What is the biggest cause of ovarian cancer? Ovarian cancer is often found late, making it hard to treat. Understanding the risk factors is key for early detection and prevention. Actress Kathy Bates’ battle with ovarian and breast cancer shows the personal toll of these diseases.
We will look into the main causes and risk factors of ovarian cancer. This includes genetic predisposition, hormonal influences, and lifestyle factors. Knowing these can help us understand and tackle this disease better.

Key Takeaways
- Genetic mutations play a significant role in ovarian cancer risk.
- Family history is a key factor in determining risk.
- Hormonal influences can impact ovarian cancer development.
- Lifestyle factors contribute to the overall risk profile.
- Early detection is critical for effective treatment.
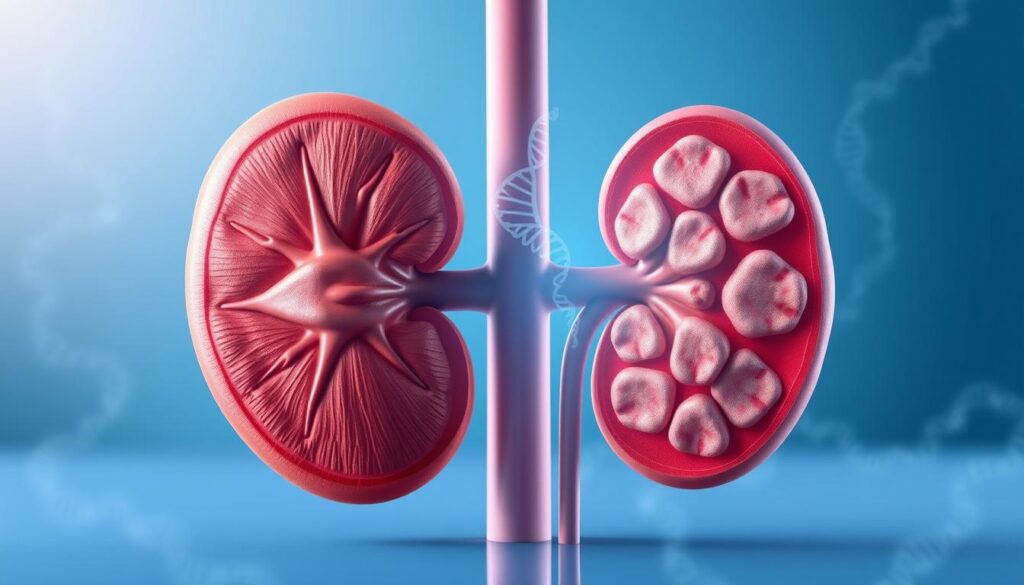
The Nature and Impact of Ovarian Cancer
It’s key to know about ovarian cancer to catch it early and treat it well. This cancer grows out of control in the ovaries. If not treated fast, it can cause serious health problems.
What Happens in Ovarian Cancer
Ovarian cancer messes up normal cell growth, creating tumors. These tumors can spread, making treatment harder. The disease often starts quietly, with symptoms that are hard to spot early.
Key aspects of ovarian cancer include:
- Uncontrolled cell growth in the ovaries
- Potential for late-stage diagnosis due to nonspecific symptoms
- Spread of cancer to other parts of the body
Prevalence and Mortality Rates in the United States
Ovarian cancer is a big worry in the U.S., with high rates of occurrence and death. It’s one of the top five gynecologic cancers in death rates. Every year, it affects thousands of women, touching their families and communities deeply.
The prevalence and mortality rates show we need to spread awareness and find ways to catch it early. Some important stats are:
- Ovarian cancer is the fifth leading cause of death among women in the U.S.
- The chance of getting ovarian cancer in a lifetime is about 1 in 78 for women.
- Early ovarian cancer often has no symptoms, leading to late diagnosis.
Understanding ovarian cancer helps us see why we must keep researching its causes and find better ways to screen and treat it.
Genetic Predisposition: The Primary Cause of Ovarian Cancer
Genetic predispositions play a big role in ovarian cancer risk. Mutations in the BRCA1 and BRCA2 genes are key risk factors. Genetic testing is vital for those at high risk.
