Last Updated on October 31, 2025 by Saadet Demir
Bacterial acute pharyngitis is a big problem in primary care, affecting millions globally. Getting the right diagnosis and treatment is key to avoid serious issues like rheumatic heart disease.
Streptococcal pharyngitis, or “strep throat,” is a bacterial throat infection caused by Streptococcus pyogenes (group A streptococcus). Knowing how it works is vital for treating it well.

It’s important to know what causes bacterial acute pharyngitis to treat it well. We’ll look at what it is, how common it is, and the bacteria that cause it. This will help us understand it better.
Bacterial acute pharyngitis is an infection of the throat caused by bacteria. It’s a big problem, mainly for kids in school. The most common bacteria causing this is Group A beta-hemolytic streptococcus (GABHS).
This infection is most common in school-age kids. It gets less common as people get older. Doctors need to remember this when they see patients.
The main bacteria causing throat infections is Streptococcus pyogenes, or Group A beta-hemolytic streptococcus (GABHS). Other bacteria like Arcanobacterium haemolyticum, Neisseria gonorrhoeae, and Fusobacterium necrophorum can also cause infections, but not as often.
Bacterial Pathogen | Characteristics | Prevalence |
Group A beta-hemolytic streptococcus (GABHS) | Most common cause of bacterial pharyngitis | High among school-age children |
Arcanobacterium haemolyticum | Causes pharyngitis, often with a rash | Less common, mainly affects teens and young adults |
Neisseria gonorrhoeae | Cause of gonococcal pharyngitis, often sexually transmitted | Less common, linked to certain risk factors |

Streptococcal pharyngitis happens when Group A beta-hemolytic streptococcus (GABHS) sticks to and invades the pharynx’s cells. This causes an inflammatory response in the host. It’s key to understanding how the disease develops and grows.
The invasion starts with GABHS sticking to the pharyngeal cells. Streptococcus pyogenes, the cause of streptococcal pharyngitis, is a gram-positive coccus. It forms fine chains on gram-stain material. The bacteria stick due to adhesins on their surface.
The invasion process includes:
The host’s immune system reacts to GABHS and its parts, like the cell wall and streptolysins. This response brings immune cells like neutrophils and macrophages to fight the infection.
This fight can cause symptoms like:
Knowing how streptococcal pharyngitis works is vital. It helps in making treatments that fight the bacteria and the host’s reaction to it.
Bacterial acute pharyngitis shows clear signs that doctors need to spot for the right diagnosis. It starts suddenly and can be very severe, affecting how well a person feels.
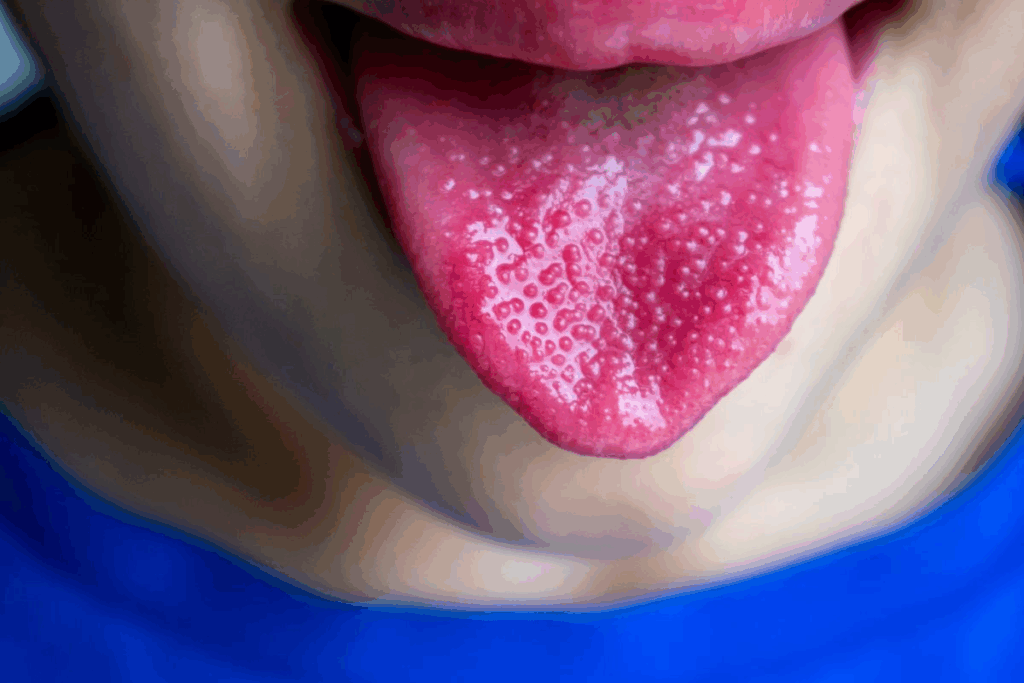
The main signs of bacterial pharyngitis are a sore throat and a fever over 100.4 degrees Fahrenheit. You might also see a red throat and pus on the tonsils. Swollen neck glands are another important sign.
