Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know over 40% of adults in the United States are obese? This means they have a Body Mass Index (BMI) of 30 or higher. This shows the need for effective ways to treat obesity, like weight loss surgery.
Bariatric weight classification is key to see if someone can have surgery. Doctors use BMI to decide. Health groups set these BMI levels.
We offer top-notch healthcare services worldwide. We carefully evaluate patients before surgery and provide personalized support throughout their journey.
Key Takeaways
- Obesity is defined as a BMI score of 30 or more.
- Bariatric weight classification is critical for determining weight loss surgery eligibility.
- Obesity classification standards are based on BMI thresholds.
- Comprehensive evaluation is essential for patients considering weight loss surgery.
- Personalized care and support are key throughout the treatment process.
Understanding Bariatric Weight Classification
To understand bariatric weight classification, we need to know its definition and why it matters. It’s not just about a patient’s weight. It’s about figuring out if they’re a good candidate for weight loss surgery and the health risks involved.
Definition of Bariatric Weight Classification
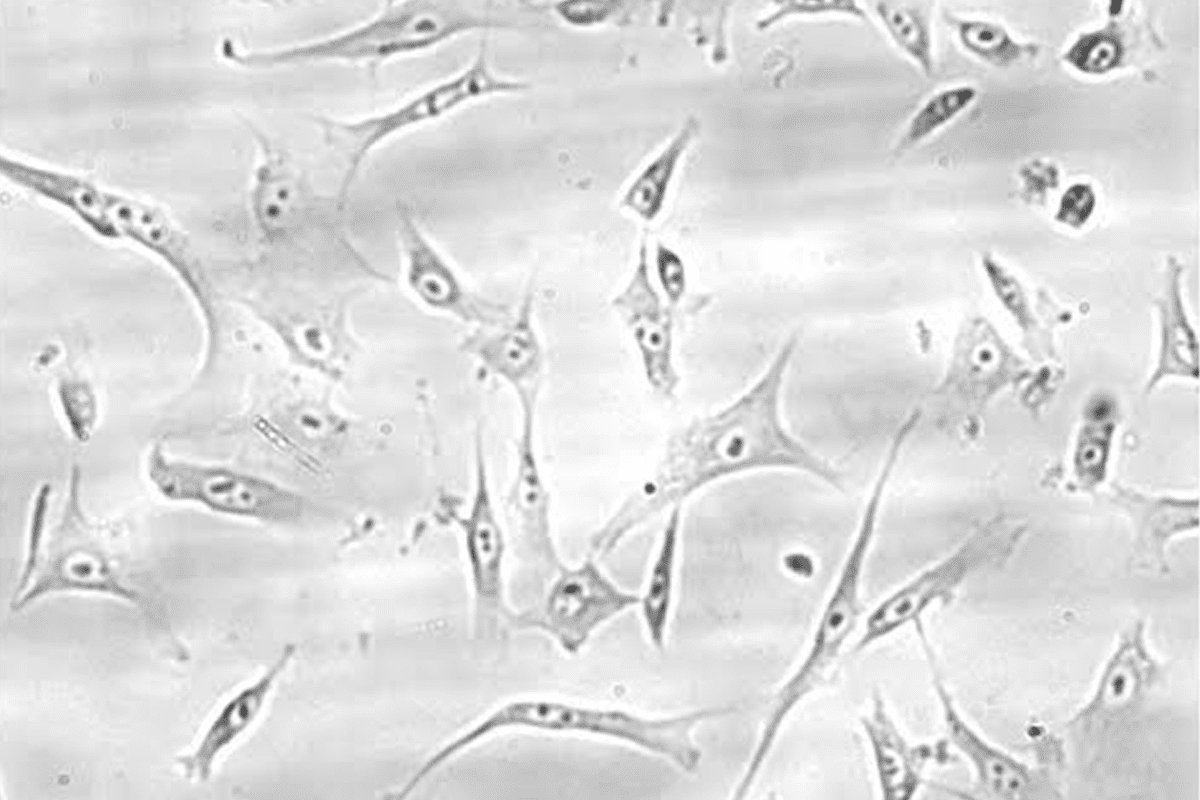
Bariatric weight classification uses the Body Mass Index (BMI). BMI is a number that shows how a person’s weight compares to their height. BMI is a key tool for doctors to sort people into different weight groups. This helps show how serious their obesity is.
