, thinking about the patient and local infection patterns.
Treatment Approaches for Bloodstream Infections
Managing bloodstream infections requires a detailed plan. This plan includes starting treatment before knowing the exact cause. It also involves choosing the right treatment based on the cause and the patient’s health.
Empiric Antimicrobial Therapy
When a bloodstream infection is suspected, treatment starts right away. The choice of treatment depends on several things. These include the likely cause of the infection, local resistance patterns, and the patient’s health.
Key considerations for empiric antimicrobial therapy include:
- Coverage of likely pathogens based on the suspected source of infection
- Local antimicrobial resistance patterns
- Patient-specific factors such as allergies and comorbidities
Targeted Treatment Based on Pathogen
After identifying the cause through blood tests, treatment can be fine-tuned. This targeted approach helps in using the right antibiotics. It also reduces the chance of developing antibiotic resistance.
| Pathogen | Preferred Antimicrobial Therapy | Alternative Options |
| Staphylococcus aureus (MSSA) | Nafcillin or Oxacillin | Cefazolin, Vancomycin |
| Escherichia coli | Ceftriaxone | Ciprofloxacin, Piperacillin-tazobactam |
| Pseudomonas aeruginosa | Piperacillin-tazobactam or Ceftazidime | Meropenem, Ciprofloxacin |
Supportive Care Measures
Supportive care is key in managing bloodstream infections, mainly in severe cases. It includes giving fluids, using medicines to support blood pressure, and supporting organs as needed.
We stress the need for a complete treatment plan. This plan should include the right antibiotics and supportive care. Tailoring treatment to each patient’s needs and the specific pathogen improves outcomes and lowers complication risks.
Complications of Untreated Bloodstream Infections
Untreated bloodstream infections can cause severe and life-threatening problems. We will look at the dangers of not treating these infections quickly. It shows why finding and treating them early is so important.
Septic Shock
Septic shock is a major risk of untreated bloodstream infections. It happens when the body’s fight against infection gets out of control. This leads to widespread inflammation and can cause blood pressure to drop.
Key characteristics of septic shock include:
- Hypotension (low blood pressure)
- Tachycardia (rapid heart rate)
- Tachypnea (rapid breathing rate)
- Confusion or altered mental status
Organ Dysfunction and Failure
Untreated bloodstream infections can harm organs like the kidneys, liver, lungs, and heart. This can cause problems like kidney failure, lung issues, or heart problems.
| Organ | Dysfunction/Failure |
| Kidneys | Acute kidney injury, reduced urine output |
| Lungs | Respiratory failure, need for mechanical ventilation |
| Liver | Elevated liver enzymes, jaundice |
| Heart | Cardiac dysfunction, reduced ejection fraction |
Long-term Sequelae
People who survive bloodstream infections may face long-term effects. These can include lasting fatigue, brain problems, and physical disabilities. These issues can greatly affect a person’s life and may need ongoing care and therapy.
We stress the need for quick and effective treatment of bloodstream infections. Early action can greatly improve outcomes and lower the chance of lasting problems.
Prevention Strategies for Bloodstream Infections
Bloodstream infections can be stopped with the right steps in healthcare and community efforts. It’s key to cut down on sickness, death, and the cost of treatment.
Healthcare Setting Prevention
In hospitals, stopping these infections means using strong infection control. This includes washing hands well, using antibiotics wisely, and keeping procedures clean.
Managing catheters and other devices right is also important. Keeping an eye on infection rates and giving feedback helps too.
| Prevention Measure | Description | Impact |
| Hand Hygiene | Proper hand washing techniques before and after patient contact | Reduces transmission of pathogens |
| Antimicrobial Prophylaxis | Appropriate use of antibiotics before surgical procedures | Decreases surgical site infections |
| Sterile Techniques | Use of sterile equipment and techniques during invasive procedures | Minimizes introduction of pathogens into the bloodstream |
Community-Based Prevention
In the community, we use public health and education to fight infections. This includes shots to protect against some infections, teaching about wound care, and spreading the word about infection risks.
It’s also vital to use antibiotics correctly to fight off resistant bacteria. This is a big deal in treating bloodstream infections.
Special Populations and Bloodstream Infections
Special groups, like kids and older adults, need special care when dealing with bloodstream infections. They have different health needs and body responses that affect how we find, treat, and prevent these infections.