Telling bacterial pharyngitis apart from viral is key for the right treatment. Bacterial infections, often from Group A Streptococcus, have worse symptoms like higher fevers. Look for red throat, spots on the palate, and swollen tonsils with pus.
Signs of bacterial pharyngitis include swollen neck glands, red throat, and tonsil pus. These signs help doctors diagnose and confirm the infection. Finding these signs early is important to start the right treatment and avoid serious problems.
Diagnosing bacterial acute pharyngitis requires a detailed approach. This includes both clinical checks and lab tests. Getting the diagnosis right is key to treating the illness and avoiding serious problems.
First, we assess the patient clinically. We use tools like the Centor criteria to guess if a patient has Group A Streptococcal (GAS) infection. The criteria include:
Patients with many Centor criteria signs are more likely to have GAS pharyngitis. But, we need to confirm this with more tests.
Lab tests are vital to confirm bacterial pharyngitis. We use two main tests:
Test | Description | Advantages |
Rapid Antigen Detection Test (RADT) | Quick test to detect GAS antigens | Rapid results, high specificity |
Throat Culture | Gold standard for diagnosing GAS pharyngitis | High sensitivity, allows for antibiotic sensitivity testing |
The Infectious Disease Society of America (IDSA) suggests starting with RADT. This is because it’s fast. Then, we do throat cultures if RADT is negative but we’re not sure.
Imaging isn’t usually needed for bacterial pharyngitis. But, if there’s a chance of complications like a peritonsillar abscess, we might use it. Ultrasound or CT scans can help in these cases.
By using clinical tools and lab tests together, we can accurately diagnose bacterial acute pharyngitis. This helps us treat it properly.
Antibiotics are key in treating bacterial acute pharyngitis. They help lessen symptoms, prevent complications, and stop the spread of the infection.
Choosing the right antibiotic is important. Penicillin or amoxicillin are top choices for treating bacterial pharyngitis. They are effective, safe, and target the bacteria well.
For those not allergic to penicillin, amoxicillin is often the first choice. It works as well as penicillin but is easier to take. The usual dose is 50 mg/kg once a day (or 25 mg/kg twice a day) for 10 days.
The standard treatment time for uncomplicated bacterial pharyngitis is 10 days. It’s vital to finish the antibiotic course to avoid treatment failure and antibiotic resistance.
For those allergic to penicillin, azithromycin or clarithromycin can be used. The choice depends on local resistance patterns and the patient’s needs.
Important points for treating bacterial acute pharyngitis include:
Following evidence-based guidelines helps manage bacterial acute pharyngitis. It reduces complications and improves patient outcomes.
Managing symptoms is key in treating bacterial acute pharyngitis. It makes patients feel better and helps them recover faster. Supportive care is important for quick recovery and to avoid complications.
Controlling pain is vital for patients with bacterial acute pharyngitis. We suggest using acetaminophen or NSAIDs to manage pain from GAS pharyngitis. These medicines not only ease pain but also lower fever.
Table 1: Common Pain Management Options
Medication | Dose | Frequency |
Acetaminophen | 500-1000 mg | Every 4-6 hours |
Ibuprofen | 200-400 mg | Every 4-6 hours |
Drinking enough fluids is essential for patients with bacterial acute pharyngitis. We suggest drinking water, clear broths, or electrolyte-rich drinks. Eating soft, bland foods can also help by reducing throat irritation.
Recommended foods include:
Rest is important for recovering from bacterial acute pharyngitis. We advise avoiding hard activities and resting well. Changing activities to avoid straining the throat can also help.
By adding these supportive care steps to their treatment, patients can manage their symptoms better. This improves their overall recovery.
Bacterial acute pharyngitis in kids needs a special treatment plan. This plan must consider their age and growth stage. We must think about several factors to treat them well and avoid complications.
When treating bacterial acute pharyngitis in kids, we adjust treatments based on their age. Antibiotic choices and dosages are tailored for their developing bodies and possible sensitivities.
We pick the right antibiotic for a child’s age. For example, amoxicillin is often used because it’s safe and works well.
Dosing for kids depends on their weight and age. It’s important to stick to the right dosing to treat the infection well. Accurate dosing helps avoid bad side effects.
Kids with group A strep pharyngitis should miss school until they’re no longer sick. They should have been on antibiotics for at least 12 to 24 hours. This helps stop the spread of the infection and lets the child recover better.