We use BMI to see if someone needs bariatric surgery. This usually means a BMI of 40 or higher. Or a BMI of 35 or higher with health problems linked to obesity.
Using BMI in bariatric weight classification shows how important clinical guidelines are. It helps us understand the health risks of obesity. Knowing a patient’s BMI helps us choose the best treatment for them.
Importance of Weight Classification
Weight classification is key because it shapes how we treat obesity. It helps us find the right people for bariatric surgery and other weight loss plans. It guides doctors in making the best choices for their patients. This leads to better health results.
- Accurate weight classification helps find patients at risk for health problems.
- It lets doctors create treatment plans that fit each patient’s needs.
- It’s critical for deciding if someone can have bariatric surgery or other weight loss treatments.
Understanding bariatric weight classification helps us care for patients with obesity better. Our team stresses the need for accurate classification. This ensures the best results for our patients.
The Obesity Epidemic in the United States
The obesity problem in the U.S. is complex and urgent. It affects many people and the healthcare system too. We need to act fast and find good solutions.
Looking at obesity rates and health risks is key. Obesity is a big issue for everyone, not just individuals. It’s a problem that needs a team effort to solve.
Statistics on Obesity Rates
Obesity rates in the U.S. have been going up for years. Now, over two-fifths of adults are obese. Childhood obesity is also a big worry, affecting the future health of our country.
Here are some important statistics:
Year | Adult Obesity Rate | Childhood Obesity Rate |
2010 | 35.7% | 16.9% |
2015 | 37.7% | 17.2% |
2020 | 42.4% | 19.3% |
Health Risks Associated with Obesity
Obesity is linked to serious health problems. These include heart disease, type II diabetes, and high blood pressure. These issues can lower quality of life and increase healthcare costs and deaths.
It’s important to know these risks to fight obesity. Some major health risks are:
- Coronary Heart Disease: Obesity raises heart disease risk due to high blood pressure and cholesterol.
- Type II Diabetes: Obese people face a higher risk of type II diabetes, making it hard to control blood sugar.
- Hypertension: High blood pressure often goes with obesity, putting extra strain on the heart.
By knowing these facts, we can tackle the obesity crisis. This will help improve public health.
Defining Bariatric Surgery
Bariatric surgery is a proven way to treat severe obesity. It changes the digestive system to help people lose weight. This is a big decision, and we’re here to support you every step of the way.
Types of Bariatric Surgical Procedures
There are many types of bariatric surgery, each aimed at helping patients lose a lot of weight. The most common ones are:
- Gastric Bypass Surgery: This makes a small pouch from the stomach and connects it to the small intestine.
- Sleeve Gastrectomy: A big part of the stomach is removed, leaving a narrow “sleeve.”
- Adjustable Gastric Banding: A band is put around the upper stomach to make a small pouch.
Each procedure has its own benefits and risks. We’ll help you choose the best one for you, based on your health and weight loss goals.
Eligibility Criteria for Bariatric Surgery
To get bariatric surgery, you need to meet certain criteria. These include:
Criteria | Description |
BMI Requirement | A Body Mass Index (BMI) of 40 or higher, or a BMI of 35 with significant obesity-related health conditions. |
Previous Weight Loss Attempts | Proof of trying to lose weight through diet and exercise. |
Health Evaluations | Thorough health checks to see if surgery is right for you. |
We carefully check if you’re a good candidate for bariatric surgery. We look at your health, past weight loss efforts, and any health problems you have.
How Many Pounds Are Considered Bariatric?
To understand bariatric weight, we must first look at Body Mass Index (BMI). BMI is a key tool for doctors to check a person’s weight and health risks.
BMI and Its Role in Classification
BMI is found by dividing a person’s weight in kilograms by their height in meters squared. This number is key in deciding if someone is in the bariatric weight range. A BMI of 40 or more is usually seen as morbidly obese, showing a big health risk.