BRCA1 Mutations and Their Impact
BRCA1 mutations raise the risk of ovarian cancer a lot. Women with this mutation face a higher chance of getting ovarian cancer. The cancer can also be more aggressive.
It’s important to know about BRCA1 mutations to manage risk. This includes talking about preventive steps and more frequent check-ups.
BRCA2 Mutations and Associated Risks
BRCA2 mutations also increase ovarian cancer risk, but less than BRCA1. People with BRCA2 should know their risk is higher. They should talk to their doctor about managing it.
Having either BRCA1 or BRCA2 mutation means a detailed risk plan is needed. This might include genetic counseling and testing for family members.
Genetic Testing and Risk Assessment
Testing for BRCA1 and BRCA2 mutations helps figure out ovarian cancer risk. It lets doctors offer better screening and prevention. This could lower the risk of ovarian cancer.
For those with a family history of ovarian or breast cancer, genetic testing is key. It’s important to talk to a genetic counselor. They can explain what the test results mean and how to manage risk.
Family History as a Critical Risk Factor
Having a close relative diagnosed with ovarian cancer can greatly increase a woman’s risk. This shows how vital it is to know about family history when it comes to ovarian cancer.
A family history of ovarian cancer, like in mothers, sisters, or daughters, is a big risk factor. When ovarian cancer is found in these close relatives, it makes a person’s risk much higher.
First-Degree Relatives with Ovarian Cancer
Research shows that women with a first-degree relative with ovarian cancer face a higher risk. This risk grows if more first-degree relatives have been diagnosed.
For example, if a woman has a mother or sister with ovarian cancer, her risk is two to three times higher than average. The exact risk depends on how many relatives are affected and their age at diagnosis.
Hereditary Cancer Syndromes Beyond BRCA
There are more than just BRCA1 and BRCA2 gene mutations that raise ovarian cancer risk. Lynch syndrome, or hereditary nonpolyposis colorectal cancer (HNPCC), is another example.
Lynch syndrome is caused by mutations in genes like MLH1, MSH2, MSH6, and PMS2. People with Lynch syndromeface a higher risk of several cancers, including ovarian cancer.
It’s important to understand these hereditary cancer syndromes to assess ovarian cancer risk. Genetic testing and counseling can help find those at higher risk.
By recognizing the role of family history and hereditary cancer syndromes, we can spot those at higher risk for ovarian cancer. This allows us to offer the right preventive and surveillance steps.
Ovarian Cancer Causes: The Incessant Ovulation Theory
The incessant ovulation theory suggests that how often a woman ovulates might affect her risk of ovarian cancer. It proposes that ovulating too often without enough time to recover could increase this risk.
To grasp this theory, we must look at how ovulation impacts the ovaries. Each ovulation, the ovarian surface breaks to release an egg. Then, the ovaries repair themselves, which involves cell growth.
How Ovulation Damages Ovarian Tissue
Ovulation and repair can cause genetic harm to the ovarian surface cells. Repeated ovulation without enough breaks can build up this damage. This might lead to cancerous changes.
Studies indicate that women with more ovulatory cycles in their lives face a higher ovarian cancer risk. Early menarche, late menopause, and never having children are factors that increase ovulation frequency.
Factors That Interrupt Ovulation and Reduce Risk
On the other hand, things that stop ovulation can lower ovarian cancer risk. Pregnancy and breastfeeding are key examples, as they stop ovulation for a long time. Women who have been pregnant or breastfed have a lower risk of ovarian cancer.
Other things that can lower ovulation frequency include using birth control pills. Research shows that using birth control pills can greatly lower ovarian cancer risk. The more you use them, the more protection you get.
Understanding the incessant ovulation theory helps identify women at higher risk. It also guides preventive measures. By knowing what affects ovulation frequency and ovarian cancer risk, doctors can give better advice and help.
Hormonal Influences on Ovarian Cancer Development
It’s important to know how hormones affect ovarian cancer. Hormones play a big role in this disease. Research has shown how these hormones increase the risk.
