Bilateral optic neuritis is a serious eye condition that affects both eyes at once. It’s a big challenge in eye health. At Liv Hospital, we know how fast we need to act to save your vision.Our critical guide to bilateral optic neuritis covers the serious symptoms, key diagnostic steps, and essential treatment options.
Prompt intervention is key in treating this condition. It can cause sudden blindness. The usual treatment is intravenous methylprednisolone (IVMP). This shows how important it is to find out what’s causing it quickly.
We know that things like neuromyelitis optica spectrum disorders or vasculitis might be the cause. So, we do a detailed check to find out.
Key Takeaways
- Rapid diagnosis is critical for preserving vision in bilateral optic neuritis.
- IVMP is the standard treatment for managing the condition.
- Underlying causes such as neuromyelitis optica spectrum disorders or vasculitis must be considered.
- Comprehensive diagnostic evaluation is essential for determining the appropriate treatment plan.
- Timely intervention can significantly impact patient outcomes.
Understanding Bilateral Optic Neuritis

Bilateral optic neuritis is a serious condition where both optic nerves get inflamed. This can cause vision loss. We will dive into the details of this condition to help you understand its effects.
Definition and Pathophysiology
Bilateral optic neuritis happens when both optic nerves get inflamed at the same time. It can be caused by diseases that damage the myelin sheath, infections, or autoimmune disorders. The pathophysiology is when the immune system attacks the myelin sheath, causing inflammation and damage.
This inflammation stops the normal flow of visual signals from the eye to the brain. Symptoms include vision loss, eye pain, and blurry vision. Knowing the cause is key to managing the condition.
Prevalence and Epidemiology
About 21.7 to 29.3 percent of optic neuritis cases involve both eyes. The rate of new cases is between 0.56 and 5.1 cases per 100,000 each year. Women are more likely to get it, with a ratio of 2:1 female to male.
It mainly hits young adults, between 20 to 40 years. Caucasians are also more likely to be affected, showing a racial trend.
Important factors include:
- Age: 20 to 40 years
- Sex: Female predominance (2:1 ratio)
- Race: More common in Caucasians
Knowing these factors helps in early diagnosis and treatment.
Clinical Presentation of Bilateral Optic Neuritis

Understanding bilateral optic neuritis is key for correct diagnosis and treatment. Patients often show symptoms that affect their vision greatly.
Common Symptoms
Common symptoms include vision loss in both eyes and pain around the eyes. These symptoms can get worse with eye movement. They may also change over time.
Vision loss can be mild or severe. Periocular pain gets worse with eye movement. Dyschromatopsia makes it hard to see colors.
Symptom | Characteristics | Impact on Patients |
Vision Loss | Variable, ranging from mild to severe | Affects daily activities, such as reading and driving |
Periocular Pain | Worsens with eye movement | Causes discomfort and pain around the eyes |
Dyschromatopsia | Reduced color vision | Makes distinguishing colors difficult |
Distinguishing Features from Unilateral Cases
Bilateral optic neuritis affects both eyes at once. This can lead to more severe vision loss. It might also mean a more serious condition.
This condition could be linked to diseases like multiple sclerosis. So, a detailed check-up is needed to find the cause.
Red Flags in Presentation
Some signs need quick attention. These include severe vision loss and symptoms that get worse fast. Also, look out for fever or headache.
Spotting these signs early is vital. It helps in quick treatment and prevents more vision loss. It also helps find any underlying issues.
Etiologies of Bilateral Optic Neuritis
It’s important to know what causes bilateral optic neuritis to treat it well. This condition can come from many sources, each needing its own care plan.
Demyelinating Disorders
Demyelinating disorders are a big reason for bilateral optic neuritis. Multiple sclerosis (MS) and neuromyelitis optica spectrum disorder (NMOSD) are two main conditions linked to it.
MS is a chronic disease where the body attacks the central nervous system. It often starts with one optic nerve but can affect both.
NMOSD mainly hits the optic nerves and spinal cord. It’s more likely to cause both optic nerves to be affected.
Demyelinating Disorder | Characteristics | Association with Bilateral Optic Neuritis |
Multiple Sclerosis (MS) | Chronic autoimmune demyelination in the CNS | Less common than unilateral; can be a presenting feature |
Neuromyelitis Optica Spectrum Disorder (NMOSD) | Autoimmune condition affecting optic nerves and spinal cord | More frequently associated with bilateral optic neuritis |
Inflammatory and Autoimmune Causes
Other causes of bilateral optic neuritis include inflammatory and autoimmune diseases. These include systemic lupus erythematosus (SLE), sarcoidosis, and other autoimmune disorders.