We use BMI to sort weight categories. For example, a BMI of 35 to 39.9 is obese, and 40 or higher is morbidly obese. These clinical guidelines help us find who might need bariatric surgery or other weight loss help.
Weight Thresholds for Bariatric Classification
The weight needed for bariatric classification changes with height. For a 5’6″ (168 cm) person, about 250 pounds (113 kg) is a BMI of 40. We look at these weights when thinking about bariatric surgery for patients.
Knowing these weight ranges and BMI levels is key for finding the right treatment for obesity. By explaining these weight categories and the clinical guidelines, we can help our patients more on their weight loss path.
Different Types of Obesity
It’s key to know the different types of obesity to manage weight well. Obesity isn’t just one thing; it’s a range of conditions. Each has its own health risks and effects. We use the Body Mass Index (BMI) to sort obesity into classes.
Class I Obesity
Class I obesity has a BMI of 30 to 34.9. People in this group face higher risks of diseases like type 2 diabetes and heart problems. Starting early and making lifestyle changes can help a lot.
Class II Obesity
Class II obesity has a BMI of 35 to 39.9. At this level, health risks grow, including severe conditions. Full weight management plans are suggested for those here.
Class III Obesity
Class III obesity, or severe obesity, has a BMI of 40 or more. It brings big health risks, even death. Special care and sometimes surgery might be needed for Class III.
Knowing the types of obesity helps doctors tailor care for each patient. Understanding obesity’s types and risks helps us make better treatment plans.
Our team focuses on a complete weight management plan. This includes diet, exercise, and sometimes medical help. Treating obesity based on its type can lead to better health and less health problems.
The Role of Body Mass Index (BMI)
Body Mass Index (BMI) is key in checking health risks tied to weight. It’s a tool doctors use to see if a person’s weight is healthy for their height.
Calculating Your BMI
To find your BMI, just divide your weight in kilograms by your height in meters squared. Or, you can use online BMI calculators. Knowing your BMI category is important. It shows health risks and guides health checks.
For adults, BMI falls into several groups:
- Underweight: BMI
- Normal weight: BMI = 18.5-24.9
- Overweight: BMI = 25-29.9
- Obese: BMI ≥ 30
These groups help spot health risks and suggest weight management plans.
Limitations of BMI
BMI is useful but has its downsides. It doesn’t measure body fat or muscle. So, athletes or those with a lot of muscle might have a high BMI without being obese. Also, BMI might not be right for older adults or some ethnic groups because of body composition differences.
Even with its flaws, BMI is a key first step in health evaluation processes. It points out who needs more health checks and lifestyle changes. When paired with other health metrics, BMI offers a full view of health. It helps doctors and patients make better lifestyle considerations assessed during health talks.
Benefits of Weight Loss
Weight loss brings many health benefits, from better physical health to improved mental well-being. It’s clear that good weight management strategies are key to these gains.
Physical Health Improvements
Losing weight can greatly improve physical health. This includes:
- Reduced risk of chronic diseases: Losing weight can lower the risk of type 2 diabetes, high blood pressure, and some cancers.
- Improved cardiovascular health: Losing weight can lower blood pressure and improve heart health.
- Enhanced mobility and flexibility: Losing weight can make joints healthier and reduce mobility problems.
A study in the Journal of the American Medical Association (JAMA) found that weight loss in obese people can greatly improve heart health. This includes better blood pressure and lipid profiles.
“Weight loss is a critical component of the treatment plan for obesity-related comorbidities.”
Health Benefit | Description |
Reduced Risk of Chronic Diseases | Weight loss decreases the risk of developing type 2 diabetes, hypertension, and certain cancers. |
Improved Cardiovascular Health | Weight loss lowers blood pressure, improves lipid profiles, and reduces heart disease risk. |
Enhanced Mobility and Flexibility | Weight loss improves joint health and reduces mobility-related disorders. |
Psychological Benefits
Weight loss also greatly improves mental health. Good weight management strategies can lead to:
- Improved self-esteem and body image: A healthier weight can boost confidence and self-image.