Estrogen Exposure Throughout Life
Estrogen is key in ovarian cancer. The more estrogen a woman is exposed to, the higher her risk. This can come from her body or from hormone therapy.
- Early onset of menstruation
- Late menopause
- Hormone replacement therapy
Hormone Replacement Therapy Considerations
Hormone therapy (HRT) can raise ovarian cancer risk. Studies show estrogen-only therapy increases this risk. But, the risk depends on many factors, like the type of therapy and how long it’s used.
Women and their doctors need to think about the benefits and risks of HRT. They should consider their own risk for ovarian cancer.
Birth Control Pills and Risk Reduction
Birth control pills can lower ovarian cancer risk. They work by stopping ovulation, which reduces genetic mutations that can cause cancer. The longer a woman uses them, the more her risk goes down.
Benefits of Birth Control Pills:
- Reduced risk of ovarian cancer
- Protection against other reproductive cancers
- Regulation of menstrual cycles
Knowing how hormones affect ovarian cancer helps women make better health choices. This includes deciding on hormone therapy and birth control pills. It’s vital to talk to a doctor about these choices based on individual risks.
Reproductive History and Ovarian Cancer Risk
Research shows that reproductive history can greatly affect a woman’s chance of getting ovarian cancer. We’ll look at how pregnancy, childbirth, and breastfeeding impact this risk.
Pregnancy’s Protective Effect
Pregnancy lowers the risk of ovarian cancer. Studies show that each full-term pregnancy reduces the risk. This is due to changes in the ovaries and hormonal effects that may cut down on ovulations.
The risk drop is significant. Women with multiple pregnancies might have a 50% lower risk than those who never got pregnant.
Never Having Children as a Risk Factor
Women who never had children face a higher risk of ovarian cancer. This is linked to the incessant ovulation theory. Uninterrupted ovulation over a lifetime may cause more genetic errors in the ovaries, leading to cancer.
The “incessant ovulation” hypothesis says the more a woman ovulates, the higher her cancer risk. Pregnancy and breastfeeding, which stop ovulation, may protect against cancer.
Breastfeeding and Risk Reduction
Breastfeeding also lowers the risk of ovarian cancer. Longer breastfeeding periods are linked to greater risk reduction. This is thought to be due to ovulation suppression and hormonal changes.
The link between reproductive history and ovarian cancer risk is complex. Knowing these factors can help spot women at higher risk. This knowledge can guide preventive measures.
| Reproductive Factor | Effect on Ovarian Cancer Risk |
| Pregnancy | Reduces risk, with greater reduction with multiple pregnancies |
| Never having children | Increases risk |
| Breastfeeding | Reduces risk, with longer durations giving more protection |
Age-Related Risk Factors
Ovarian cancer risk increases with age, affecting post-menopausal women the most. As we get older, our bodies undergo changes that raise the risk of ovarian cancer.
Why Ovarian Cancer Risk Increases with Age
Ovarian cancer is more common in older women, with most cases found in women over 50. The American Cancer Society reports that over half of ovarian cancer cases are in women aged 63 or older. This increase is due to hormonal, genetic, and environmental factors.
As women age, their ovaries are more likely to develop genetic mutations, which can lead to cancer. Also, the buildup of estrogen over a lifetime may play a role in increasing risk.
Post-Menopausal Vulnerability
Post-menopausal women face a higher risk of ovarian cancer due to hormonal changes. After menopause, estrogen and progesterone levels drop, affecting the ovaries and possibly raising cancer risk.
These women are also more likely to have other health issues that can make diagnosing and treating ovarian cancer harder. It’s important for them to be aware of their risk and talk to their healthcare provider about any concerns.
We suggest that women over 50 stay informed about their ovarian cancer risk. Regular check-ups can help in early detection and understanding age-related risk factors, improving outcomes.
Menstrual History and Ovarian Cancer
Menstrual history is key in figuring out ovarian cancer risk. It’s influenced by when you start and stop menstruating. We look into how these times can affect a woman’s chance of getting ovarian cancer.