SLE is a disease that can harm many parts of the body, including the eyes. It can cause severe and bilateral optic neuritis.
Sarcoidosis can also lead to bilateral optic neuritis through inflammation.
Infectious and Post-Infectious Causes
Infections and conditions after infections are also causes of bilateral optic neuritis. Some infections can directly or indirectly cause optic neuritis.
Viral infections like measles and mumps, and bacterial infections, are examples. Post-infectious optic neuritis happens when the body’s immune system reacts to an infection.
In conclusion, bilateral optic neuritis can come from many causes. These include demyelinating disorders, inflammatory and autoimmune diseases, and infections. Knowing these causes helps doctors diagnose and treat the condition properly.
Differential Diagnosis in Bilateral Optic Neuritis
Bilateral optic neuritis is a tough diagnosis. We need to look at many possible causes to find the right one. This helps us treat the patient well.
Toxic and Nutritional Optic Neuropathies
Toxic and nutritional optic neuropathies can look like bilateral optic neuritis. These happen from toxins or not getting enough nutrients. For example, tobacco-alcohol amblyopia damages the optic nerve from drinking and smoking a lot.
It’s important to know if the patient has been exposed to toxins or lacks nutrients. Vitamin B12 deficiency can cause optic neuropathy. Taking more vitamin B12 can help.
Compressive Optic Neuropathies
Compressive optic neuropathies happen when something presses on the optic nerve. This can cause vision loss. Tumors like optic nerve gliomas or meningiomas can do this.
Cause | Characteristics |
Tumors (e.g., optic nerve gliomas, meningiomas) | Progressive visual loss, potentially with proptosis or other signs of orbital involvement |
Aneurysms or other vascular lesions | Variable presentation, potentially with acute visual loss or cranial nerve palsies |
Hereditary Optic Neuropathies
Hereditary optic neuropathies are genetic and affect the optic nerve. Leber’s hereditary optic neuropathy (LHON) is a common one. It usually hits young men.
“The diagnosis of hereditary optic neuropathies relies heavily on genetic testing and family history.”
Knowing the genetic cause helps us predict the outcome. It also helps with family counseling.
Comprehensive Diagnostic Approach for Bilateral Optic Neuritis
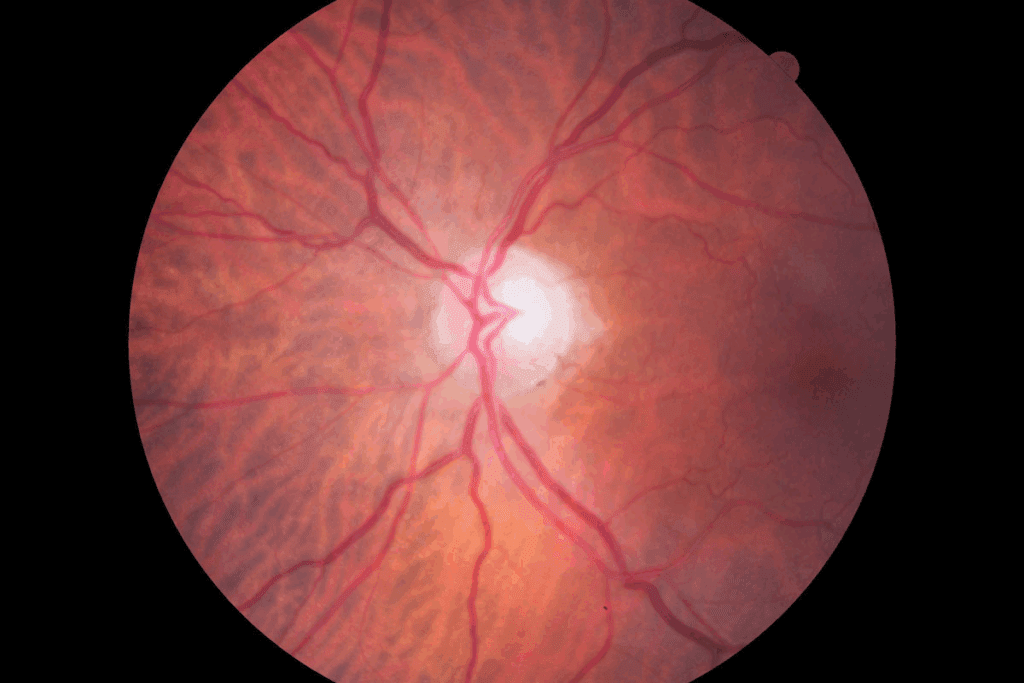
Accurately identifying bilateral optic neuritis requires a detailed diagnostic strategy. This involves several steps, including clinical exams, visual field tests, and advanced imaging like Optical Coherence Tomography (OCT).