- Reduced stress and anxiety: Losing weight can lower stress and anxiety, improving mental health.
- Enhanced overall quality of life: Losing weight can make life better, allowing for more enjoyable activities.
We stress the importance of lifestyle considerations assessed during weight loss. Healthy habits and sustainable strategies are key to enjoying these mental benefits.
Criteria for Bariatric Candidates
To decide if someone is right for bariatric surgery, we look at many things. We check their health and lifestyle to make sure they’re a good fit for the surgery.
Medical Assessments
Checking a patient’s health is key to seeing if they can have bariatric surgery. We look at their BMI, overall health, and past health issues. This helps us see if there are any risks and if they’re ready for surgery.
Lifestyle Considerations
How someone lives their life also matters a lot. We check their eating habits, how active they are, and if they’re ready to change their lifestyle for good. These things help make sure they’ll do well after surgery.
Criteria | Description | Importance |
BMI | Body Mass Index calculation | High |
Previous Medical Conditions | History of chronic diseases | High |
Dietary Habits | Eating habits and food choices | Medium |
Physical Activity Level | Regularity and intensity of exercise | Medium |
Psychological Evaluation | Mental health and readiness for surgery | High |
Looking at both health and lifestyle helps us decide if someone is right for bariatric surgery. This careful look makes sure patients get the best care and support on their weight loss journey.
Post-Surgery Weight Management
Managing weight after surgery is key to lasting weight loss. After bariatric surgery, patients must make big lifestyle changes. This ensures the best results.
Importance of Follow-Up Care
Follow-up care is vital for managing weight after surgery. Regular visits with healthcare providers are important. They help track progress and address any issues.
Follow-up appointments include weight checks, nutrition advice, and health assessments. These visits help adjust care plans to keep patients on track with their weight loss goals.
During these visits, healthcare providers do several things:
- Monitor weight loss progress
- Check for nutritional deficiencies
- Address any concerns or complications
- Offer guidance on a healthy lifestyle
Long-term Lifestyle Changes
Long-term lifestyle changes are essential for lasting weight loss. This means changing diet, increasing exercise, and managing stress. Patients must be ready to make these changes to reach and keep their weight loss goals.
Some important strategies for long-term weight management include:
- Eating a balanced diet rich in nutrients
- Doing regular physical activity, like walking or swimming
- Staying hydrated and controlling portion sizes
- Getting support from healthcare providers, support groups, or loved ones
Combining follow-up care with long-term lifestyle changes leads to significant and lasting weight loss. Our team is committed to supporting patients throughout their journey. We help them overcome challenges and celebrate their victories.
Support Systems for Bariatric Patients
A strong support system is key for bariatric patients to reach their weight loss goals. The journey to success is not just about the surgery. It also involves a network that covers physical, emotional, and nutritional needs.
We focus on a support system that includes emotional groups and nutrition counseling. These elements help bariatric patients get the tools they need for long-term success.
Emotional Support Groups
Emotional support groups are essential for bariatric patients. They offer a safe place to share experiences and challenges. This way, patients can develop coping strategies and build confidence.
Our groups are led by experts in bariatric care. They talk about stress management, body image, and staying motivated. Patients get insights and support from those who understand their journey.
Nutrition Counseling
Nutrition counseling is vital for bariatric patients. Our team creates personalized meal plans to support weight loss. They work with patients to meet their nutritional needs.
Good nutrition counseling does more than give dietary advice. It teaches healthy eating habits and meal planning. We also help with common nutritional challenges after surgery.
Key Components of Nutrition Counseling:
- Personalized meal planning
- Nutritional education
- Guidance on managing nutritional challenges
- Ongoing support and monitoring
We also do a support system evaluation to find where more support is needed. This helps us tailor our services to each patient’s unique needs.
We emphasize the importance of consultation with specialists too. Our team works with psychologists, nutritionists, and surgeons for complete care.