Pediatric Considerations
Children are more likely to get bloodstream infections because their immune systems are not fully grown. We must think about these points when treating kids with these infections:
- Age-specific risk factors: Babies and young kids are more at risk because their immune systems are not ready yet.
- Different clinical presentations: Kids might show symptoms that are not clear, making it harder to diagnose.
- Weight-based dosing: We have to carefully figure out the right amount of medicine based on the child’s weight.
Geriatric Considerations
Older people are also more likely to get bloodstream infections because of age-related changes and weaker immune systems. When treating older adults with these infections, we should keep in mind:
- Comorbid conditions: Older adults often have many health problems that can make treatment harder.
- Polypharmacy: They might take many medicines, which can lead to more drug interactions.
- Atypical presentations: Older adults might not show typical signs of infection, so finding it early is key.
By knowing these special needs, we can give better care to both kids and older adults with bloodstream infections.
Recent Advances in Bloodstream Infection Management
The way we treat bloodstream infections is changing fast. New discoveries in treatments and tests are making a big difference. This is leading to better care for patients.
New Antimicrobial Agents
New medicines are key in fighting bloodstream infections. They work against tough-to-beat germs and are more effective.
- Novel Antibiotics: Antibiotics like ceftazidime-avibactam and meropenem-vaborbactam fight hard-to-beat bacteria.
- Antifungal Agents: New treatments for fungal infections include better triazoles and echinocandins.
Innovative Diagnostic Approaches
New ways to diagnose bloodstream infections are also emerging. These help doctors find the cause of infections faster and more accurately.
- Rapid Diagnostic Tests: Tests like PCR and MALDI-TOF help quickly identify pathogens and resistance.
- Advanced Blood Culture Systems: New blood culture systems spot germs sooner, speeding up treatment.
These new treatments and tests are changing how we handle bloodstream infections. By using these advances, we can help patients more and fight infections better.
Conclusion
Understanding bloodstream infections, like bacteremia, is key to better patient care. We’ve looked at what these infections are, how they’re diagnosed, and how to treat them.
Bloodstream infections can cause serious problems if not treated quickly. Finding them early and using the right medicines is vital. This helps avoid long-term issues and saves lives.
This article highlights the need for knowledge and education in fighting these infections. Doctors and nurses must keep up with new ways to find and treat infections. This ensures the best care for patients.
To manage bloodstream infections well, we need a complete plan. This includes preventing infections, finding them early, and treating them right. By doing this, we can help patients get better and make healthcare systems work better too.
FAQ
What is bacteremia?
Bacteremia is defined as the presence of live bacteria in the blood.
What is the difference between bacteremia and sepsis?
Bacteremia is defined as the presence of live bacteria in the blood.
What are the common symptoms of bacteremia?
Symptoms of bacteremia include fever, chills, and a fast heart rate. It can also cause fast breathing. In severe cases, it can lead to sepsis, causing confusion, less urine, and extreme tiredness.
How is bacteremia diagnosed?
Doctors diagnose bacteremia by taking a blood sample. They try to grow bacteria in a lab. They also use other tests and markers to help diagnose.
What are the risk factors for developing bloodstream infections?
People with weak immune systems are at risk. So are those with invasive medical devices, recent surgery, and certain health conditions.
How are bloodstream infections treated?
Treatment includes antibiotics chosen based on the bacteria. Patients may also need fluid replacement and help managing organ problems.
What are the possible complications of untreated bloodstream infections?
Untreated infections can cause severe problems. These include septic shock, organ failure, and long-term health issues. Septic shock is very dangerous and needs quick medical help.
How can bloodstream infections be prevented?
Preventing infections involves good hygiene and sterile procedures in healthcare. Vaccines and proper wound care are also important.
Are there special considerations for certain populations regarding bloodstream infections?
Yes, kids and older adults need special care. Their bodies and health issues are different, so treatment must be tailored.
What are the recent advances in the management of bloodstream infections?
New antibiotics and diagnostic tools are being developed. These advances help improve treatment outcomes for patients.
Can bloodstream infections be community-acquired?
Yes, infections can happen outside of hospitals. Community-acquired infections can be caused by many pathogens.
What is the significance of early detection and treatment of bloodstream infections?
Finding and treating infections early is key. It prevents severe problems like sepsis and organ damage. Quick action can greatly improve patient outcomes.
References
Verway, M., et al. (2022). Prevalence and mortality associated with bloodstream infections: A study of over 22,000 episodes. Journal of Clinical Microbiology.