Clinical Examination Techniques
Diagnosing bilateral optic neuritis starts with a thorough clinical exam. We check the patient’s vision, how their pupils react, and their color vision. A relative afferent pupillary defect (RAPD) can show if one optic nerve is affected more than the other.
Key components of the clinical examination include:
- Visual acuity testing
- Pupillary reaction assessment
- Color vision testing
- Ophthalmoscopy to examine the optic disc
Medical Expert, “A detailed clinical exam is key to diagnosing bilateral optic neuritis and distinguishing it from other vision problems.”
“The clinical presentation can vary significantly among patients, making a complete examination essential.”
Visual Field Testing
Visual field tests are also vital in diagnosing bilateral optic neuritis. They help us see how much vision is lost and how severe the optic nerve damage is.
Type of Visual Field Defect | Common Causes |
Central scotoma | Demyelinating disorders, toxic optic neuropathy |
Diffuse depression | Inflammatory, infectious causes |
Altitudinal defects | Ischemic optic neuropathy |
Visual field defects in bilateral optic neuritis can differ. Identifying these patterns helps narrow down possible causes.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) has greatly improved how we assess optic nerve and retinal issues. It gives detailed images of the retinal nerve fiber layer and ganglion cell layer, helping us measure optic nerve damage.
A recent study found, “OCT is now a critical tool in diagnosing and tracking optic neuritis. It offers insights into disease severity and how it progresses.” OCT findings can also relate to how well a patient sees and their overall prognosis.
By using clinical exams, visual field tests, and OCT together, we get a full picture of bilateral optic neuritis in each patient. This helps us choose the best treatment options.
Advanced Imaging in Diagnosis
Advanced imaging is key for diagnosing bilateral optic neuritis. These techniques help us see the optic nerves and the areas around them. They help spot inflammation and other issues.
MRI Protocol with Gadolinium Enhancement
MRI with gadolinium is a vital tool for diagnosing bilateral optic neuritis. It lets us see the optic nerves and find signs of inflammation. Gadolinium contrast makes these signs clearer.
Interpreting Neuroimaging Findings
We look for optic nerve enhancement on MRI scans. This enhancement means there’s inflammation. Finding this is a key sign of bilateral optic neuritis.
Differential Patterns in Various Etiologies
Each cause of bilateral optic neuritis shows different MRI patterns. For example, diseases like multiple sclerosis have specific brain lesions.
Etiology | MRI Findings |
Demyelinating Diseases (e.g., Multiple Sclerosis) | Lesions in the brain, optic nerve enhancement |
Inflammatory and Autoimmune Causes | Optic nerve enhancement, possible systemic involvement |
Infectious Causes | Variable findings, may include optic nerve enhancement and signs of infection |
Knowing these patterns is vital for correct diagnosis and treatment of bilateral optic neuritis.
Laboratory Investigations
To accurately diagnose bilateral optic neuritis, a thorough approach is needed. Laboratory tests are key to finding the cause and planning treatment.
Serological Testing
Serological tests are essential. They look for antibodies and proteins that show what’s causing the problem. These tests help us find signs of autoimmune diseases, infections, or other conditions.
Common serological tests include:
- Aquaporin-4 antibody test for Neuromyelitis Optica Spectrum Disorder (NMOSD)
- Myelin Oligodendrocyte Glycoprotein (MOG) antibody test
- Tests for systemic autoimmune diseases like Lupus or Sjögren’s syndrome
Cerebrospinal Fluid Analysis
Cerebrospinal fluid (CSF) analysis is also critical. We check the CSF for signs of inflammation, infection, or other issues that might be causing the optic neuritis.
Key components of CSF analysis include:
- Cell count and differential to identify inflammation or infection
- Protein and glucose levels to assess blood-CSF barrier integrity
- Oligoclonal band testing to detect intrathecal immunoglobulin synthesis
Additional Biomarkers
Other biomarkers can also offer important insights. These might include markers of inflammation, oxidative stress, or metabolic changes linked to bilateral optic neuritis.
Biomarker | Significance |
Aquaporin-4 antibodies | Indicative of NMOSD |
MOG antibodies | Associated with MOG-associated optic neuritis |
Oligoclonal bands | Suggestive of intrathecal inflammation, often seen in Multiple Sclerosis |
By combining the results of these tests, we can understand the cause of bilateral optic neuritis better. This helps us create a treatment plan that works.
Treatment Strategies for Bilateral Optic Neuritis
Managing bilateral optic neuritis needs a deep understanding of its causes and treatments. A good plan must tackle both the immediate symptoms and the root cause of the problem.