Support System Component | Description | Benefits |
Emotional Support Groups | Led by experienced professionals, these groups provide a safe space for sharing experiences and challenges. | Coping strategies, confidence building, sense of community |
Nutrition Counseling | Personalized meal planning and nutritional education. | Healthy eating habits, managing nutritional challenges |
Consultation with Specialists | Collaboration with healthcare professionals to provide complete care. | Multidisciplinary support, tailored care |
Innovative Approaches to Weight Management
New ways to manage weight are changing bariatric care. We’re moving towards more holistic and patient-focused methods.
Non-surgical weight loss options are a big step forward. They’re great for those who can’t or don’t want surgery.
Non-Surgical Weight Loss Options
Non-surgical weight loss is getting better. Some top options include:
- Prescription Medications: New meds help control hunger and fullness.
- Endoscopic Procedures: Small procedures can change stomach size or digestion.
- Lifestyle Interventions: Programs with diet advice, exercise plans, and therapy.
Technological Advances in Bariatric Care
Technology is key in improving bariatric care. Some major advances are:
- Telehealth Services: Remote care and support.
- Mobile Health Applications: Apps track diet, exercise, and health.
- Advanced Diagnostic Tools: New tools for better health checks and weight tracking.
These new methods are making weight management better. They also improve care quality for bariatric patients. By using the latest in non-surgical options and tech, we offer more tailored and effective support.
Future Trends in Bariatric Weight Classification
The field of bariatric care is growing fast. We’re seeing new ways to treat obesity and manage weight. Research and development are key in shaping the future of how we classify bariatric weight.
Advancements in Obesity Treatment
Studies are working on better, more tailored treatments. We’re moving towards more detailed approaches. These consider personal factors that affect weight loss and health.
Policy Impact on Weight Management
Policy choices, like insurance coverage, will change how we access weight management programs. Good policy-making is vital. It ensures bariatric care is available to those who need it.
Understanding the link between research, policy, and insurance helps us tackle the challenges of bariatric weight classification. This way, we can offer better support to our patients.
FAQ
What is bariatric weight classification, and why is it important?
Bariatric weight classification sorts people by their weight and BMI. It helps decide if someone can have weight loss surgery. It also shows the health risks involved.
How is BMI used in bariatric weight classification?
BMI is a way to measure weight against height. It helps figure out who needs bariatric surgery. A higher BMI means more obesity.
What are the different types of obesity, and how are they classified?
Obesity is divided into three classes: Class I, II, and III. Class I has a BMI of 30-34.9. Class II is 35-39.9, and Class III is 40 or higher.
What are the eligibility criteria for bariatric surgery?
To get bariatric surgery, you need a BMI of 40 or higher. Or a BMI of 35 with obesity-related health issues. You also need a full health check and lifestyle review.
What is the role of follow-up care in post-surgery weight management?
After surgery, follow-up care is key. It helps keep weight off and deals with any problems. You’ll see doctors regularly and get advice on diet and lifestyle.
How can patients access support systems after bariatric surgery?
There are many ways to get support after surgery. You can join emotional support groups or get nutrition advice. These help you stay on track and succeed in the long run.
What are the benefits of weight loss for overall health?
Losing weight can greatly improve your health. It lowers the risk of chronic diseases and boosts your mood and well-being.
What are the limitations of relying solely on BMI as a health metric?
BMI is useful but has its limits. It doesn’t consider muscle or body fat. So, it’s best to use it with other health measures for a full picture.
What are the different types of bariatric surgery available?
There are several bariatric surgeries, like gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Each has its own benefits. The right one depends on your health and needs.
How do insurance coverage factors influence access to bariatric surgery?
Insurance can affect who gets bariatric surgery. Some plans have rules or limits. It’s important to check your policy to understand what’s covered.
What are the possible risks and complications of bariatric surgery?
Bariatric surgery can have risks, like bleeding or infection. It can also lead to nutritional problems. Talk to your doctor about these risks and benefits.
What are the future trends in bariatric weight classification and obesity treatment?
Bariatric care is always changing. New treatments and techniques are being developed. Policy changes and technology will also shape the future of obesity treatment.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery/potential-candidates