Early Menstruation as a Risk Factor
Starting your period early, before 12, raises your risk of ovarian cancer. This is because you’re exposed to estrogen longer. Estrogen can help tumors grow in the ovaries.
Key factors associated with early menarche include:
- Earlier age of first menstrual period
- Increased lifetime estrogen exposure
- Potential genetic predispositions
Late Menopause and Extended Ovulation
Starting your period late, after 55, also ups your risk of ovarian cancer. This is because you’re ovulating more. The incessant ovulation theory says this can damage the ovaries, leading to cancer.
| Menstrual History Factor | Impact on Ovarian Cancer Risk |
| Early Menarche (<12 years) | Increased risk due to longer estrogen exposure |
| Late Menopause (>55 years) | Increased risk due to prolonged ovulation |
Knowing these factors can help figure out your risk. Women with early or late periods should talk to their doctor about it.
Endometriosis and Its Connection to Ovarian Cancer
There’s a strong link between endometriosis and ovarian cancer, a key area in women’s health. Endometriosis is when endometrial tissue grows outside the uterus, affecting millions. Studies show it raises the risk of ovarian cancer.
The Biological Link Between These Conditions
Research shows endometriosis’ biology might lead to ovarian cancer. Chronic inflammation in endometriosis could cause genetic changes in the ovaries, starting cancer. “The chronic inflammatory environment in endometriosis may create a fertile ground for tumorigenesis,” a study found.
The incessant ovulation theory also plays a part. It says repeated ovulation damages the ovaries. Women with endometriosis often have irregular ovulation, raising their risk.
Managing Endometriosis to Potentially Reduce Cancer Risk
Managing endometriosis well is key for symptom relief and cancer risk reduction. Treatments include hormonal therapies and surgery. “Early diagnosis and treatment of endometriosis are essential for improving the quality of life for these women and may also have implications for cancer prevention,” experts say.
Strategies for managing endometriosis include:
- Hormonal treatments to reduce menstrual flow and alleviate symptoms
- Surgical options, such as laparoscopic surgery, to remove endometrial lesions
- Lifestyle modifications, including dietary changes and exercise, to manage symptoms
Understanding the link between endometriosis and ovarian cancer helps healthcare providers. They can offer better care to women with endometriosis, potentially lowering their cancer risk.
Infertility and Treatment-Related Risks
There’s a lot of research on how infertility, fertility treatments, and ovarian cancer are connected. We need to know about the health issues that might lead to infertility and cancer. We also need to understand how fertility treatments could affect ovarian cancer risk.
Underlying Conditions Causing Both Infertility and Cancer Risk
Some health problems can make you more likely to have infertility and ovarian cancer. For example, endometriosis can cause infertility and might raise your risk of ovarian cancer. Polycystic ovary syndrome (PCOS), which often causes infertility, might also increase ovarian cancer risk, but more research is needed.
It’s key to understand these health issues. They might make it harder to see if fertility treatments increase cancer risk. Women with these conditions might already have a higher risk of ovarian cancer.
Fertility Treatments and Possible Ovarian Cancer Links
Fertility treatments like ovulation induction and in vitro fertilization (IVF) have been studied for their possible link to ovarian cancer. Some research suggests that certain fertility drugs might raise cancer risk. This could be because they stimulate the ovaries, possibly leading to cancer.
But, the research isn’t clear yet. Some studies say the risk might be higher for women who have many treatments or have fertility problems. It’s also important to remember that the overall risk is low. The benefits of these treatments often outweigh the risks.
As we keep looking into the link between fertility treatments and ovarian cancer, it’s vital for women to talk to their doctors. They should understand their own risk factors, the treatments they’re getting, and any health conditions that might affect their cancer risk.
Lifestyle Factors Influencing Ovarian Cancer Risk
Research shows that lifestyle choices can affect ovarian cancer risk. By changing our daily habits, we might lower our risk. This is important to understand.
Obesity and Its Mechanisms in Cancer Development
Obesity is linked to a higher risk of ovarian cancer. The reasons are complex. Chronic inflammation and hormonal changes from obesity play a role. A study published in a medical journal showed that obesity increases ovarian cancer risk, mainly in women with a BMI of 30 or higher.