Acute Phase Management
In the early stages, our main goal is to lessen inflammation and help the body heal. We use high-dose corticosteroids as the first treatment. This includes intravenous methylprednisolone (IVMP) at 1 gram a day for 3 to 5 days, followed by oral prednisone.
The Optic Neuritis Treatment Trial showed IVMP can speed up recovery. But, it might not change the long-term vision much. So, we choose aggressive treatment for severe cases to improve recovery chances.
Etiology-Specific Treatments
After finding the cause, we tailor the treatment. For conditions like Multiple Sclerosis (MS), we use disease-modifying therapies (DMTs). These help prevent future attacks and slow the disease.
Etiology | Treatment Approach |
Demyelinating Disorders (e.g., MS) | Disease-Modifying Therapies (DMTs) |
Inflammatory/Autoimmune Causes | Immunosuppressive Therapy |
Infectious Causes | Antimicrobial Therapy |
Emerging Therapeutic Approaches
New research is looking into better treatments for bilateral optic neuritis. We’re studying plasma exchange for cases that don’t respond to steroids and intravenous immunoglobulin (IVIG) for autoimmune causes.
We’re also looking into neuroprotective agents and remyelinating therapies. These might help improve vision and prevent lasting damage.
Prognosis and Long-term Management
Understanding the prognosis and long-term management of bilateral optic neuritis is key. It’s important to know the cause to predict recovery and plan treatment.
Visual Recovery Expectations
How well a person recovers from bilateral optic neuritis depends on the cause. If it’s due to a condition like multiple sclerosis, recovery is often good. Many see big improvements in a few months.
Table: Visual Recovery Expectations Based on Etiology
Etiology | Visual Recovery Expectation |
Demyelinating Disorders | Generally good, with significant improvement within weeks to months |
Inflammatory and Autoimmune Causes | Variable, depending on the response to immunosuppressive therapy |
Infectious and Post-Infectious Causes | Generally improves with treatment of the underlying infection |
Preventing Relapses
Stopping relapses is a big part of managing the condition long-term. For those with multiple sclerosis or other autoimmune diseases, certain treatments can help a lot.
Visual Rehabilitation
Helping patients adjust to any lasting vision problems is important. This includes using low vision aids and occupational therapy.
Follow-up Protocol
Having a plan for follow-ups is vital. It helps keep track of the disease and makes sure treatments are working. Regular visits to eye doctors or neurologists are a must.
Conclusion
Diagnosing and treating bilateral optic neuritis needs a detailed plan. This plan includes looking at symptoms, causes, and using new tests. We’ve covered what bilateral optic neuritis is, its symptoms, causes, how to tell it apart from other conditions, and how to treat it.
Getting a diagnosis and starting treatment early is key. Knowing a lot about the condition helps doctors make good plans. This can help patients see better again and avoid getting sick again.
In short, treating bilateral optic neuritis needs a team effort. By using what doctors know and the latest technology, we can help patients a lot. This improves their life a lot.
FAQ
What is bilateral optic neuritis?
Bilateral optic neuritis is when both eyes get inflamed. This leads to vision loss and other eye problems.
What are the common symptoms of bilateral optic neuritis?
Symptoms include losing vision, blurry vision, eye pain, and light sensitivity. Other symptoms can also appear, depending on the cause.
How is bilateral optic neuritis diagnosed?
Doctors use many tests to diagnose it. These include eye exams, visual field tests, and MRI scans. They also check the blood and spinal fluid.
What are the causes of bilateral optic neuritis?
It can be caused by several things. These include Multiple Sclerosis, infections, and other diseases.
How is bilateral optic neuritis treated?
Treatment starts with steroids to manage the inflammation. Then, treatments are chosen based on the cause. New treatments are also being explored.
What is the prognosis for visual recovery in bilateral optic neuritis?
Recovery depends on the cause, how severe it is, and how quickly it’s treated. Some see big improvements, while others may not fully recover.
Can bilateral optic neuritis be prevented?
Not all cases can be prevented. But, managing health, avoiding infections, and staying healthy can lower the risk.
What is the role of MRI in diagnosing bilateral optic neuritis?
MRI scans are key in diagnosing it. They show the optic nerves and any inflammation. They also help find the cause, like demyelinating lesions.
How often should patients with bilateral optic neuritis follow up with their healthcare provider?
Follow-up visits depend on the cause, how severe it is, and how well it’s treated. Regular visits are important to check on vision, adjust treatment, and handle any issues.
Reference
Government Health Resource. Bilateral Optic Neuritis: Diagnosis and Prompt Intervention. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1805557