By following these school attendance recommendations, we can lower the spread of bacterial acute pharyngitis in schools.
Antibiotic resistance is a big problem in treating bacterial infections like acute pharyngitis. We use antibiotics a lot, but bacteria are getting better at fighting them. This makes it hard for doctors to treat infections.
Many antibiotics, like azithromycin and clindamycin, are not working as well as they used to. The problem is different in different places and changes over time. This means we need to watch it closely and treat patients in a way that works best for where they are.
Regional Resistance Patterns: Studies show that resistance levels vary a lot. For example, in the U.S., some areas have more resistant Streptococcus pyogenes than others.
Antibiotic | Resistance Rate (%) | Region |
Azithromycin | 12-15 | North America |
Clarithromycin | 10-12 | Europe |
Clindamycin | 8-10 | Asia |
To fight resistance, we need to use antibiotics wisely. This means choosing the right one and using it for the right amount of time. We also need to cut down on when we use antibiotics too much.
Key Principles of Antibiotic Stewardship:
As resistance grows, finding new ways to treat infections will get harder. Scientists are working on new antibiotics and treatments. They’re seeing good results in early tests.
By understanding resistance and using antibiotics carefully, we can improve treatment for bacterial infections like acute pharyngitis.
Untreated bacterial acute pharyngitis can lead to serious problems. These include both suppurative and non-suppurative complications. These issues can greatly affect a patient’s health and quality of life. It’s vital to know about these complications to stress the need for quick and proper treatment.
Suppurative complications happen when the infection spreads to nearby areas or through the blood. Some common ones are:
These complications need quick medical care. This often includes draining the abscess and using antibiotics.
Non-suppurative sequelae happen because of the body’s immune response to the infection. The most serious ones are:
Knowing about these complications shows why it’s so important to diagnose and treat bacterial acute pharyngitis early. This can help prevent these serious outcomes.
It’s important for patients with bacterial acute pharyngitis to know when they need to see a doctor right away. We will talk about the warning signs and red flags for urgent care. We will also cover emergency situations and follow-up care guidelines.
Certain symptoms mean you should see a doctor quickly. These include:
If you have any of these symptoms, you should get medical help. Early treatment can stop complications and help you get better faster.
In some cases, bacterial acute pharyngitis can be a serious emergency. These include:
If you’re facing any of these emergencies, get medical help right away. Waiting can cause serious problems.
After you’ve been treated, it’s key to follow up to make sure the infection is gone. We suggest:
Knowing when to get medical help and following these steps can help you get better faster. It also lowers the chance of serious problems.
It’s important to treat bacterial acute pharyngitis well to avoid serious problems and stop it from spreading. We’ve talked about how to diagnose and treat streptococcal pharyngitis, a common cause of this illness.
Getting the right diagnosis is key to treating bacterial pharyngitis right. This ensures the right antibiotics are used. Following proven treatment plans helps doctors improve patient care and lower the chance of serious complications.
We stress the need for good treatment and care plans. This includes managing pain, staying hydrated, and resting. It’s also vital to use antibiotics wisely to fight antibiotic resistance.
By using these methods, we can give the best care to those with bacterial acute pharyngitis. This helps both individuals and communities. Treating streptococcal pharyngitis well means finding a balance between treating the infection and using antibiotics carefully.
Bacterial acute pharyngitis is an infection of the pharynx. It’s usually caused by Group A beta-hemolytic streptococcus (GABHS).
Symptoms include a sore throat and fever. You might also have swollen lymph nodes and white patches on your tonsils.
Doctors use a few methods to diagnose it. These include clinical assessment, rapid antigen detection testing, and sometimes lab tests.
Treatment usually involves antibiotics. Doctors might prescribe penicillin or amoxicillin to help symptoms.
Treatment usually lasts about 10 days. But it can vary based on the antibiotic and the patient.
If left untreated, it can cause abscesses. It can also lead to rheumatic fever, a serious condition.
To manage symptoms, take pain relief medication. Stay hydrated and rest as much as you can.
While prevention is not always possible, good hygiene helps. Frequent handwashing can reduce the risk of getting it.
Seek medical help if symptoms are severe. Also, if you have trouble swallowing or if symptoms get worse.
Yes, children need special treatment. This includes age-specific dosing and considering their overall health.
Antibiotic stewardship is key. It helps prevent antibiotic resistance and ensures treatment is effective.
Yes, other bacteria can also cause pharyngitis. But GABHS is the most common and serious cause.
Bacterial pharyngitis has more severe symptoms. It often has specific signs like exudative throat.
National Center for Biotechnology Information. (2025). How to Treat Bacterial Acute Pharyngitis A Guide. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559007/)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us