“Obesity is a modifiable risk factor, and understanding its impact on ovarian cancer risk can inform strategies for prevention.”
Keeping a healthy weight is key. It lowers ovarian cancer risk and helps avoid other obesity-related health problems.
Dietary Patterns and Their Impact
Studies have looked into how diet affects ovarian cancer risk. Eating lots of vegetables, fruits, and whole grains can help. But, a diet full of processed foods and red meat might raise the risk. The exact reasons are not clear, but diet can affect hormones and inflammation, which are important in cancer development.
A study in the American Journal of Clinical Nutrition found that a Mediterranean diet can lower ovarian cancer risk. This diet includes lots of fruits, vegetables, and healthy fats.
Physical Activity as a Protective Factor
Regular exercise is good for many reasons, including lowering ovarian cancer risk. It can affect hormone levels, improve insulin sensitivity, and reduce inflammation. All these factors might help lower cancer risk.
- Engaging in at least 30 minutes of moderate-intensity exercise per day
- Incorporating strength training to improve overall health
- Aiming for a variety of physical activities to maintain long-term adherence
By living a lifestyle that includes exercise, a balanced diet, and a healthy weight, we can lower our risk of ovarian cancer.
Environmental Risk Factors for Ovarian Cancer
Some environmental factors might increase the risk of ovarian cancer. Our surroundings and lifestyle choices can affect our risk. It’s important to understand this connection.
Occupational Exposures and Hazards
Certain jobs may raise the risk of ovarian cancer. Women in jobs with asbestos, talc, or certain chemicals might be at higher risk. We should know about these dangers and take steps to avoid them.
Jobs in manufacturing or agriculture might also increase the risk. While the evidence is not solid, it’s key for those in these jobs to talk to their doctors about the risks.
Environmental Pollutants and Their Effects
Environmental pollutants, like endocrine-disrupting chemicals (EDCs), are linked to health problems, including cancer. They can mess with our hormones, possibly leading to ovarian cancer.
EDCs are found in plastics, pesticides, and industrial chemicals. Cutting down on these pollutants is vital. We can do this by changing our lifestyle and pushing for cleaner environments.
Being careful about the products we use and the places we go is important. Making smart choices and supporting clean environments can help lower ovarian cancer risk.
Preventive Strategies Against Ovarian Cancer
Preventing ovarian cancer involves surgery, medicine, and lifestyle changes. These steps are based on a woman’s risk level. For those at high risk, knowing these strategies is key.
Prophylactic Surgery for High-Risk Women
Women with BRCA1 or BRCA2 mutations can greatly lower their risk. They can do this by having their ovaries and fallopian tubes removed. This surgery is very effective in preventing ovarian cancer.
A study in the Journal of Clinical Oncology showed a big drop in ovarian cancer risk. High-risk women saw their risk fall by up to 80% after this surgery.
| Risk Factor | Prophylactic Surgery Benefit |
| BRCA1 Mutation | Up to 80% risk reduction |
| BRCA2 Mutation | Up to 80% risk reduction |
| Family History | Significant risk reduction, exact percentage varies based on individual risk factors |
Chemoprevention Options
Chemoprevention uses medicines to lower cancer risk. Oral contraceptives are one example. They help lower ovarian cancer risk, with longer use providing more protection.
A study in the Lancet found a 27% drop in ovarian cancer risk. This was for women who had ever used oral contraceptives. Longer use led to even more protection.
Lifestyle Modifications for Risk Reduction
Lifestyle changes can also help lower ovarian cancer risk. Staying at a healthy weight, exercising regularly, and eating well are good choices.
By making these lifestyle changes, women at high risk can lower their chance of getting ovarian cancer.
Early Detection and Management of Ovarian Cancer Risk
Managing ovarian cancer risk is about being aware, getting screened, and talking to a genetic counselor. Early detection is vital for better survival rates and treatment results.
Current Screening Recommendations
There’s no single, reliable test for ovarian cancer for everyone. But, those at high risk might find:
- Transvaginal ultrasound (TVUS)
- CA-125 blood test
These tests can spot ovarian cancer early, but they’re not perfect. The American Cancer Society says women at high risk should talk to their doctor about these options.
Recognizing Warning Signs and Symptoms
Ovarian cancer symptoms are often hard to spot early. Common signs include:
- Bloating or swelling in the abdomen
- Pelvic pain or pressure
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
Women should know these symptoms and see a doctor if they don’t go away.
When to Consult a Genetic Counselor
If you have a family history of ovarian or breast cancer, see a genetic counselor. They can help understand your risk. They’ll decide if genetic testing is right for you.
Some reasons to see a genetic counselor include:
- A family history of BRCA1 or BRCA2 mutations
- Multiple relatives with ovarian or breast cancer
- Being diagnosed with breast cancer at a young age
Knowing your risk helps you make smart health choices. This might include preventive steps.
Conclusion
Ovarian cancer is a complex disease with many causes. These include genetic predisposition, hormonal influences, lifestyle choices, and environmental exposures. We’ve looked at the various causes and risk factors for ovarian cancer. This highlights the need to understand these factors for prevention and early detection.
Genetic mutations like BRCA1 and BRCA2 play a big role. Family history also matters. Knowing about hormonal and reproductive factors, and lifestyle choices, helps assess risk. Prevention involves awareness, risk assessment, and taking proactive steps like lifestyle changes and sometimes surgery.
It’s vital to keep researching and educating about ovarian cancer. This will help us improve prevention and outcomes for those affected.
FAQ
What are the primary causes of ovarian cancer?
Ovarian cancer is caused by many factors. Genetics, lifestyle, and the environment play a role. BRCA1 and BRCA2 mutations are key genetic risks.
How does family history impact ovarian cancer risk?
A family history of ovarian cancer raises your risk. This is true, even more so if it’s in first-degree relatives. BRCA1 and BRCA2 mutations add to this risk.
What is the incessant ovulation theory, and how does it relate to ovarian cancer?
The incessant ovulation theory says repeated ovulation without rest may lead to ovarian cancer. Pregnancy and breastfeeding can lower this risk by interrupting ovulation.
How do hormonal factors influence ovarian cancer risk?
Hormones like estrogen can affect ovarian cancer risk. Hormone replacement therapy is a concern. But, birth control pills might help lower this risk.
What role does reproductive history play in determining ovarian cancer risk?
Reproductive history is important. Pregnancy and breastfeeding protect against ovarian cancer. Never having children, though, increases the risk.
How does age impact ovarian cancer risk?
Age is a big risk factor. Most ovarian cancer cases are found in post-menopausal women. As you get older, your risk goes up.
What is the connection between endometriosis and ovarian cancer?
Endometriosis, where endometrial tissue grows outside the uterus, raises ovarian cancer risk. Managing endometriosis might lower this risk.
Do infertility and its treatments increase ovarian cancer risk?
Infertility and its treatments might raise cancer risk. But, the link between fertility treatments and ovarian cancer is not fully understood yet.
How do lifestyle factors influence ovarian cancer risk?
Lifestyle choices, like obesity, diet, and exercise, can affect ovarian cancer risk. Making healthy lifestyle choices can help reduce risk.
Can environmental exposures contribute to ovarian cancer risk?
Yes, environmental factors like work hazards and pollutants can increase ovarian cancer risk. It’s important to avoid these exposures.
What preventive strategies are available for women at high risk of ovarian cancer?
Preventive steps include surgery, medication, and lifestyle changes. These can help lower ovarian cancer risk.
How can ovarian cancer be detected early?
Early detection is hard because symptoms are not specific. Screening, recognizing symptoms, and genetic counseling can help find cancer early.
What is the significance of genetic testing for ovarian cancer risk?
Genetic testing is key for finding BRCA1 and BRCA2 mutations. This allows for early action and risk reduction.
How does Lynch syndrome impact ovarian cancer risk?
Lynch syndrome, a hereditary condition, raises ovarian cancer risk. It’s important for those at high risk to understand this.